Abstract
Background:
Meta-analyses of the published literature indicate that about 9% of gastric cancers contain Epstein-Barr virus (EBV), with consistent and significant differences by sex and anatomic subsite. This study aimed to identify additional determinants of EBV positivity and their joint effects.
Methods:
From 15 international populations with consistent laboratory testing for EBV, we pooled individual-level data for 5081 gastric cancer cases including information on age, sex, subsite, histologic type, diagnostic stage, geographic region, and period of diagnosis. First, we combined population-specific EBV prevalence estimates using random effects meta-analysis. We then aggregated individual-level data to estimate odds ratios of EBV positivity in relation to all variables, accounting for within-population clustering.
Results:
In unadjusted analyses, EBV positivity was significantly higher in males, young subjects, non-antral subsites, diffuse-type histology, and in studies from the Americas. Multivariable analyses confirmed significant associations with histology and region. Sex interacted with age (P=0.003) and subsite (P=0.002) such that male predominance decreased with age for both subsites. The positivity of EBV was not significantly associated with either stage or time period.
Conclusion:
Aggregating individual-level data provides additional information over meta-analyses. Distinguishing histologic and geographic features as well as interactions among age, sex, and subsite further support classification of EBV-associated gastric cancer as a distinct aetiologic entity.
Similar content being viewed by others
Main
Gastric cancer is the second leading cause of cancer-related deaths worldwide (Parkin et al, 2005). Chronic Helicobacter pylori infection is considered to be the initiating factor in gastric carcinogenesis (International Agency for Research on Cancer, 1994), although human genetic polymorphisms and environmental factors also modulate risk of neoplasia (Correa et al, 2006; Hamajima et al, 2006).
Epstein-Barr virus (EBV) is a ubiquitous infectious agent which has been causally linked to the development of several malignancies, including Burkitt's lymphoma, immunosuppression-related lymphoma, Hodgkin's lymphoma, and nasopharyngeal carcinoma (International Agency for Research on Cancer, 1997). Although some cases of gastric adenocarcinoma harbour EBV infection (Takada, 2000; Akiba et al, 2008), it remains unclear whether the presence of EBV is a cause or a consequence of neoplastic changes.
To expand on our recent meta-analysis of EBV prevalence in gastric cancer (Murphy et al, 2009), we have conducted a pooled analysis of individual-level data on variables for which the published aggregate data were insufficient for meta-analysis. In addition, we aimed to investigate whether EBV positivity is modified by the joint effect of these determinants.
Materials and methods
Data sources
Over the past 10 years, one of us (SA) has participated in multiple international collaborations assessing the presence of EBV in gastric cancer tumours in Asia and Latin America. In general, these studies followed a common protocol evaluating EBV infection by EBV-encoded small RNA in situ hybridisation. In the present reanalysis, we have combined individual-level data of 12 of these studies from areas with differing risk profiles for gastric cancer (Corvalan et al, 2001; Koriyama et al, 2001, 2004; Hao et al, 2002; Kattoor et al, 2002; Carrascal et al, 2003; Lee et al, 2004; Anwar et al, 2005; Herrera-Goepfert et al, 2005; Yoshiwara et al, 2005; Campos et al, 2006; Abdirad et al, 2007). Since none of these studies was conducted in North America or Europe, these geographic areas were not represented in our analysis. We included information on EBV status, sex, age at diagnosis, geographic region, histologic type, anatomic subsite, diagnostic stage, and year of diagnosis. Two of the identified studies (Koriyama et al, 2001; Hao et al, 2002) reported findings from more than one population group, and thus, data on 15 distinct populations were analysed.
Statistical analyses
Given the limited sample size in some studies, EBV prevalence and corresponding standard errors (s.e.) were calculated by the Wilson method (Wilson, 1927) for each population, overall and separately for the following five covariables: age at diagnosis (treated as a continuous and as a categorical variable), sex (male vs female), anatomic subsite (antrum vs other subsites; overlapping cases were excluded), diagnostic stage (early vs advanced), and Lauren histologic type (diffuse vs intestinal). The diffuse subtype included the following Japanese histologic classifications: solid type poorly differentiated adenocarcinoma (por1), non-solid type poorly differentiated adenocarcinoma (por2), signet-ring cell carcinoma (sig), and lymphepithelial-like carcinoma (LE). The intestinal subtype included the following: well-differentiated type tubular adenocarcinoma (tub1), moderately differentiated type tubular adenocarcinoma (tub2), papillary adenocarcinoma (pap), and mucinous adenocarcinoma (muc). Population-specific log odds ratios (ORs) and 95% confidence intervals (CIs) of EBV positivity were calculated for the same five covariables using standard logistic regression models. Strata with no EBV-positive cases were assigned an arbitrary prevalence of 1% to allow calculation of ORs and for the subsequent meta-analysis.
