Abstract
Suppressor of cytokine signaling 1 (SOCS1) protein, which encodes a member of signal transducers and activators of transcription-induced inhibitors, takes part in a negative regulation of cytokine signaling. The mechanism of SOCS1 in tumor carcinogenesis is complex and there have been no studies concerning the clinic-biologic implication of SOCS1 expression in acute myeloid leukemia (AML). Here, we first identified that higher bone marrow (BM) SOCS1 expression was closely associated with older age, FLT3-ITD, NPM1 and DNMT3A mutations, but negatively correlated with CEBPA mutation in patients with de novo AML. Compared to patients with lower SOCS1 expression, those with higher expression had lower complete remission rates and shorter overall survival. Further, higher expression of SOCS1 in the BM was an independent unfavorable prognostic factor irrespective of age, white blood cell, cytogenetics and gene mutations. Next, we generated zebrafish model overexpressing SOCS1 by spi1 promoter, which showed kidney marrow from adult SOCS1 zebrafish had increased myelopoiesis, myeloid progenitors and the kidney or spleen structure were effaced and distorted, mimicking leukemia phenotype. The SOCS1/FLT3-ITD double transgenic fish could further facilitate the leukemic process. The results indicate SOCS1 plays an important role in AML and its higher expression serves as a new biomarker to risk-stratify AML patients.
Similar content being viewed by others
Introduction
Suppressor of cytokine signaling (SOCS) proteins are negative feedback regulators of the JAK-STAT signaling pathway and aberrant SOCS expression is associated with dysregulated immunity, inflammation and malignant processes.1 Alterations of SOCS1 expression are often seen in cancers and may contribute to tumorigenesis, cancer progression and metastasis.2, 3 The prognostic relevance of SOCS1 expression in tumor cells is controversial. Higher SOCS1 expression was associated with early tumor stage and better overall survival (OS) in breast cancer.4 On the other hand, increased SOCS1 expression was shown to be correlated with tumor progression and poor prognosis in melanoma.5 Regarding hematologic malignancies, SOCS1 messenger RNA overexpression was noted in two-thirds of chronic myeloid leukemia patients and was associated with shorter progression-free survival and poorer cytogenetic response to interferon treatment.6
To date, little is known about the clinical implication of SOCS1 expression and its role in leukemogenesis in acute myeloid leukemia (AML). In this study, we investigated the bone marrow (BM) SOCS1 expression in an original cohort of 223 adults with de novo AML and correlated the results with clinical features and outcomes of the patients. To the best of our knowledge, this is the first report to address the prognostic implication of SOCS1 expression in AML patients. We found that higher BM SOCS1 expression is an independent unfavorable prognostic factor for OS in these patients, and the finding was also validated in an independent validation cohort. We also demonstrated that SOCS1 expression and FLT3-ITD, a common mutation in AML, synergistically promoted myeloid hyperplasia with expansion of precursor cells in zebrafish.
Materials and methods
Patients
An original cohort comprised 223 adults 15 years of age or older with newly diagnosed de novo AML at the National Taiwan University Hospital (NTUH) from May 1995 to December 2007, who had complete clinical data and enough cryopreserved BM samples for analysis. Thirty normal marrow donors were also enrolled for comparison. Diagnosis and classification of AML were made according to the French–American–British (FAB) Cooperative Group Criteria. Patients with antecedent hematological diseases or therapy-related AML were excluded. The expression of BM SOCS1 was determined before treatment. Among the 223 patients, 154 (69.1%) received standard induction chemotherapy (idarubicin 12 mg/m2 per day for 3 days and cytarabine 100 mg/m2 per day for 7 days) and then consolidation chemotherapy with 2–4 courses of high-dose cytarabine (2000 mg/m2 every 12 h for 4 days, total eight doses), with or without an anthracycline (idarubicin or mitoxantrone), after achieving complete remission (CR).7 The patients with acute promyelocytic leukemia (M3 subtype) received concurrent all-trans retinoic acid and chemotherapy. Twenty-one patients received allogeneic hematopoietic stem cell transplantation (HSCT) in CR1. The remaining 69 patients received palliative therapy with supportive care and/or low-dose chemotherapy due to underlying comorbidity or based on the decision of the patients. The validation cohort comprised 73 adults 15 years of age or older with newly diagnosed non-M3 AML at the NTUH from January 2008 to November 2011. These patients were treated with the same regimens as those in the original cohort and were used to validate the prognostic impact of BM SOCS1 expression in AML. This study was approved by the Institutional Review Board of the NTUH (201207060RIC and 201503072RINC) and was done in accordance with the Declaration of Helsinki. All patients and normal donors signed the informed consents.
Real-time quantitative PCR
BM mononuclear cells from both cohorts and 30 healthy transplantation donors were isolated and cryopreserved until use. Total RNA was extracted and reverse transcribed. The gene expression level was quantified using TaqMan technology on the Applied Biosystems 7500/7500 Fast Real-Time PCR System (Carlsbad, CA, USA) as previously described.8 Gene-specific primers and probe of SOCS1 were available on TaqMan Gene Expression Assay (Assay id, Hs00705164_s1, ThermoFisher Scientific, Waltham, MA, USA). Each sample was tested at least twice independently. The amount of the target gene was normalized to the housekeeping gene RPLP0. The copies of target gene were quantified only after successful amplification of the internal control, using the standard curves derived from cloned plasmids. All data were presented as log ratio of the target gene/RPLP0.
