Abstract
Mutation of the fms-like tyrosine kinase 3-internal tandem duplication (FLT3-ITD), which is one of the most frequent genetic alterations, strongly contributes to an increased risk of treatment failure and to poor prognosis. In this study, we established quantitative fragment analysis of FLT3-ITD simultaneously measuring mutant allele burden and length, verified the analytical performance and evaluated the clinical significance in adult acute myeloid leukemia (AML) patients. FLT3-ITD was detected in 73 of 363 adult AML patients (20.1%) and high mutant allelic burden (⩾50%, n=13) and long ITD length (⩾70 base pairs, n=15) were significantly associated with inferior overall survival (OS; P=0.002 and 0.005, respectively) and event-free survival (EFS; P=0.004 and 0.007, respectively). FLT3-ITD poor prognostic group was identified as patients with high allele burden or long ITD length (n=24), which revealed significant adverse clinical outcome for both OS (P<0.001) and EFS (P<0.001). In cytogenetically normal AML, even FLT3-ITD low allele burden and short length was associated with poorer OS (P=0.037) and EFS (P=0.044) than wild type, whose influence was overcome when hematopoietic stem cell transplantation was performed. In minimal residual disease monitoring, FLT3-ITD negativity after consolidation therapy was a valuable predictor of better OS (P<0.001) and EFS (P<0.001). FLT3-ITD poor prognostic group with high mutant allele burden or long ITD length is efficiently identified by quantitative fragment analysis.
Similar content being viewed by others
Introduction
Mutation of the fms-like tyrosine kinase 3 gene consisting of internal tandem duplication (FLT3-ITD), which is one of the most frequent genetic alterations, occurs in 15–35% of adults with acute myeloid leukemia (AML).1, 2 Many studies have reported that the FLT3-ITD mutation strongly contributes to an increased risk of treatment failure and to a poor prognosis.3, 4 Detection of ITD mutations at diagnosis is now a routine clinical practice to provide guidance of optimal treatment for AML patients. Currently, most AML patients with ITD mutations need hematopoietic stem cell transplantation (HSCT).5, 6
FLT3-ITD mutations are amenable to PCR-based molecular diagnostic DNA testing because they are limited to a small, predictable region of the FLT3 gene. PCR amplification followed by fragment analysis is a rapid, sensitive and specific method that is commonly used. This method is able to detect mutant allele burden and changes in the length of ITD simultaneously.
Despite the evident poor outcome associated with the FLT3-ITD mutation, it is unclear whether this can be explained simply by the presence or absence of the abnormality, or whether other factors including mutant allele burden or mutant length influence its prognostic impact. A high total mutant level (more than 50%) revealed significantly worse clinical outcome.7 A recent study showed that minor mutants with a low allele burden can be clinically significant because they may become a dominant clone at the later refractory status.8 Persistence of FLT3-ITD minimal residual disease (MRD) after induction chemotherapy are predictive of complete remission duration.9 But in another study FLT3 allele burden had no significant influence on outcomes after correcting for other variables.10 The meaning of the length of FLT3-ITD is also still debatable. In one study, mutant length and number had no significant impact on outcome,7 whereas others reported that patients with shorter ITDs have a lower relapse rate and more favorable outcome than those with longer ITDs.11, 12, 13 It is therefore necessary to clarify the significance of those indicators to determine the ideal treatment modality in AML with FLT3-ITD.
In this study, we measured the relative mutant allele burden and length of FLT3-ITD using fragment analysis and verified the analytical performance. The clinical significance was investigated in ITD mutants with allele burden and length to define risk groups in adult AML.
Materials and Methods
Patients and samples
Adult patients (n=363) diagnosed with de novo AML in Seoul St Mary’s Hospital were included in the study. Diagnosis of AML was determined according to the 2008 World Health Organization classifications. The median age of 191 males and 172 females was 51 years (range, 15–85 years). Median follow-up was 31 months from initial presentation (range, 11.3–56.6 months). Patients were immunophenotyped using flow cytometric analyses. Cytogenetic analysis was performed using bone marrow (BM) specimen and classified based on National Comprehensive Cancer Network 2014 guidelines. Serial follow-up BM samples after treatment were available from 42 patients whose FLT3-ITD results were positive at diagnosis. DNA isolated from the peripheral blood or BM of 50 normal donors was used to analyze method specificity. According to the Declaration of Helsinki, all patients and donors in this study provided written informed consent for genetic analyses. The study protocol was approved by the Institutional Review Board of Seoul St Mary’s Hospital, The Catholic University of Korea.