Random effects meta-analysis (DerSimonian and Laird, 1986) was used to pool overall log prevalence estimates, with s.e. (log prevalence) calculated by the Delta-method as 1/prevalence × s.e. (prevalence), and to pool log ORs for covariables. Between study heterogeneity was assessed using the I2 and Q statistics, with I2 >50% or PQ<0.05 indicating heterogeneity (Deeks, 2002; Higgins and Thompson, 2002).
To increase statistical precision, pooled ORs were also estimated for aggregated data using logistic regression models that included a random population-specific intercept. This approach avoided the computational requirement for non-zero prevalence for all subgroups. In addition to the covariables-listed above, we also assessed the separate effects of geographic region (Americas vs Asia), estimated national gastric cancer incidence rates in 2008 (<10, 10–19.9, and ⩾20 cases per 100 000 population; Ferlay et al, 2010), year of diagnosis, and decade of birth. Year of diagnosis was treated alternatively as a continuous or categorical (⩽1959, 1960–1969, 1970–1979, 1980–1989, and ⩾1990) variable. Decade of birth was also treated as either continuous or categorical (⩽1919, 1920–1929, 1930–1939, 1940–1949, 1950–1959, and ⩾1960). Additionally, age, year of diagnosis, and decade of birth were tested for non-linear associations with EBV positivity by including the squared terms of the variables in the respective models. Two-sided P-values for associations <0.05 were considered statistically significant. Pooled ORs for the meta-analytic and aggregated approaches were generally similar, so only the aggregated estimates are presented.
To assess interactions and evaluate confounding, we performed multivariable aggregated analysis, excluding the terms for decade of birth and national incidence due to collinearity with age and period and with region, respectively. To evaluate effect modification, we generated cross-product terms for the six pairwise combinations of the four variables significantly associated with EBV positivity (i.e., age at diagnosis, sex, anatomic subsite, and histologic type). In the final models, age at diagnosis was treated as a continuous variable and adjustments were included for stage, decade of diagnosis, and geographic region. Wald χ2-tests were used to assess interaction terms, with P-values corrected for multiple comparisons of <0.0083 (0.05/6) considered statistically significant. Estimated parameters from the final regression model were used to calculate age-specific prevalence of EBV positivity by sex and anatomic subsite, as well as age- and subsite-specific ORs of EBV positivity for males compared with females. All statistical analyses were performed in Stata 10.0 (Stata Corp, College Station, TX, USA).
Results
A total of 5081 gastric cancer cases from 15 different populations contributed to these analyses (Table 1). The meta-analytic estimated prevalence of EBV positivity was 7.7% overall (95% CI: 6.1–9.8), with high heterogeneity among studies (I2=77.5%, PQ<0.001; Figure 1).
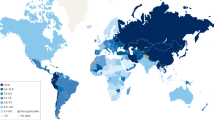
In unadjusted analyses (Table 2), the following association patterns emerged: (a) tumours in young subjects were more likely to be EBV positive than those in older subjects, (b) tumours in males were more than twice as likely to be EBV positive than tumours in females, (c) non-antral tumours were more likely to be EBV positive than those arising in the antrum, (d) diffuse-type tumours were almost twice as likely to be EBV positive than tumours of intestinal histology, and (e) EBV prevalence was similar in early and advanced tumours. Furthermore, EBV positivity did not significantly differ by decade of birth (ORs for comparison with 1910s or earlier: 1.3 for 1920s, 1.1 for 1930s, 1.2 for 1940s, 1.5 for 1950s, and 1.6 for 1960s or later) or decade of diagnosis (ORs using 1990 or later as referent: 0.7 for ⩽1959, 1.2 for 1960s, 1.0 for 1970s, and 1.3 for 1980s). However, EBV positivity was significantly higher for studies conducted in the Americas as compared with those in Asia (OR: 1.7, 95% CI: 1.1–2.7) and marginally lower in countries with gastric cancer incidence rates <10 or ⩾20 cases per 100 000 population as compared with 10–19.9 cases per 100 000 population (OR: 0.5, 95% CI: 0.3–1.0 and OR: 0.7, 95% CI: 0.4–1.1, respectively). Inclusion of squared terms for age, decade of birth and period did not significantly improve the fit of models with linear terms for these variables.