Immunophenotyping
A panel of monoclonal antibodies to myeloid-associated antigens, including CD13, CD33, CD11b, CD15, CD14 and CD41a, as well as lymphoid-associated antigens including CD2, CD5, CD7, CD19, CD10 and CD20 and lineage non-specific antigens HLA-DR, CD34 and CD56 were used to characterize the phenotypes of the leukemia cells as previously described.9
Cytogenetic study
BM cells were harvested directly or after 1–3 days of unstimulated culture as described previously.10 The metaphase cells were banded by trypsin-Giemsa technique and karyotyped according to the International System for Human Cytogenetic Nomenclature.
Mutation analysis
Mutation analyses of 19 relevant molecular marker genes, including Class I mutations, such as FLT3/ITD and FLT3/TKD,11 NRAS,12 KRAS,12 JAK2,12 KIT13 and PTPN11,13 mutations, and Class II mutations, such as CEBPA14 and RUNX1,15 mutations, as well as mutations of NPM,16 WT1,17 TP53,18 splicing genes (SF3B1, SRSF2 and U2AF1),19 and those related to epigenetic modifications, such as MLL/PTD,20 ASXL1,7 IDH1,21 IDH2,22 TET2,23 and DNMT3A9 were performed as previously described. Abnormal sequencing results were confirmed by at least two repeated analyses.
Zebrafish husbandry
Zebrafish embryos, larvae, and adult fish were maintained at 28 °C under continuous flow and a 14-h light and 10-h dark cycle in the zebrafish core facility.24 All experiments involving zebrafish were approved by the Institutional Animal Care and Use Committee (IACUC) of the National Taiwan University (NTU) (IACUC Approval No: 20130373).
Generation of spi1: SOCS1-2A-mCherry/CG2 transgenic zebrafish using the Tol2 transposon system
To create the pME entry clone, the human SOCS1 gene was amplified using the primer pair of attB1-SOCS1-forward (5′-GGGGACAAGTTTGTACA AAAAAGCAGGCTATGGTAGCACACAACCAGGT-3′) and attB2-SOCS1 -reverse (5′-GGGGACCACTTTGTACAAGAAAGCTGGGTAAATCTGGAAGG GGAAGGAGC-3′) and the MV4–11 complimentary DNA (cDNA) as template. The attB1 and attB2 sites, highlighted by underlines, were added to the 5’ end of the primer pair of SOCS1, respectively. The PCR products were recombined into pDONR221 (Invitrogen, Grand Island, NY, USA) to generate pME-SOCS1. The plasmids were constructed in accordance with manufacturer’s protocol (MultiSite Gateway Three-Fragment Vector Construction Kit, Invitrogen). Finally, p5E-spi1, pME-SOCS1 and p3E-2A-mCherrypA were assembled together with pDestTol2CG2 by LR reaction to create expression plasmid of spi1:SOCS1-2A-mCherry/CG2. All plasmid constructs were confirmed by sequencing. The transgenic founders were generated with the Tol2 transposon system using previously described methods.25
Transposase RNA synthesis and microinjection
To generate transposase RNA for injection, the pCS2FA-transposase plasmid was digested with NotI at 37 °C overnight and the NucleoSpin Gel and PCR clean-up kit (Macherey-Nagel, Düren, Germany) were used to purify and concentrate amplified DNA. Linearized plasmid was synthesized by mMESSAGE mMachine SP6 Kit (Ambion, Austin, Texas, USA). For generation of transgenic zebrafish, expression construct of pDestTol2CG2-spi1-SOCS1-2A-mCherrypA (25 pg/μl) was mixed with in vitro-transcribed transposases messenger RNA (25 pg/μl), and 2.3 nl of the mixture was co-injected into the animal pole of one-cell stage embryos. After the microinjection process was completed, we selected positively transgenic larvae for further study, and these positive F0 fish were outcrossed with wild-type (WT) fish to establish stable transgenic lines.25
Generation of spi1:SOCS1/FLT3-ITD double transgenic zebrafish
To establish this double transgenic (dTg) fish, we crossed Tg (spi1:SOCS1-2A-mCherry/CG2) and Tg (spi1:FLT3-ITD-2A-EGFP/CG2)25 fish to create dTg fish expressing simultaneously SOCS1 and FLT3-ITD in a WT background. We selected positive larvae for further study, and these positive F1 embryos from transgenic fish were maintained until they reached the adult stage. In the adult stage, genomic DNA analysis did reveal both SOCS1 expression and FLT3-ITD in 9-month-old dTg fish.