Fragment analysis for FLT3-ITD
Genomic DNAs were extracted from the BM aspirates with the QIAamp DNA Mini Kit (Qiagen, Hamburg, Germany). The DNA was quantified spectrophotometrically using a ND-1000 apparatus (Nanodrop Technologies, Wilmington, DE, USA). PCR for fragment analysis to detect an ITD mutation was performed using a modified protocol based on that previously described.14 The functional domains of FLT3 gene (Gene Bank Accession NM_004119.2) were PCR-amplified with forward primers 5′ end labeled with fluorescent dye. The PCR products were analyzed using a model 3130XL genetic analyzer (Applied Biosystems, Foster City, CA, USA) and the amplicons with a size greater than that of wild type (328±1 bases) were interpreted as positive for the ITD mutation. The number, area and length of mutant peaks on the electropherogram were analyzed using GeneMapper analysis software (Applied Biosystems). The FLT3-ITD mutant allelic burden was calculated as the ratio of the area under the curve of mutant and wild-type alleles (mutant/total FLT3). All tests were duplicated. Specificity was evaluated using DNA samples derived from 50 normal donors. No false positivity was identified. Mutant plasmid DNA was prepared by cloning and the detection sensitivity was defined as 10 copies of mutant plasmid DNA. Analytical sensitivity was analyzed using serial mixtures of mutant and wild-type plasmid DNA. Limit of detection was calculated by Probit analysis at 95% detection level as 3% of mutant allele burden. A strict linear correlation was observed with correlation coefficient (r2) of 0.99.
Treatment courses
Of the 363 patients, 30 opted for conservative treatment, and 333 were treated according to our standard induction chemotherapeutic regimens. Briefly, 152 (45.6%) were treated with 3+7 idarubicin (IDA) plus N4-behenoyl-1-β-d-arabinofuranosyl cytosine (BHAC)15 as remission induction chemotherapy. IDA was administered daily at a dose of 12 mg/m2 intravenous for 3 consecutive days, and BHAC was administered daily at 300 mg/m2 for 7 consecutive days. A total of 137 patients (41.1%) were treated with 3+7 IDA plus cytosine arabinoside (ARA-C) at a dose of 100 mg/m2. Forty four patients (13.2%) were treated with modified low-dose ARA-C (20 mg/m2 every 12 h) combined with oral etoposide, 100 mg for 14 consecutive days.16
A total of 245 patients (67.5%) achieved complete remission (CR) after first cycle of induction chemotherapy. After achievement of CR, one or two consolidation chemotherapy was administered, or patients who were not in CR after 1st induction chemotherapy were treated by re-induction chemotherapy. The standard consolidation chemotherapy consisted of ‘3+5’ mitoxantrone (12 mg/m2 intravenous) plus intermediate-dose ARA-C (1.0 g/m2 intravenous b.i.d.) or IDA (12 mg/m2) plus intermediate-dose ARA-C, applied alternatively. Seventy six patients relapsed or died during chemotherapy and 257 patients received final treatment (that is, allo-HSCT, autologous (auto)-HSCT or at least two cycles of consolidation chemotherapy after induction chemotherapy). Among these 257 patients, 183 had variable allo-HSCT courses. Eighty eight patients with an available human leukocyte antigen-matched sibling donor and 36 patients with a partially matched (<2 allele mismatched) unrelated donor underwent allo-HSCT. Thirty six patients received a haploidentical familial mismatched transplant.