The multivariable aggregated analyses identified four pairwise interactions at the P<0.05 level: sex and anatomic subsite (P-value=0.002), age and sex (P-value=0.003), age and anatomic subsite (P-value=0.011), and age and histologic type (P-value=0.013), with only the first two statistically significant as corrected for multiple comparisons. Prevalence of EBV positivity decreased with age among men, more steeply for tumours localised to the antrum than for those localised to other anatomic subsites (Figure 2). In contrast, there was no significant variation by age among women, although tumours in non-antral subsites had slightly higher EBV prevalence. In terms of the risk estimates, male predominance decreased with age for both subsites (Table 3).
In a final model that included the two significant interactions, we confirmed the associations of EBV positivity with diffuse-type histology (OR: 2.0, 95% CI: 1.5–2.6) and with studies from the Americas (OR: 2.3, 95% CI: 1.5–3.7). Differences by diagnostic stage or period of diagnosis were not statistically significant.
Discussion
We analysed individual-level participant data on 5081 subjects with gastric cancer from international studies we previously conducted with a consistent approach to EBV testing. As compared with our individual reports, the present reanalysis had greater statistical power for robust observations. The magnitude of the observed pooled prevalence (7.7%; 95% CI: 6.1–9.8%) and the degree of heterogeneity among our studies were similar to that reported in previous meta-analyses of the published literature (Lee et al, 2009; Murphy et al, 2009; Li et al, 2010). Moreover, this pooled analysis also evaluated associations with additional variables that were not included in prior meta-analyses, provided adjusted estimates, and was able to examine interactions.
Previous reports have indicated that EBV-positive gastric tumours tend to be proximally located, and account for a greater proportion of cases in males than in females (Murphy et al, 2009). However, few studies have found variation by age (Chang et al, 2003; van Beek et al, 2004). With our large data set, we found that EBV positivity varies jointly by age, sex, and anatomic subsite, interactions that may be obscuring a main effect of age. The young predominance in males and the countervailing age trend in females suggest the importance of occupational, hormonal, and/or lifestyle factors in the aetiology of EBV-associated gastric cancer.
H. pylori infection preferentially colonises the antrum (Martín-de-Argila et al, 1997), so the contrasting localisation of EBV-positive gastric cancer to non-antral subsites suggests possible antagonism between the two infectious agents. An in vitro study directly examining this interaction found that reactive products from H. pylori infection trigger EBV reactivation in latently infected gastric epithelial cells (Minoura-Etoh et al, 2006).
Two reports encompassed in the present analysis have examined variation in EBV prevalence of gastric tumours over time or birth cohort. Abdirad et al (2007) noted a cluster of EBV positivity in cancers of a specific birth cohort (Iranians born 1928–1930). However, Herrera-Goepfert et al (2005) found similar EBV prevalence in Mexican cases diagnosed during 1980–1989 as compared with those diagnosed in 1990–2000. Our pooled analysis, using data on cases diagnosed between 1949 and 2004, did not find consistent changes over time.
An inverse relationship has previously been suggested between the background population incidence of gastric cancer and EBV prevalence in the tumours (Murphy et al, 2009). In our data, EBV positivity was similar for cases in countries with high and low background incidence, but significantly higher in tumours from the Americas as compared with those from Asia. While we cannot distinguish their independent effects, EBV-positive gastric cancer may differ by geographic region rather than with background incidence per se.
While results from previous meta-analyses disagreed regarding associations with histologic subtype (Lee et al, 2009; Murphy et al, 2009; Li et al, 2010), we found a higher EBV prevalence in diffuse-type tumours. Histologic classification differs among pathologists (Borchard, 1990) and our pooled analysis may have had more consistent laboratory methods and pathologic review than the varied approaches in the published literature.