Isolation of RNA and reverse transcription PCR
Total RNA was isolated with the RNAspin Mini RNA Isolation Kit (GE Healthcare, Pittsburgh, PA, USA). RNA (1 μg) was then reverse transcribed into cDNA using the High-Capacity RNA-to-cDNA Kit (Applied Biosystems). Following the reverse transcription reaction, cDNA templates were amplified by PCR with KOD-FX Taq polymerase (TOYOBO, Osaka Japan). One microliter cDNA was amplified with PCR reaction, comprising 1 cycle at 95 °C for 5 min, 35 cycles at 95 °C for 10 s, 58 °C for 30 s and 68 °C for 1 min, and finally incubated at 68 °C for an additional 7 min to allow for the completion of synthesis. PCR products were subjected to 1.0% agarose gel electrophoresis, and actin was used as an internal control for cDNA assay.25 The primers used were as follows: SOCS1-forward: 5′-ATGGTAGCACACAACCAGGT-3′; SOCS1-reverse: 5′-AAATCTGGAAGGGGAAGGAGC-3′; actin-forward: 5′-CT CCATCATGAAGTGCGACGT-3′; actin-reverse: 5′-CAGACGGAGTATTTGCGC TCA-3′
Immunohistochemical staining
For immunohistochemistry, zebrafish tissue sections were deparaffinized using xylene and rehydrated with serial dilutions of ethanol in a stepwise fashion. Endogenous peroxidase activity was then blocked by pressure-cooking at 100 °C for 15 min in 1 × tris-ethylenediaminetetraacetic acid (pH 9.0) and tissue slides were treated with 3% H2O2 for antigen retrieval at 20 min. The slides were first incubated with protein blocker for 30 min at room temperature and then incubated with rabbit anti-SOCS1 antibodies (Catalog Number: SC-7005-R, Santa Cruz Biotechnology, Santa Cruz, CA, USA, at a 1:100 dilution) at 4 °C overnight. After washing with 1 × phosphate-buffered saline (PBS), tissue sections were developed using the EnVision+ Dual Link System (Dako, Carpinteria, CA, USA). Finally, the slides were counterstained with hematoxylin for 30 s, and mounted with slide covers for evaluation under light microscopy.25
Flow cytometric analysis
Zebrafish were anaesthetized with 0.02% tricaine. After being dissected, peripheral blood (PB) and kidneys were placed into ice-cold 0.9 × PBS containing 5% fetal bovine serum (FBS). Whole cells from kidneys were filtered through a 40-mm cell strainer (BD Falcon, San Jose, CA, USA), spun down at 1200 r.p.m. for 5 min at 4 °C, and then washed two times before being harvested in 0.9 × PBS with 5% FBS. The suspended cells were stained with propidium iodide (PI, 50 ng/ml) for 10 min in the dark, and PI-positive cells were quantified by flow cytometry.26 The cell suspension was also subjected to LS-RII (BD Bioscience, San Jose, CA, USA), and further analyzed with FlowJo (Tree Star, Ashland, OR, USA). Cell size and granularity were determined by forward scatter (FSC; abscissa) and side scatter (SSC; ordinate), respectively. Gated populations were as follows: immature and mature erythrocytes, lymphocytes, myelomonocytes and precursor cells. A total of five (9M-WT) and five samples (9M-FLT3-ITD) were collected from previously data.25
Cytological analysis of kidney marrow and PB
Zebrafish were killed at 9 and 12 months of age, respectively. PB was obtained by puncturing the tail using micropipette tips coated with heparin. Blood samples were immediately placed into ice-cold 0.9 × PBS with 5% FBS. Kidney marrow (KM) and PB cells were collected, and cytospin smears were prepared for further cytological analysis. Over 300 marrow cells were evaluated and recognized as either myeloid progenitors, myelomonocytes, lymphocytes, immature erythrocytes or mature erythrocytes.
Statistical analysis
The discrete variables of patients with lower and higher SOCS1 expression were compared using the χ2-tests or Fisher’s exact test. We used Mann–Whitney U-test to compare continuous variables and medians of distributions. OS was measured from the date of first diagnosis to death from any cause or the last follow-up, whereas relapse was defined as a reappearance of at least 5% leukemic blasts in a BM aspirate or new extramedullary leukemia in patients with a previously documented CR.27 Disease-free status indicated that the patient achieved CR and did not relapse by the end of this study, and disease-free survival was defined as the time from recruitment to the first of three events: treatment failure, leukemia relapse or death from any cause. To exclude confounding influences of different treatment regimens, patients who received allogeneic HSCT were censored on the day of cell infusion.7 We adopted Kaplan–Meier estimation to plot survival curves, and used log-rank tests to examine the difference between groups. The variables including age,28 white blood cell counts at diagnosis, karyotype, NPM1/FLT3-ITD, CEBPA, RUNX1, WT1, ASXL1, IDH2, DNMT3A, TP53 and splicing factors mutations were used as covariates in multivariate analysis. Relative risk and 95% confidence interval were estimated by Cox proportional hazards regression models to determine independent risk factors associated with survival in multivariate analyses. The unpaired Student's t-test was used in the flow cytometric analysis. Two-sided P-values <0.05 were considered statistically significant. Whole patient population was included for analyses of the correlation between SOCS1 expression and clinical characteristics, however, only those receiving conventional standard chemotherapy, as mentioned above, were included in analyses of survivals. All statistical analyses were accomplished with the SPSS 17 (SPSS Inc., Chicago, IL, USA) and Statsdirect (2.7.8b, 2011, StatsDirect Ltd., Cheshire, UK).
Results
Correlation of BM SOCS1 expression with clinical features and laboratory data in the original cohort
BM SOCS1 expression, as determined by real-time quantitative PCR, varied greatly in the AML patients. The median value of BM SOCS1 expression in total AML patients was used as the cut-off point to define lower- and higher-expression groups. The comparison of clinical characteristics of patients with lower and higher SOCS1 expression is shown in Supplementary Table 1. Patients with higher SOCS1 expression were older than those with lower expression (median, 60 years vs 51 years, P=0.032) and less frequently had FAB M1 subtype (P=0.021), and CD7 and CD34 expression on leukemic cells (P=0.019 and P=0.001, respectively, Supplementary Table 2). There was no difference in other variables including sex, hemoglobin levels and platelet counts between the two groups.