As a reduced-intensity conditioning regimen, we administered busulfex 6.4 mg/kg and fludarabine 150 mg/m2 with 400 cGy total body irradiation (TBI). The myeloablative conditioning regimen included cyclophosphamide 120 mg/kg combined with 1320 cGy TBI or busulfex 12.8 mg/kg. Familial mismatched transplant comprised busulfex 6.4 mg/kg, fludarabine 150 mg/m2 and 800 cGy TBI with antithymocyte globulin (1.25 mg/day) for 4 days.17 If a patient achieved CR and did not have a suitable donor, we also considered auto-HSCT in 15 young patients (age <60 years) with a myeloablative conditioning regimen consisting of ARA-C 9 g/m2, melphalan 100 mg/m2 and 1200 cGy TBI.18 The remaining 55 patients were treated with chemotherapy alone.
Definition of clinical end points
Achievement of CR was defined as a normocellular BM containing <5% leukemic blasts and showing normal maturation of all cell lineages. In addition, recovery of neutrophils 1500/μl and platelets >100 000/μl in peripheral blood was mandatory, as well as no evidence for circulating blasts and/or extramedullary leukemia. Relapse was defined as reoccurrence of >5% of leukemic blasts in BM, reappearance of circulating blasts or the development of extramedullary leukemia.19 Overall survival (OS) was defined as the time from diagnosis to death or date last known alive. Event-free survival (EFS) was defined as the time from diagnosis to relapse for patients who experienced a relapse, time to death for non-relapsed patients who did not survive or time to last follow-up for surviving patients who did not experience a relapse.
Statistical analyses
Differences in clinical variables according to mutation status were investigated using Fisher’s exact test for categorical variables and the Mann–Whitney U-test for continuous variables. OS and EFS probabilities were calculated using the Kaplan–Meier survival analysis and the differences in survival curves were compared using a two-sided log-rank test. Cox proportional hazard models were used to estimate hazard ratios for univariate and multivariate analyses for OS and EFS. To extract independent events, those with a P-value ⩽0.20 were analyzed using the forward stepwise model selection procedure. All statistical analyses were performed using SPSS 12.0.1 for Windows (SPSS Inc., Chicago, IL, USA). A two-sided P-value <0.05 was used to assess statistical significance.
Results
Detection of FLT3-ITD with fragment analysis
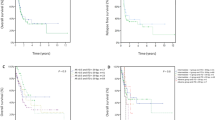
The main characteristics of patients are summarized in Table 1. FLT3-ITD was identified in 73 of 363 adult AML patients (20.1%) and 71 patients (97.3%) had a single ITD and two patients had double ITDs at diagnosis. Presence of ITDs were associated with higher white blood cell count (median of 45.9 × 109/l vs 5.3 × 109/l; P<0.001) and higher peripheral blood blast percentage (median of 74 vs 24.5%, P<0.001), higher BM blast percentage (median of 86 vs 70%; P<0.001). FLT3-ITD were more common in patients with normal karyotypes (frequency, 29.5 vs 10.6%; P<0.001) and NPM1 mutation (frequency 37.0 vs 2.4%; P<0.001). CR rates were not significantly different between patients with or without FLT3-ITDs (P=0.214). OS was somewhat poorer for FLT3-ITD-positive patients (estimated median OS (95% CI) 10.7 months (8.7–12.7) vs 19.4 months (12.9–25.9)) (P=0.058) compared with FLT3-ITD-negative patients. EFS was poorer for FLT3-ITD-positive patients (estimated median EFS (95% CI) 6.6 months (3.8–9.4) vs 13.0 months (6.8–19.1)) (P=0.032; Figure 1a).
Characteristics and clinical significance of FLT3-ITD mutant allele burden and length
FLT3-ITD mutant allele burden
The allelic burden of the ITD mutant in each patient ranged from 2.3 to 75.2% with a median of 32.9% (Table 2). According to the distribution of mutant allele burden and a previous study,7 we grouped patients with ⩾50% as high mutant allele burden. Thirteen patients (17.8%) were included in the high mutant allele burden group and 60 patients in the low mutant allele group (Supplementary Table S1). The mutant allele burden was associated with OS (estimated median OS of 7.2 months (5.7–8.6), 11.5 months (3.5–19.5) and 19.4 months (12.9–25.9); P<0.001) and EFS with estimated median EFS 4.8 months (0.0–11.8), 8.1 months (2.4–13.8) and 13.0 months (6.8–19.1); P=0.002) in FLT3-ITD high, low and wild type, respectively (Figure 1b).