Although it has been suggested that EBV-positive gastric cancer cases may have a better prognosis than EBV-negative cases, previous individual reports are limited and somewhat inconsistent. Recently, Song et al (2010) reported a survival advantage for certain histologic subgroups of EBV-associated gastric cancer in a large Korean series, but there was no significant survival advantage for EBV-positive tumours overall. A meta-analytic review by Lee et al (2009) including seven studies did not find associations with the clinicopathologic prognostic indicators clinical stage, depth of invasion, or lymph node metastasis. Our null finding for clinical stage was consistent with this meta-analysis and, importantly, our estimates were also adjusted for possible confounders.
Although the specific role of EBV in gastric carcinogenesis has not yet been elucidated, several lines of evidence support its aetiological significance. Epstein-Barr virus-positive gastric carcinomas exhibit uniform presence of monoclonal viral episomes in the tumour cells (Ott et al, 1994). Epstein-Barr virus-positive gastric carcinomas also display distinct clinical and genetic features relative to EBV-negative tumours (zur Hausen et al, 2000; van Beek et al, 2004). In addition, some studies have found elevated serum antibodies against viral capsid and nuclear antigens preceding development of preneoplastic and neoplastic gastric lesions (Levine et al, 1995; Schetter et al, 2008).
Histologic specificity and geographic variation suggest that EBV-positive gastric cancer is a distinct entity. The pairwise interactions that we found among age, sex, and anatomic subsite are novel and should be explored further. Our findings reveal a complex interplay of factors influencing EBV's presence in gastric tumours and may provide important clues to understanding its aetiologic significance.
Change history
29 March 2012
This paper was modified 12 months after initial publication to switch to Creative Commons licence terms, as noted at publication
References
Abdirad A, Ghaderi-Sohi S, Shuyama K, Koriyama C, Nadimi-Barforoosh H, Emami S, Mosavi-Jarrahi A, Nahvijou A, Akiba S (2007) Epstein-Barr virus associated gastric carcinoma: a report from Iran in the last four decades. Diagn Pathol 2: 25
Akiba S, Koriyama C, Herrera-Goepfert R, Eizuru Y (2008) Epstein-Barr virus associated gastric carcinoma: epidemiological and clinicopathological features. Cancer Sci 99: 195–201
Anwar M, Koriyama C, Naveed IA, Hamid S, Ahmad M, Itoh T, Minakami Y, Eizuru Y, Akiba S (2005) Epstein-Barr virus detection in tumors of upper gastrointestinal tract. An in situ hybridization study in Pakistan. J Exp Clin Cancer Res 24: 379–385
Borchard F (1990) Classification of gastric carcinoma. Hepatogastroenterology 37: 223–232
Campos FI, Koriyama C, Akiba S, Carrasquilla G, Serra M, Carrascal E, Itoh, T, Minakami Y, Eizuru Y (2006) Environmental factors related to gastric cancer associated with Epstein-Barr virus in Colombia. Asian Pac J Cancer Prev 7: 633–637
Carrascal E, Koriyama C, Akiba S, Tamayo O, Itoh T, Eizuru Y, Garcia F, Sera M, Carrasquilla G, Piazuelo MB, Florez L, Bravo JC (2003) Epstein-Barr virus-associated gastric carcinoma in Cali, Colombia. Oncol Rep 10: 1059–1062
Chang MS, Lee HS, Kim HS, Kim SH, Choi SI, Lee BL, Kim CW, Kim YI, Yang M, Kim WH (2003) Epstein-Barr virus and microsatellite instability in gastric carcinogenesis. J Pathol 199: 447–452
Correa P, Piazuelo MB, Camargo MC (2006) Etiopathogenesis of gastric cancer. Scand J Surg 95: 218–224
Corvalan A, Koriyama C, Akiba S, Eizuru Y, Backhouse C, Palma M, Argandoña J, Tokunaga M (2001) Epstein-Barr virus in gastric carcinoma is associated with location in the cardia and with a diffuse histology: a study in one area of Chile. Int J Cancer 94: 527–530