Correlation of BM SOCS1 expression with karyotype and molecular gene mutations in the original cohort
Chromosome data were available in 204 patients at diagnosis. The comparison of karyotypes of patients with lower and higher SOCS1 expression was shown in Supplementary Table 3. Patients with higher SOCS1 expression had lower incidence of t(8;21) (P=0.011). There was no association of SOCS1 expression with any other chromosome change. Regarding the molecular gene mutations (Table 1), higher SOCS1 expression was closely associated with NPM1 mutation (33 vs 14.4%, P=0.002) and DNMT3A mutation (22.3 vs 10.8%, P=0.029), and showed a trend to be associated with FLT3/ITD (30.4 vs 19.8%, P=0.089), but was inversely correlated with CEBPAdouble mutation (1.8 vs 14.4%, P=0.001).
Impact of BM SOCS1 expression on response to therapy and clinical outcome in the original cohort
Of the 154 AML patients undergoing conventional intensive induction chemotherapy, 113 (73.4%) patients achieved a CR. The patients with higher SOCS1 expression had a lower probability of achieving CR than those with lower SOCS1 expression (62.5 vs 82.9%, P=0.006). But the relapse rate was similar between the two groups once CR was achieved (P=0.334). After a median follow-up time of 37 months (range 0.5–160), patients with higher SOCS1 expression had a significant shorter OS than those with lower expression (median 20 months vs not reached, P=0.003) (Figure 1a). There was no significant difference in disease-free survival between these two groups (P=0.341). The prognostic differences remained significant among the patients with non-M3 AML (median, 18 months vs not reached, P=0.003, Figure 1b) and those with intermediate-risk cytogenetics (median, 15 months vs not reached, P=0.031, Figure 1c). The same were also true for the subgroup of 77 patients with normal karyotype (median, 18 months vs not reached, P=0.018, Figure 1d). Intriguingly, patients with concurrent higher SOCS1 expression and FLT3/ITD had the worst outcome (Supplementary Figure 1).
Kaplan–Meier survival curves for overall survival stratified by BM SOCS1 messenger RNA (mRNA) expression in the original cohort. Kaplan–Meier survival curves for overall survival in total 154 AML patients (a), non-M3 AML patients (b), patients with intermediate-risk cytogenetics (c) and 77 patients with CN-AML (b and d) who received standard intensive chemotherapy. The median value of BM SOCS1 expression in the original cohort of 223 patients was used as the cut-off point to define lower- and higher-expression groups.
In multivariate analysis (Table 2), the independent poor risk factors for OS were age older than 50 years, white blood cell counts more than 50 000/μl, unfavorable karyotype, RUNX1 mutation and higher SOCS1 expression. Among cytogenetically normal (CN)-AML patients, higher SOCS1 expression was still an independent poor prognostic factor for OS (relative risk 2.41, 95% confidence interval 1.012–5.738, P=0.047, Supplementary Table 4). Intriguingly, the unfavorable prognostic impact of higher SOCS1 expression on OS was lost among the 37 patients receiving allogeneic HSCT, 21 in CR1 (P=0.894). Furthermore, in patients with higher SOCS1 expression, those who received allogeneic HSCT (n=17) had better OS than those who did not (median 27 vs 9 months, P=0.0155). It implies that HSCT may ameliorate the poor survival impact of higher SOCS1 expression. However, further investigations with more patients recruited are needed to verify this point.
The prognostic impact of BM SOSC1 expression in the validation cohort
The median value of SOCS1 expression in the original cohort was used as a cut-off point to define lower- and higher-expression groups in the validation cohort of 73 non-M3 AML patients. After a median follow-up time of 33.3 months (range 0.4–64.3), we found that higher SOCS1 expression was still an unfavorable prognostic factor for OS in non-M3 AML cohort and a trend in CN-AML group (median 15.6 months vs not reached, P=0.007, Supplementary Figure 2A and median 17 months vs not reached, P=0.056, Supplementary Figure 2B, respectively).
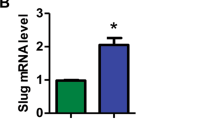
Myeloid cells-specific expression of SOCS1 in transgenic zebrafish
To further investigate the role of SOCS1 in leukemogenesis, we generated the spi1:SOCS1-2A-mCherry/CG2 construct to express SOCS1 and EGFP in zebrafish under the control of the 5.3 kb spi1 (also known as pu.1) and cmlc2 promoter, respectively (Figure 2a). The construct was flanked with the Tol2 transposon element and co-injected with Tol2 transposase messenger RNA into one-cell embryos of an AB-WT background zebrafish to generate spi1:SOCS1-2A-mCherry transgenic fish founder. The transgene expression was demonstrated in F1 zebrafish by visualizing mCherry in the myeloid cells and EGFP in the heart of 24-h post-fertilization (hpf) larva (Figure 2b). In addition, the spi1:SOCS1-2A-mCherry construct was co-injected with mpeg1:EGFP-pA construct. We found that mCherry-positive cells (that is, cells that expressed SOCS1) colocalized with EGFP-positive cells (that is, myeloid cells, Supplementary Figure 3).
Generation of transgenic zebrafish expressing human SOCS1 driven by spi1 promoter. (a) Diagram of the spi1:SOCS1-2A-mCherry/CG2 construct, which contains Tol2 sequences and the cmlc2:EGFP expression cassette. (b) Fluorescent images of spi1:SOCS1-2A-mCherry larva at 24 hpf. The red dots denote SOCS1-expressing myeloid cells and the green denotes fluorescent transgenesis marker in the heart. (c) Semi-quantitative PCR showing the expression of SOCS1 in transgenic larva at 24, 48 and 72 hpf. Actin as an internal control. Positive control: plasmid of spi1:SOCS1-2A-mCherry/CG2, Negative control: non-template.