FLT3-ITD mutant length
We next examined whether ITD length had an impact on clinical outcome. The length of the ITDs ranged from 16 to 150 base pairs (bp) with a median of 50 bp. The distribution of mutant length suggested two groups containing cases of less than 70 bp (n=57, 79.5%) and longer length with 70 bp or more (n=15). FLT3-ITD length was not significantly correlated with age, white blood cell count, peripheral blood blast percentage, BM blast percentage or ITD mutant allele burden. Treatment outcomes were related with ITD length. ITDs exceeding 70 bp in length were associated with decreasing OS, with an estimated median OS 6.4 months (2.7–10.1) compared with shorter ITDs (11.5 months (2.5–20.5)) and FLT3 wild type (19.4 months (12.9–25.9; P=0.005)). Likewise, EFS tended to decrease in patients with long ITD with estimated median EFS as 4.2 months (1.5–6.9) compared with shorter ITDs and FLT3 wild type, which had a median EFS of 8.1 months (2.7–13.5) and 13.0 months (6.8–19.1; P=0.007; Figure 1c).
Identification of FLT3-ITD poor prognostic group
As a high mutant allele burden (⩾50%) and long ITD length (⩾70 bp) were associated with worse clinical outcomes, we considered patients with either high mutant allele burden or long ITD length as one independent prognostic group. Therefore, we identified them as the FLT3-ITD poor prognostic group. Twenty four patients were included in the group because only four cases had both high allele burden and long ITD length. Notably, 22 of 24 patients died during follow-up (91.7%). The FLT3-ITD poor prognostic group demonstrated decreasing OS (7.2 months (5.4–9.0)) compared with the other FLT3-ITD-positive patients (low allele burden and short ITD length) (18.9 months (7.5–30.3)) and wild type (19.4 months (12.9–25.9); P<0.001) and EFS (4.8 months (2.4–7.2)) than the other FLT3-ITD-positive patients (11.0 months (7.4–14.6)) and wild type (13.0 months (6.8–19.1); P<0.001) (Figure 1d).
The FLT3-ITD high allele burden or long ITD length remained a significant adverse prognostic factor for both OS and EFS. Cox multivariate analysis, with the variables considered being age, sex, white blood cell count, National Comprehensive Cancer Network cytogenetic risk status and NPM1 mutation (Table 3). The influence of FLT3-ITD high allele burden or long ITD length on clinical outcomes was remained even when the analysis was limited to patients receiving HSCT.
Clinical significance of FLT3-ITD in cytogenetically normal AML
Next, the analysis was restricted to patients with cytogenetically normal (CN) AML (n=183) because the influence of FLT3-ITD is most strong in CN-AML, which is re-classified as poor-risk category when ITD is accompanied. In CN-AML, FLT3-ITD poor prognostic group (n=19) revealed inferior clinical outcome (median OS 7.2 months, P<0.001; median EFS 5.3 months, P<0.001) as like in entire patients. Interestingly, even patients with FLT3-ITD low allele burden and short length (n=35) showed poor OS (median 39.4 vs 11.1 months, P=0.037) and EFS (median 24.9 vs 8.1 months, P=0.044) when compared with FLT3 wild-type patients. However, patients with FLT3-ITD low allele burden and short length did not show significantly different OS (P=0.329) and EFS (P=0.288) rates compared with FLT3-ITD wild-type CN-AML when the analysis was restricted in HSCT-performed CN-AML patients (n=112; Figure 2). These results indicated that the influence of the prognostic impact of FLT3-ITD was overcome when HSCT was performed except FLT3-ITD poor prognostic group.