Deeks JJ (2002) Issues in the selection of a summary statistic for meta-analysis of clinical trials with binary outcomes. Stat Med 21: 1575–1600
DerSimonian R, Laird N (1986) Meta-analysis in clinical trials. Control Clin Trials 7: 177–188
Ferlay J, Shin HR, Bray F, Forman D, Mathers C, Parkin DM (2010) GLOBOCAN 2008, Cancer Incidence and Mortality Worldwide: IARC CancerBase No. 10 (Internet). International Agency for Research on Cancer: Lyon, France. Available from: http://globocan.iarc.fr
Hamajima N, Naito M, Kondo T, Goto Y (2006) Genetic factors involved in the development of Helicobacter pylori-related gastric cancer. Cancer Sci 97: 1129–1138
Hao Z, Koriyama C, Akiba S, Li J, Luo X, Itoh T, Eizuru Y, Zou J (2002) The Epstein-Barr virus-associated gastric carcinoma in Southern and Northern China. Oncol Rep 9: 1293–1298
Herrera-Goepfert R, Akiba S, Koriyama C, Ding S, Reyes E, Itoh T, Minakami Y, Eizuru Y (2005) Epstein-Barr virus-associated gastric carcinoma: evidence of age-dependence among a Mexican population. World J Gastroenterol 11: 6096–6103
Higgins JP, Thompson SG (2002) Quantifying heterogeneity in a meta-analysis. Stat Med 21: 1539–1558
International Agency for Research on Cancer (1994) Monographs on the Evaluation of Carcinogenic Risks to Humans. Schistosomes, Liver Flukes and Helicobacter Pylori, vol. 61. IARC Press: Lyon, pp 177–240
International Agency for Research on Cancer (1997) Monographs on the Evaluation of Carcinogenic Risks to Humans. Epstein-Barr Virus and Kaposi's Sarcoma Herpesvirus/Human Herpesvirus 8. IARC Press: Lyon, pp 347–373
Kattoor J, Koriyama C, Akiba S, Itoh T, Ding S, Eizuru Y, Abraham EK, Chandralekha B, Amma NS, Nair MK (2002) Epstein-Barr virus-associated gastric carcinoma in southern India: A comparison with a large-scale Japanese series. J Med Virol 68: 384–389
Koriyama C, Akiba S, Corvalan A, Carrascal E, Itoh T, Herrera-Goepfert R, Eizuru Y, Tokunaga M (2004) Histology-specific gender, age and tumor-location distributions of Epstein-Barr virus-associated gastric carcinoma in Japan. Oncol Rep 12: 543–547
Koriyama C, Akiba S, Iriya K, Yamaguti T, Hamada GS, Itoh T, Eizuru Y, Aikou T, Watanabe S, Tsugane S, Tokunaga M (2001) Epstein-Barr virus-associated gastric carcinoma in Japanese Brazilians and non-Japanese Brazilians in São Paulo. Jpn J Cancer Res 92: 911–917
Lee HS, Chang MS, Yang HK, Lee BL, Kim WH (2004) Epstein-Barr virus-positive gastric carcinoma has a distinct protein expression profile in comparison with Epstein-Barr virus-negative carcinoma. Clin Cancer Res 10: 1698–1705
Lee JH, Kim SH, Han SH, An JS, Lee ES, Kim YS (2009) Clinicopathological and molecular characteristics of Epstein-Barr virus-associated gastric carcinoma: a meta-analysis. J Gastroenterol Hepatol 24: 354–365
Levine PH, Stemmermann G, Lennette ET, Hildesheim A, Shibata D, Nomura A (1995) Elevated antibody titers to Epstein-Barr virus prior to the diagnosis of Epstein-Barr-virus-associated gastric adenocarcinoma. Int J Cancer 60: 642–644
Li S, Du H, Wang Z, Zhou L, Zhao X, Zeng Y (2010) Meta-analysis of the relationship between Epstein-Barr virus infection and clinicopathological features of patients with gastric carcinoma. Sci China Life Sci 53: 524–530
Martín-de-Argila C, Boixeda D, Redondo C, Alvarez I, Gisbert JP, García Plaza A, Cantón R (1997) Relation between histologic subtypes and location of gastric cancer and Helicobacter pylori. Scand J Gastroenterol 32: 303–307
Minoura-Etoh J, Gotoh K, Sato R, Ogata M, Kaku N, Fujioka T, Nishizono A (2006) Helicobacter pylori-associated oxidant monochloramine induces reactivation of Epstein-Barr virus (EBV) in gastric epithelial cells latently infected with EBV. J Med Microbiol 55: 905–911