The expression of SOCS1 RNA in spi1:SOCS1-2A-mCherry transgenic fish was assessed by RT-PCR. SOCS1 expression was shown in F1 transgenic larva at 24, 48 and 72 hpf, but was not observed in WT fish (Figure 2c). We further verified that SOCS1 protein expression was restricted to a small fraction of cells in the KM of 12-month old transgenic fish (Supplementary Figure 4).
Overexpression of SOCS1 enhanced myelopoiesis with leukemic phenotype in transgenic zebrafish
The flow cytometry on whole KM cells from spi1:SOCS1-2A-mCherry transgenic fish at the ages of 9 and 12 months showed a significant increase in the precursor cells compared with those in WT (9 months, 16.79±6.20% vs 5.84±0.4; P<0.001 and 12 months, 20.35±4.23% vs 6.83±1.1; P<0.001) (Figures 3a–f). Microscopic observation of the KM cytospin smears from spi1:SOCS1-2A-mCherry transgenic fish at 9 and 12 months of age also revealed an excess of blast cells with focal aggregation, suggesting leukemia transformation was emerged (Figures 3g and h; Supplementary Table 5). These blast cells in KM were usually of medium to large size, and characterized by a high nuclear–cytoplasmic (N/C) ratio and mildly basophilic cytoplasm with scanty or fewer granules. Further, blasts were observed in PB (Figure 3h). Histopathologic examination showed mild effacement and distortion of kidney structure and increased infiltration of myeloid cells (Figure 4a) compared with WT fish (Figure 4b). Furthermore, mild distortion of spleen structure was found at 12 months of age (Figure 4a). These data indicate that SOCS1 expression in zebrafish leads to the development of myeloid hyperplasia with increased blasts, mimicking leukemic phenotype.
Fluorescence-activated cell sorting analysis and morphological analysis of hematopoietic cells from the kidney marrow or peripheral blood of spi1:SOCS1-2A-mCherry transgenic fish showing increased myelopoiesis with expansion of myeloid precursors at 9 and 12 months of age. (a–d) A total of 30 000 cells from the kidney marrow per animal were analyzed to differentiate various subtypes of hematopoietic cells by flow cytometry. (e and f) The numbers of various subtypes of hematopoietic cells were counted and expressed as mean s.e.m. Gate populations are as follows: immature erythroid, mature erythroid, lymphocytes, myelomonocytes and precursor cells. Mean percentage of cells is indicated for each gated subpopulation. (g and h) Microscopic observation of cytospin smears of the kidney marrow (upper panel) and peripheral blood (lower panel) at 9 months (g) and 12 months (h) showing increased blasts in spi1:SOCS1-2A–mCherry transgenic fish (right), compared with wild-type fish (left). Blasts can be seen in the PB of 12-month transgenic fish (h). Differences among variables were assessed using a Student’s t-test. Significant differences between wild-type and SOCS1 transgenic fish are indicated as follows: *P<0.05; **P<0.01; and ***P<0.001.
Histopathological examination of the kidney marrow, spleen and liver of spi1:SOCS1-2A-mCherry or SOCS1/FLT3-ITD double transgenic fish. (a and b) Hematoxylin and eosin stains of the kidney marrow, spleen and liver from 9- and 12-month old spi1:SOCS1-2A-mCherry transgenic, SOCS1/FLT3-ITD double transgenic and wild-type fish. Kidney marrows from spi1:SOCS1-2A-mCherry transgenic or SOCS1/FLT3-ITD double transgenic fish show increased infiltration by myeloid cells compared with wild-type fish.
A synergistic interaction between SOCS1 expression and FLT3-ITD promoted the expansion of precursor cells in double-hit transgenic fish
On the basis of our findings that higher SOCS1 expression tended to be associated with FLT3/ITD in AML, and patients with both higher SOCS1 expression and FLT3-ITD had poorest prognosis, we generated myeloid-specific expression of SOCS1/FLT3-ITD dTg fish to investigate whether FLT3-ITD could facilitate the leukemogenesis in SOCS1 overexpressing transgenic fish.
As shown by flow cytometric analysis (Supplementary Figures 5A and B) and cytomorphology analysis (Supplementary Figures 5C and D) of the KM and PB smears from 9-month old SOCS1/FLT3-ITD dTg fish, myeloid hyperplasia with much increase of blast cells and depletion of erythroid series were noted in KM (Supplementary Figure 5C; Supplementary Table 5) and appearance of blasts in PB (Supplementary Figure 5D). Moreover, histopathological examination of the kidney from 9-month old SOCS1/FLT3-ITD dTg fish showed mild effacement and distortion of kidney structure, and increased infiltration of myeloid cells (Figure 4a) compared with WT fish (Figure 4b). On the other hand, severe distortion of liver structure was found at 9 months of age (Figure 4a). In addition, 4 (80.0%) out of 5 SOCS1/FLT3-ITD dTg zebrafish had significantly increased precursor cells (18.27±8.39%) and M:E ratio (16.30±8.36%) in KM at 9 months of age, earlier than the time SOCS1 transgenic fish developed the similar picture (12 months, Supplementary Table 5). Moreover, significant difference of groups in the distribution of hematopoietic cells between the 9M-FLT3-ITD or 9M-SOCS1 and 9M-SOCS1/FLT3-ITD dTg zebrafish was observed in morphological analysis (P<0.001, Supplementary Table 5). Altogether, we suggested that FLT3-ITD and SOCS1 expression synergistically promoted myeloid hyperplasia with expansion of precursor cells in zebrafish.