MRD monitoring using FLT3-ITD with fragment analysis
Considerable effort has been directed at identifying molecular markers that can be used to detect residual disease or predict relapse at an earlier stage and lead to therapeutic intervention before overt hematological relapse occurs. Presently, the utility of FLT3-ITD mutant allele burden was evaluated by fragment analysis as a MRD marker. Forty two patients with FLT3-ITD were serially followed during treatment. FLT3-ITD negativity was demonstrated after consolidation therapy in 28 (66.7%) patients. Initial ITD allele burden (median 35.5%, 6.6–74.6% at diagnosis) was dramatically decreased after induction therapy (median 0%, 0–27.4%) and was not detectable after consolidation. Patients with detectable ITD by fragment analysis (MRD positivity, n=14) revealed transient decrement of ITD mutant allele level after induction (11.0±19.2%), which was increased after consolidation therapy (Figure 3). MRD negativity after consolidation therapy was also a valuable predictor of better OS (40.0 vs 12.4 months, P<0.001) and EFS (37.4 vs 4.8 months, P<0.001). Among patients who achieved hematological CR (n=36), nine had detectable ITD during follow-up. Of note, all nine were relapsed or died. The other 27 patients maintained FLT3-ITD negativity during the 12-month follow-up. Relapsed patients retained identical FLT3-ITD mutations that were harbored at diagnosis except for one patient who gained another new ITD at the time of relapse. In a patient with two ITD-positive mutants at initial diagnosis, a minor mutant with an allelic burden of 40.1% became the dominant mutant, with an allelic burden of 64.1% at the time of relapse.
Discussion
FLT3-ITD heralds a poor prognosis in AML. However, the risk conferred by FLT3-ITD mutation remains to be determined whether specific characteristics, such as the allelic burden, length of the mutation or specific sequence as well as the presence of absence of ITD are related. It should be defined preferentially to draw up adequate therapeutic plan for each patient. The present study was performed with the two aims. The first was to determine the specific characteristics of FLT3-ITD associated with clinical outcomes. The second was to evaluate the fragment analysis, which is commonly used technique because of its convenience, is acceptable to test FLT3-ITD in routine laboratory.20
On the basis of the results from this study, the presence or absence of FLT3-ITD did not properly predict patient outcome. The mutant allele burden was more predictable for prognosis when the cutoff was determined as 50%. The 50% cutoff value is consistent with the observation that higher levels are indicative of the presence of biallelic disease, at least in some cells. The mutant allele burden in patients with leukemia is one of the most important features modulating the prognostic impact of the mutation.7, 21, 22 Prognostic relevance of FLT3-ITD allele burden might be based on biological grounds: highest FLT3-ITD corresponds to a homozygous state, usually because of a process of uniparental disomy, whereas a low ITD burden might have arisen in a minor subclone, perhaps occurring at a later stage of the leukemogenic process.23
This study also suggests that ITD length may be important in disease prognosis. We set the cutoff as 70 bp on the basis of the distribution of the length and the simulation of the effect on patients’ outcome. These data suggest that the long ITDs are associated with a worse OS and EFS. Whether it is the length of the ITD or the involvement of specific residues remains to be clarified. It is possible that longer ITDs may involve multiple functional domains and more effectively disrupt the autoinhibitory regulation of the kinase activity.11, 12
Because the high mutant allele burden and long ITD length were proved to be poor prognostic factors, we considered patients with at least one of them as FLT3-ITD poor prognostic group. Only four cases overlapped, so that the number of cases in this group was nearly double compared with each group. Patients in the FLT3-ITD poor prognostic group had an inferior clinical outcome even though HSCT was performed, because relapse after HSCT occurs frequently.24 The prognostic factor might help guide early intervention with a strategy, such as FLT3 inhibition and/or alteration in graft versus host disease prophylaxis in patients at high risk of relapse.25
Little is known about the significance of a low allele burden and short length in FLT3-ITD mutation. Patients with low ITD allele burden and NPM1 mutation were reported to show a similar prognostic impact to FLT3 wild-type AML, whereas those with low ITD and wild-type NPM1 had a higher risk of relapse and shortened OS than FLT3 wild-type patients.26 To investigate the potential effect of low allele burden and short length of FLT3-ITD, we evaluated the prognostic impact of FLT3-ITD in restricted to CN-AML. Patients with FLT3-ITD low allele burden and short length had poorer OS and EFS compared with FLT3 wild type. The prognostic impact of FLT3-ITD low allele burden and short length was overcome when HSCT was performed, whereas not in the FLT3-ITD poor prognostic group. These results support the view that comprehensive evaluation of FLT3-ITD mutation and cytogenetic risk group might help identify patients who benefit from early allogeneic HSCT.