Murphy G, Pfeiffer R, Camargo MC, Rabkin CS (2009) Meta-analysis shows that prevalence of Epstein-Barr virus-positive gastric cancer differs based on sex and anatomic location. Gastroenterology 137: 824–833
Ott G, Kirchner T, Müller-Hermelink HK (1994) Monoclonal Epstein-Barr virus genomes but lack of EBV-related protein expression in different types of gastric carcinoma. Histopathology 25: 323–329
Parkin DM, Bray F, Ferlay J, Pisani P (2005) Global cancer statistics, 2002. CA Cancer J Clin 55: 74–108
Schetter AJ, You WC, Lennette ET, Gail MT, Rabkin CS (2008) Association of Epstein-Barr virus antibody levels with precancerous gastric lesions in a high-risk cohort. Cancer Sci 99: 350–354
Song HJ, Srivastava A, Lee J, Kim YS, Kim KM, Ki Kang W, Kim M, Kim S, Park CK, Kim S (2010) Host inflammatory response predicts survival of patients with Epstein-Barr virus-associated gastric carcinoma. Gastroenterology 139: 84–92.e2
Takada K (2000) Epstein-Barr virus and gastric carcinoma. Mol Pathol 53: 255–261
van Beek J, zur Hausen A, Klein Kranenbarg E, van de Velde CJ, Middeldorp JM, van den Brule AJ, Meijer CJ, Bloemena E (2004) EBV-positive gastric adenocarcinomas: a distinct clinicopathologic entity with a low frequency of lymph node involvement. J Clin Oncol 22: 664–670
Wilson EB (1927) Probable inference, the law of succession, and statistical inference. J Am Stat Assoc 22: 209–212
Yoshiwara E, Koriyama C, Akiba S, Itoh T, Minakami Y, Chirinos JL, Watanabe J, Takano J, Miyagui J, Hidalgo H, Chacon P, Linares V, Eizuru Y (2005) Epstein-Barr virus-associated gastric carcinoma in Lima, Peru. J Exp Clin Cancer Res 24: 49–54
zur Hausen A, Brink AA, Craanen ME, Middeldorp JM, Meijer CJ, van den Brule AJ (2000) Unique transcription pattern of Epstein-Barr virus (EBV) in EBV-carrying gastric adenocarcinomas: expression of the transforming BARF1 gene. Cancer Res 60: 2745–2748
Acknowledgements
This study was funded by the Intramural Research Program of the National Cancer Institute, National Institutes of Health. We thank Dr Garth Rauscher for his helpful comments on an earlier version of this manuscript. The findings and conclusions in this report are those of the authors and do not necessarily represent the official position of the United States National Cancer Institute.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
From twelve months after its original publication, this work is licensed under the Creative Commons Attribution-NonCommercial-Share Alike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Camargo, M., Murphy, G., Koriyama, C. et al. Determinants of Epstein-Barr virus-positive gastric cancer: an international pooled analysis. Br J Cancer 105, 38–43 (2011). https://doi.org/10.1038/bjc.2011.215
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bjc.2011.215
Keywords
This article is cited by
-
CHSY3 promotes proliferation and migration in gastric cancer and is associated with immune infiltration
Journal of Translational Medicine (2023)
-
Global burden of gastric cancer: epidemiological trends, risk factors, screening and prevention
Nature Reviews Clinical Oncology (2023)
-
Genetic landscape and PD-L1 expression in Epstein–Barr virus-associated gastric cancer according to the histological pattern
Scientific Reports (2023)
-
MiR-BART1-3p and BART18-5p inhibit cell migration, proliferation and activate autophagy in Epstein-Barr virus-associated gastric cancer by targeting erythropoietin-producing human hepatocellular 2
Virus Genes (2023)
-
PD-L1 expression in EBV associated gastric cancer: a systematic review and meta-analysis
Discover Oncology (2022)