Discussion
A variety of studies demonstrated a role of SOCS1 expression in tumor initiation and progression; however, little is known about the prognostic implication of SOCS1 expression in AML. To the best of our knowledge, this is the first report to demonstrate higher expression of BM SOCS1 is an independent poor prognostic factor for OS in AML patients, irrespective of age, white blood cell counts, karyotype and other genetic markers. The poor prognostic implication of higher SOCS1 expression on OS could also be demonstrated in non-M3 and CN-AML patients.
The mechanisms involved in the regulation of SOCS1 expression include aberrant DNA methylation, gene mutation, loss of heterozygosity and others. Hypermethylation of SOCS1 promoter was frequently identified in various cancers, including multiple myeloma,29 pancreatic cancer,30 hepatocellular carcinoma,31 melanoma32 and so on. We and others also showed 60–72% of AML had SOCS1 methylation by methylation-specific PCR.33, 34 The relationship of SOCS1 methylation and SOCS1 expression may not be positively correlated. Similarly, we could not find the association of SOCS1 methylation and SOCS1 expression in this study (data not shown). Previous studies concerning the relationship between the SOCS1 expression and prognosis in solid cancers showed conflicting results. Decreased SOCS1 expression was correlated with advanced tumor stage and poor outcome in breast cancer and hepatocellular carcinoma,4, 35 supporting its role as a tumor suppressor. On the other hand, overexpression of SOCS1 was associated with tumor invasion and advanced stage in melanoma,5 indicative of tumor-promoting effect. The reasons of the discrepancies of SOCS1 expression on tumor behavior are still unknown. The impact of SOCS1 expression induced by tumor cells on tumor microenvironment may possibly play a role.3 Taken together, SOCS1 may function as either a tumor suppressor or an oncogene dependent on tumor types and microenvironment.
The dual opposite roles of SOCS1 expression in various cancer prompted us to clarify the function and clinical relevance of SOCS1 in AML. In the present study, we distinctly showed that higher SOCS1 expression was associated with a poorer OS in a large cohort of AML patients. The prognostic impact of higher SOCS1 expression was also validated in the independent validation cohort, albeit the patient numbers were limited in that cohort. The underlying mechanisms that higher SOCS1 expression is associated with poor prognosis in AML remain to be determined. Patients with higher SOCS1 expression were more refractory to chemotherapy and had reduced survival, raising the possibility that SOCS1 supports molecular signaling pathways and promotes drug resistance. SOCS1-targeted agent in combination with chemotherapy may be an attracting strategy for the treatment of AML patients with higher expression of this protein. Intriguingly, the poor prognostic impact of SOCS1 in OS was lost if the patients received allogeneic HSCT. In other words, HSCT may ameliorate the poor survival impact of higher SOCS1 expression. Further studies in more patients are needed to clarify this point.
To further investigate the role of SOCS1 in leukemogenesis, we generated the spi1:SOCS1-2A-mCherry transgenic fish. From the age of 9 to 12 months, the SOCS1 transgenic fish showed progressive increase of immature myeloid cells with decreased normal hematopoietic elements. The determination of the leukemia phenotype in this SOCS1 zebrafish model was precisely based on a delicate assessment of morphologic changes in cytospin smears of PB and KM cells and tissue section of KM. The finding is consistent with our clinical observation that higher SOCS1 expression predicts poorer clinical outcomes and supports the assumption that SOCS1 may play as an oncogene in AML patients.
In this study, we found that higher SOCS1 expression was closely associated with FLT3/ITD in AML patients. The survival data further supported a more aggressive course in AML patients with simultaneous higher SOCS1 expression and FLT3/ITD. Interestingly, in a report of Reddy et al.,36 it was shown that co-expression of SOCS1 with FLT3/ITD inhibited interferon-γ signaling and protected FLT3/ITD hematopoietic cells from interferon-mediated growth inhibitory effects. To better delineate the double hits in leukemogenesis, the SOCS1/FLT3-ITD dTg fish was established. In this two-hit fish model, myeloid hyperplasia with proliferation of blast cells in KM and circulating blasts in PB could be detected earlier than SOCS1 or FLT3/ITD single hit fish, suggesting SOCS1 and FLT3-ITD synergistically promoted leukemia transformation in zebrafish. Concerted interaction of these two genetic alterations might play a role in myeloid leukemogenesis. This finding was consistent with the report that SOCS1 expression accelerated the onset of FLT3-ITD induced myeloproliferative neoplasm in the mouse model.36 To the best of our knowledge, this is the first report to demonstrate SOCS1 expression-induced myeloid malignancies in transgenic zebrafish and FLT3-ITD as the second hit could enhance the disease progression. These transgenic fish can potentially provide a valuable platform to investigate leukemogenesis and screen drugs in the near future.
In summary, this study showed that higher SOCS1 expression was closely associated with older age, FLT3/ITD, NPM1 and DNMT3A mutations, but negatively correlated with CEBPA mutation. Further, higher SOCS1 expression was an independent poor prognostic factor for OS in non-M3 and CN-AML patients. The unfavorable prognostic impact of higher SOCS1 expression was also validated in an independent validation cohort. Higher SOCS1 expression may serve as a new biomarker for foreseeing the clinical outcome of AML patients. SOCS1-targeted therapy may represent a potential new approach for AML patients with higher SOCS1 expression.
References
Yoshimura A, Suzuki M, Sakaguchi R, Hanada T, Yasukawa H . SOCS, inflammation, and autoimmunity. Front Immunol 2012; 3: 20.
Beaurivage C, Champagne A, Tobelaim WS, Pomerleau V, Menendez A, Saucier C . SOCS1 in cancer: an oncogene and a tumor suppressor. Cytokine 2016; 82: 87–94.