CR after chemotherapy and post-transplant remission in AML patients has been assessed using BM morphology as well as hematologic recovery. Morphologic evaluations are insensitive and better methods are needed to assess MRD in AML patients. FLT3-ITDs may provide an adequate MRD marker for nearly 25% of AML patients especially in CN-AML.27 However, whether FLT3 mutational status is an adequate marker for MRD has been questioned, given that FLT3 status can change over time.28, 29 Although a relapsed patient with emerging new clone and a patient showing shift of dominant clone were identified in this study, such alterations are not common. When relapse occurs in patients harboring the FLT3-ITD mutation at diagnosis, the mutation is present in most cases. In addition, our results confirm that FLT3 positivity after consolidation therapy predicts treatment failure or relapse. Therefore, molecular FLT3-ITD monitoring is useful to assess MRD in those patients. Nine patients showed detectable ITDs in hematologic CR stuatus, which was regarded as incomplete molecular CR status. In those patients, more intensive chemotherapy, including early HSCT can be a replaceable solution instead of routine consolidation protocol.
In the view of analytical technique, a standard PCR assay using primers that straddle the ITD mutation has been developed to detect length-altering mutations of ITD.30 Amplicons with a size greater than that of wild type and labeled with both fluorochromes are interpreted as positive for ITD mutation. The advantage of ITD assay using fragment analysis is that this method is able to detect the allelic burden of wild-type and mutant FLT3, multiple clonality and length of ITD simultaneously without extra labor. The detection sensitivity is about 5% of the mutant allele burden30 and we also observed a similar limit of detection (~3%). The limitation of this method for quantification is that the wild-type allele being amplified at a more rapid rate than the mutant allele during PCR. This PCR bias affects the accuracy of mutant allele burden, so that long ITD mutant is measured to lower level than expected. We tried to minimize this bias by the modification of PCR cycle and confirmed the accuracy of the method using standardized material resulted in excellent linearity and high concordance rate. Continuous FLT3-ITD monitoring in patients achieving molecular remission demonstrated that MRD-negative status retained during the 12 months follow-up. Therefore, fragment analysis is useful technique for MRD monitoring.
Finally, our findings indicate that FLT3-ITD poor prognostic group with high mutant allele burden or long ITD length is efficiently identified by quantitative fragment analysis. In addition, FLT3-ITD is quite useful for MRD monitoring to detect incomplete remission or early relapse in molecular level. This FLT3-ITD analysis is capable of guiding clinical decision making, potentially including the use of another treatment modality such as FLT3 inhibitors.
References
Döhner H, Estey EH, Amadori S, Appelbaum FR, Büchner T, Burnett AK et al. Diagnosis and management of acute myeloid leukemia in adults: recommendations from an international expert panel, on behalf of the European LeukemiaNet. Blood 2010; 115: 453–474.
Schlenk RF, Döhner K, Krauter J, Fröhling S, Corbacioglu A, Bullinger L et al. Mutations and treatment outcome in cytogenetically normal acute myeloid leukemia. N Engl J Med 2008; 358: 1909–1918.
Meshinchi S, Woods WG, Stirewalt DL, Sweetser DA, Buckley JD, Tjoa TK et al. Prevalence and prognostic significance of Flt3 internal tandem duplication in pediatric acute myeloid leukemia. Blood 2001; 97: 89–94.
Schnittger S, Schoch C, Dugas M, Kern W, Staib P, Wuchter C et al. Analysis of FLT3 length mutations in 1003 patients with acute myeloid leukemia: correlation to cytogenetics, FAB subtype, and prognosis in the AMLCG study and usefulness as a marker for the detection of minimal residual disease. Blood 2002; 100: 59–66.
O’Donnell MR, Tallman MS, Abboud CN, Altman JK, Appelbaum FR, Arber DA et al. Acute myeloid leukemia, version 2. J Natl Compr Canc Netw 2013; 11: 1047–1055.
Estey EH . Acute myeloid leukemia: 2013 update on risk-stratification and management. Am J Hematol 2013; 88: 318–327.
Gale RE, Green C, Allen C, Mead AJ, Burnett AK, Hills RK et al. The impact of FLT3 internal tandem duplication mutant level, number, size, and interaction with NPM1 mutations in a large cohort of young adult patients with acute myeloid leukemia. Blood 2008; 111: 2776–2784.
Beierl K, Tseng LH, Beierl R, Haley L, Gocke CD, Eshleman JR et al. Detection of minor clones with internal tandem duplication mutations of FLT3 gene in acute myeloid leukemia using delta-PCR. Diagn Mol Pathol 2013; 22: 1–9.
Abdelhamid E, Preudhomme C, Helevaut N, Nibourel O, Gardin C, Rousselot P et al. Minimal residual disease monitoring based on FLT3 internal tandem duplication in adult acute myeloid leukemia. Leuk Res 2012; 36: 316–323.
How J, Sykes J, Gupta V, Yee KW, Schimmer AD, Schuh AC et al. Influence of FLT3-internal tandem duplication allele burden and white blood cell count on the outcome in patients with intermediate-risk karyotype acute myeloid leukemia. Cancer 2012; 118: 6110–6117.
Meshinchi S, Stirewalt DL, Alonzo TA, Boggon TJ, Gerbing RB, Rocnik JL et al. Structural and numerical variation of FLT3/ITD in pediatric AML. Blood 2008; 111: 4930–4933.
Stirewalt DL, Kopecky KJ, Meshinchi S, Engel JH, Pogosova-Agadjanyan EL, Linsley J et al. Size of FLT3 internal tandem duplication has prognostic significance in patients with acute myeloid leukemia. Blood 2006; 107: 3724–3726.
Choi Y, Kim HJ, Park BH, Min WS, Kim CC . Novel mutations in the FLT3 gene in adult patients with refractory acute myeloid leukemia. Leukemia 2005; 19: 141–143.
Zwaan CM, Meshinchi S, Radich JP, Veerman AJ, Huismans DR, Munske L et al. FLT3 internal tandem duplication in 234 children with acute myeloid leukemia: prognostic significance and relation to cellular drug resistance. Blood 2003; 102: 2387–2394.
Park HS, Kim DW, Kim CC, Kim HK, Kim JS, Hwang TJ et al. Induction chemotherapy with idarubicin plus N4-behenoyl-1-beta-D-arabinofuranosylcytosine in acute myelogenous leukemia: a newly designed induction regimen—a prospective, cooperative multicenter study. Semin Hematol 1996; 33: 24–29.
Yoon JH, Cho BS, Kim HJ, Kim JH, Shin SH, Yahng SA et al. Outcomes of elderly de novo acute myeloid leukemia treated by a risk-adapted approach based on age, comorbidity, and performance status. Am J Hematol 2013; 88: 1074–1081.
Yahng SA, Kim JH, Jeon YW, Yoon JH, Shin SH, Lee SE et al. A well-tolerated regimen of 800 cGy TBI-fludarabine-busulfan-ATG for reliable engraftment after unmanipulated haploidentical peripheral blood stem cell transplantation in adult patients with acute myeloid leukemia. Biol Blood Marrow Transplant 2015; 21: 119–129.
Kim HJ, Min WS, Eom KS, Park SJ, Park YH, Kim DW et al. Autologous stem cell transplantation using modified TAM or combination of triple-alkylating agents conditioning regimens as one of the post-remission treatments in patients with adult acute myeloid leukemia in first complete remission. Bone Marrow Transplant 2004; 34: 215–220.
Cheson BD, Cassileth PA, Head DR, Schiffer CA, Bennett JM, Bloomfield CD et al. Report of the National Cancer Institute-sponsored workshop on definitions of diagnosis and response in acute myeloid leukemia. J Clin Oncol 1990; 8: 813–819.
Levis M . FLT3 mutations in acute myeloid leukemia: what is the best approach in 2013? Hematology Am Soc Hematol Educ Program 2013; 2013: 220–226.