Zhang J, Li H, Yu JP, Wang SE, Ren XB . Role of SOCS1 in tumor progression and therapeutic application. Int J Cancer 2012; 130: 1971–1980.
Sasi W, Jiang WG, Sharma A, Mokbel K . Higher expression levels of SOCS 1,3,4,7 are associated with earlier tumour stage and better clinical outcome in human breast cancer. BMC Cancer 2010; 10: 178.
Li Z, Metze D, Nashan D, Muller-Tidow C, Serve HL, Poremba C et al. Expression of SOCS-1, suppressor of cytokine signalling-1, in human melanoma. J Invest Dermatol 2004; 123: 737–745.
Roman-Gomez J, Jimenez-Velasco A, Castillejo JA, Cervantes F, Barrios M, Colomer D et al. The suppressor of cytokine signaling-1 is constitutively expressed in chronic myeloid leukemia and correlates with poor cytogenetic response to interferon-alpha. Haematologica 2004; 89: 42–48.
Hou HA, Lin CC, Chou WC, Liu CY, Chen CY, Tang JL et al. Integration of cytogenetic and molecular alterations in risk stratification of 318 patients with de novo non-M3 acute myeloid leukemia. Leukemia 2014; 28: 50–58.
Hou HA, Chou WC, Lin LI, Tang JL, Tseng MH, Huang CF et al. Expression of angiopoietins and vascular endothelial growth factors and their clinical significance in acute myeloid leukemia. Leuk Res 2008; 32: 904–912.
Hou HA, Kuo YY, Liu CY, Chou WC, Lee MC, Chen CY et al. DNMT3A mutations in acute myeloid leukemia: stability during disease evolution and clinical implications. Blood 2012; 119: 559–568.
Tien HF, Wang CH, Lin MT, Lee FY, Liu MC, Chuang SM et al. Correlation of cytogenetic results with immunophenotype, genotype, clinical features, and ras mutation in acute myeloid leukemia: a study of 235 Chinese patients in Taiwan. Cancer Genet Cytogenet 1995; 84: 60–68.
Chou WC, Tang JL, Lin LI, Yao M, Tsay W, Chen CY et al. Nucleophosmin mutations in de novo acute myeloid leukemia: the age-dependent incidences and the stability during disease evolution. Cancer Res 2006; 66: 3310–3316.
Hou HA, Kuo YY, Tang JL, Chou WC, Yao M, Lai YJ et al. Clinical implications of the SETBP1 mutation in patients with primary myelodysplastic syndrome and its stability during disease progression. Am J Hematol 2014; 89: 181–186.
Hou HA, Chou WC, Lin LI, Chen CY, Tang JL, Tseng MH et al. Characterization of acute myeloid leukemia with PTPN11 mutation: the mutation is closely associated with NPM1 mutation but inversely related to FLT3/ITD. Leukemia 2008; 22: 1075–1078.
Lin LI, Chen CY, Lin DT, Tsay W, Tang JL, Yeh YC et al. Characterization of CEBPA mutations in acute myeloid leukemia: most patients with CEBPA mutations have biallelic mutations and show a distinct immunophenotype of the leukemic cells. Clin Cancer Res 2005; 11: 1372–1379.
Tang JL, Hou HA, Chen CY, Liu CY, Chou WC, Tseng MH et al. AML1/RUNX1 mutations in 470 adult patients with de novo acute myeloid leukemia: prognostic implication and interaction with other gene alterations. Blood 2009; 114: 5352–5361.
Falini B, Mecucci C, Tiacci E, Alcalay M, Rosati R, Pasqualucci L et al. Cytoplasmic nucleophosmin in acute myelogenous leukemia with a normal karyotype. N Engl J Med 2005; 352: 254–266.
Hou HA, Huang TC, Lin LI, Liu CY, Chen CY, Chou WC et al. WT1 mutation in 470 adult patients with acute myeloid leukemia: stability during disease evolution and implication of its incorporation into a survival scoring system. Blood 2010; 115: 5222–5231.
Hou HA, Chou WC, Kuo YY, Liu CY, Lin LI, Tseng MH et al. TP53 mutations in de novo acute myeloid leukemia patients: longitudinal follow-ups show the mutation is stable during disease evolution. Blood Cancer J 2015; 5: e331.
Hou HA, Liu CY, Kuo YY, Chou WC, Tsai CH, Lin CC et al. Splicing factor mutations predict poor prognosis in patients with de novo acute myeloid leukemia. Oncotarget 2016; 7: 9084–9101.
Shiah HS, Kuo YY, Tang JL, Huang SY, Yao M, Tsay W et al. Clinical and biological implications of partial tandem duplication of the MLL gene in acute myeloid leukemia without chromosomal abnormalities at 11q23. Leukemia 2002; 16: 196–202.
Chou WC, Hou HA, Chen CY, Tang JL, Yao M, Tsay W et al. Distinct clinical and biologic characteristics in adult acute myeloid leukemia bearing the isocitrate dehydrogenase 1 mutation. Blood 2010; 115: 2749–2754.
Lin CC, Hou HA, Chou WC, Kuo YY, Liu CY, Chen CY et al. IDH mutations are closely associated with mutations of DNMT3A, ASXL1 and SRSF2 in patients with myelodysplastic syndromes and are stable during disease evolution. Am J Hematol 2014; 89: 137–144.
Chou WC, Chou SC, Liu CY, Chen CY, Hou HA, Kuo YY et al. TET2 mutation is an unfavorable prognostic factor in acute myeloid leukemia patients with intermediate-risk cytogenetics. Blood 2011; 118: 3803–3810.