Whitman SP, Archer KJ, Feng L, Baldus C, Becknell B, Carlson BD et al. Absence of the wild-type allele predicts poor prognosis in adult de novo acute myeloid leukemia with normal cytogenetics and the internal tandem duplication of FLT3: a cancer and leukemia group B study. Cancer Res 2001; 61: 7233–7239.
Thiede C, Steudel C, Mohr B, Schaich M, Schäkel U, Platzbecker U et al. Analysis of FLT3-activating mutations in 979 patients with acute myelogenous leukemia: association with FAB subtypes and identification of subgroups with poor prognosis. Blood 2002; 99: 4326–4335.
Levis M . FLT3/ITD AML and the law of unintended consequences. Blood 2011; 117: 6987–6990.
Brunet S, Labopin M, Esteve J, Cornelissen J, Socié G, Iori AP et al. Impact of FLT3 internal tandem duplication on the outcome of related and unrelated hematopoietic transplantation for adult acute myeloid leukemia in first remission: a retrospective analysis. J Clin Oncol 2012; 30: 735–741.
Grunwald MR, Tseng LH, Lin MT, Pratz KW, Eshleman JR, Levis MJ et al. Improved FLT3 internal tandem duplication PCR assay predicts outcome after allogeneic transplant for acute myeloid leukemia. Biol Blood Marrow Transplant 2014; 20: 1989–1995.
Pratcorona M, Brunet S, Nomdedéu J, Ribera JM, Tormo M, Duarte R et al. Favorable outcome of patients with acute myeloid leukemia harboring a low-allelic burden FLT3-ITD mutation and concomitant NPM1 mutation: relevance to post-remission therapy. Blood 2013; 121: 2734–2738.
Stirewalt DL, Willman CL, Radich JP . Quantitative, real-time polymerase chain reactions for FLT3 internal tandem duplications are highly sensitive and specific. Leuk Res 2001; 25: 1085–1088.
Nazha A, Cortes J, Faderl S, Pierce S, Daver N, Kadia T et al. Activating internal tandem duplication mutations of the fms-like tyrosine kinase-3 (FLT3-ITD) at complete response and relapse in patients with acute myeloid leukemia. Haematologica 2012; 97: 1242–1245.
Kottaridis PD, Gale RE, Langabeer SE, Frew ME, Bowen DT, Linch DC . Studies of FLT3 mutations in paired presentation and relapse samples from patients with acute myeloid leukemia: implications for the role of FLT3 mutations in leukemogenesis, minimal residual disease detection, and possible therapy with FLT3 inhibitors. Blood 2002; 100: 2393–2398.
Murphy KM, Levis M, Hafez MJ, Geiger T, Cooper LC, Smith BD et al. Detection of FLT3 internal tandem duplication and D835 mutations by a multiplex polymerase chain reaction and capillary electrophoresis assay. J Mol Diagn 2003; 5: 96–102.
Acknowledgements
This study was supported by a grant of the Korean Health Technology R&D Project, Ministry for Health and Welfare, Korea (HI14C3417).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Blood Cancer Journal website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Kim, Y., Lee, G., Park, J. et al. Quantitative fragment analysis of FLT3-ITD efficiently identifying poor prognostic group with high mutant allele burden or long ITD length. Blood Cancer Journal 5, e336 (2015). https://doi.org/10.1038/bcj.2015.61
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bcj.2015.61
This article is cited by
-
ITDetect: a method to detect internal tandem duplication of FMS-like tyrosine kinase (FLT3) from next-generation sequencing data with high sensitivity and clinical application
BMC Bioinformatics (2023)
-
Ultrasensitive quantitation of FLT3-ITD mutation in patients with acute myeloid leukemia using ddPCR
Molecular Biology Reports (2023)
-
A comparative study of next-generation sequencing and fragment analysis for the detection and allelic ratio determination of FLT3 internal tandem duplication
Diagnostic Pathology (2022)
-
Frugal alignment-free identification of FLT3-internal tandem duplications with FiLT3r
BMC Bioinformatics (2022)
-
Association of hematologic response and assay sensitivity on the prognostic impact of measurable residual disease in acute myeloid leukemia: a systematic review and meta-analysis
Leukemia (2022)