Lu JW, Hsieh MS, Liao HA, Yang YJ, Ho YJ, Lin LI . Zebrafish as a model for the study of human myeloid malignancies. Biomed Res Int 2015; 2015: 641475.
Lu JW, Hou HA, Hsieh MS, Tien HF, Lin LI . Overexpression of FLT3-ITD driven by spi-1 results in expanded myelopoiesis with leukemic phenotype in zebrafish. Leukemia 2016; 30: 2098–2101.
Lin HF, Traver D, Zhu H, Dooley K, Paw BH, Zon LI et al. Analysis of thrombocyte development in CD41-GFP transgenic zebrafish. Blood 2005; 106: 3803–3810.
Cheson BD, Bennett JM, Kopecky KJ, Buchner T, Willman CL, Estey EH et al. Revised recommendations of the International Working Group for Diagnosis, Standardization of Response Criteria, Treatment Outcomes, and Reporting Standards for Therapeutic Trials in Acute Myeloid Leukemia. J Clin Oncol 2003; 21: 4642–4649.
Tsai CH, Hou HA, Tang JL, Liu CY, Lin CC, Chou WC et al. Genetic alterations and their clinical implications in older patients with acute myeloid leukemia. Leukemia 2016; 30: 1485–1492.
Galm O, Yoshikawa H, Esteller M, Osieka R, Herman JG . SOCS-1, a negative regulator of cytokine signaling, is frequently silenced by methylation in multiple myeloma. Blood 2003; 101: 2784–2788.
Komazaki T, Nagai H, Emi M, Terada Y, Yabe A, Jin E et al. Hypermethylation-associated inactivation of the SOCS-1 gene, a JAK/STAT inhibitor, in human pancreatic cancers. Jpn J Clin Oncol 2004; 34: 191–194.
Okochi O, Hibi K, Sakai M, Inoue S, Takeda S, Kaneko T et al. Methylation-mediated silencing of SOCS-1 gene in hepatocellular carcinoma derived from cirrhosis. Clin Cancer Res 2003; 9: 5295–5298.
Liu S, Ren S, Howell P, Fodstad O, Riker AI . Identification of novel epigenetically modified genes in human melanoma via promoter methylation gene profiling. Pigment Cell Melanoma Res 2008; 21: 545–558.
Chen CY, Tsay W, Tang JL, Shen HL, Lin SW, Huang SY et al. SOCS1 methylation in patients with newly diagnosed acute myeloid leukemia. Genes Chromosomes Cancer 2003; 37: 300–305.
Watanabe D, Ezoe S, Fujimoto M, Kimura A, Saito Y, Nagai H et al. Suppressor of cytokine signalling-1 gene silencing in acute myeloid leukaemia and human haematopoietic cell lines. Br J Haematol 2004; 126: 726–735.
Yoshikawa H, Matsubara K, Qian GS, Jackson P, Groopman JD, Manning JE et al. SOCS-1, a negative regulator of the JAK/STAT pathway, is silenced by methylation in human hepatocellular carcinoma and shows growth-suppression activity. Nat Genet 2001; 28: 29–35.
Reddy PN, Sargin B, Choudhary C, Stein S, Grez M, Muller-Tidow C et al. SOCS1 cooperates with FLT3-ITD in the development of myeloproliferative disease by promoting the escape from external cytokine control. Blood 2012; 120: 1691–1702.
Acknowledgements
This work was partially sponsored by grants MOST 100-2628-B-002-003-MY3, 103-2628-B-002-008-MY3, 104-2923-B-002-001 and 104-2314-B-002-128 -MY4 from the Ministry of Science and Technology (Taiwan), MOHW105- TDU-B-211-134005 from the Ministry of Health and Welfare (Taiwan) and NTUH 102P06 from the Department of Medical Research, National Taiwan University Hospital. We would like to acknowledge the service provided by the DNA Sequencing Core of the First Core Laboratory, National Taiwan University College of Medicine and the Flow Cytometric Analyzing and Sorting Core Facility at National Taiwan University Hospital. We also would like to thank the Taiwan Zebrafish Core Facility at NHRI for providing fish lines and resources.
Author contributions
H-AH was responsible for study design, plan and coordination, literature collection, data management and interpretation, statistical analysis and manuscript writing; J-WL was responsible for study plan, data management and interpretation, statistical analysis and manuscript writing; C-YL was responsible for statistical analysis and interpretation of the statistical findings; H-A.H, W-CC, C-CL, ZG, J-LT and H-FT contributed patient samples and clinical data; T-YL, Y-YK, M-HT, Y-LP and Y-CC performed the gene mutation studies, and H-FT and L-IL planned, designed and coordinated the study over the entire period, and wrote the manuscript. All authors read and approved the final manuscript.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Blood Cancer Journal website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/4.0/
About this article
Cite this article
Hou, HA., Lu, JW., Lin, TY. et al. Clinico-biological significance of suppressor of cytokine signaling 1 expression in acute myeloid leukemia. Blood Cancer J. 7, e588 (2017). https://doi.org/10.1038/bcj.2017.67
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bcj.2017.67
This article is cited by
-
Zebrafish ELL-associated factors Eaf1/2 modulate erythropoiesis via regulating gata1a expression and WNT signaling to facilitate hypoxia tolerance
Cell Regeneration (2023)
-
Zebrafish: a convenient tool for myelopoiesis research
Cell Regeneration (2023)
-
In-silico comparison of two induction regimens (7 + 3 vs 7 + 3 plus additional bone marrow evaluation) in acute myeloid leukemia treatment
BMC Systems Biology (2019)