Abstract
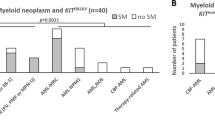
Although KITD816V occurs universally in adult systemic mastocytosis (SM), the clinical heterogeneity of SM suggests presence of additional phenotype-patterning mutations. Because up to 25% of SM patients have KITD816V-positive eosinophilia, we undertook whole-exome sequencing in a patient with aggressive SM with eosinophilia to identify novel genetic alterations. We conducted sequencing of purified eosinophils (clone/tumor sample), with T-lymphocytes as the matched control/non-tumor sample. In addition to KITD816V, we identified a somatic missense mutation in ethanolamine kinase 1 (ETNK1N244S) that was not present in 50 healthy controls. Targeted resequencing of 290 patients showed ETNK1 mutations to be distributed as follows: (i) SM (n=82; 6% mutated); (ii) chronic myelomonocytic leukemia (CMML; n=29; 14% mutated); (iii) idiopathic hypereosinophilia (n=137; <1% mutated); (iv) primary myelofibrosis (n=32; 0% mutated); and (v) others (n=10; 0% mutated). Of the 82 SM cases, 25 had significant eosinophilia; of these 20% carried ETNK1 mutations. The ten mutations (N244S=6, N244T=1, N244K=1, G245A=2) targeted two contiguous amino acids in the ETNK1 kinase domain, and are predicted to be functionally disruptive. In summary, we identified novel somatic missense ETNK1 mutations that were most frequent in SM with eosinophilia and CMML; this suggests a potential pathogenetic role for dysregulated cytidine diphosphate-ethanolamine pathway metabolites in these diseases.
Similar content being viewed by others
Introduction
Systemic mastocytosis (SM) is a chronic myeloproliferative neoplasm (MPN) characterized by an accumulation of morphologically and immunophenotypically abnormal mast cells (MC) in extra-cutaneous organs.1 Although >90% of adult SM patients can be demonstrated to harbor the KITD816V mutation,2 which constitutively activates KIT kinase activity and is thought to represent the driver mutation for this malignancy, the clinical presentation of SM is extremely heterogeneous. Patients with indolent SM have symptoms primarily related to MC degranulation with a normal life expectancy; in contrast, patients with other variants (aggressive SM (ASM), SM-AHD (SM associated with an associated hematological neoplasm) and MC leukemia) have an aggressive clinical course with features of organ dysfunction related to MC infiltration and shortened life expectancy.3 Possible explanations for the diverse clinical presentation include the lineage differential potential of the stem/progenitor cell targeted by the KITD816V mutation (reviewed by Pardanani4), and/or the co-occurrence (with KITD816V) of other pathogenetically relevant mutations that modify the disease phenotype in a given SM patient.5, 6
Approximately 15–20% of SM patients present with significant peripheral blood (PB) and bone marrow eosinophilia;3 we have previously demonstrated that the eosinophils in such cases are derived from the KITD816V-mutated neoplastic clone.7 In the current study, we pursued an exome-sequencing strategy using DNA isolated from (clonal/tumor) eosinophils that were purified to near-homogeneity from a patient with KITD816V-mutated ASM with associated eosinophilia, in order to identify genetic alterations of potential pathogenetic significance. T-lymphocytes enriched from PB served as the matched control/non-tumor sample in our experimental approach. On the basis of the initial findings from this index case, targeted resequencing of additional samples from patients with SM and other MPNs were undertaken to analyze the prevalence of disease-relevant mutations across a broader cross-section of myeloid malignancies.
Methods
The current study was approved by the Mayo Clinic institutional review board. All patients provided written informed consent for research sample collection. Diagnosis of SM and other MPNs was as per the 2008 World Health Organization (WHO) criteria.8 Granulocytes and PB mononuclear cells were enriched from whole blood using standard double-density Ficoll-gradient centrifugation. T-lymphocytes were enriched from the PB mononuclear cells fraction by positive selection of CD3 antibody-labeled cells by magnetic bead separation using standard protocols (StemCell Technologies, Vancouver, CA, USA). Similarly, a relatively pure population of eosinophils was isolated by negative selection of the CD16-labeled granulocyte fraction using the same methodology. We have previously validated the latter method as yielding eosinophils of ⩾97% purity.7
DNA was isolated from eosinophil and T-lymphocyte fractions using standard methods. Matched genomic libraries enriched for exonic regions (Agilent SureSelect XT kit; Agilent Technologies, Santa Clara, CA, USA) were prepared and sequenced on an Illumina HiSeq 2000 Analyzer using Illumina TruSeq chemistry (Illumina, San Diego, CA, USA). Data were analyzed using the GeneSifter Software (Perkin Elmer, Seattle, WA, USA). Post-processed alignments from the clonal fraction were compared with alignments from the control to make calls for somatic variants. Candidate mutations were validated by Sanger sequencing (see Supplementary Data for detailed experimental methods regarding library preparation, target capture, paired-end sequencing and data analysis).
Results
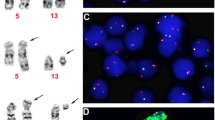
Our experimental strategy was validated by identification of heterozygous KITD816V in eosinophils (70 reads, 47.1% mutant), but not in T-lymphocytes (66 reads, 0.0% mutant) in the index patient. A detailed list of somatic coding region single-nucleotide variant calls is presented in Supplementary Table 1. Among the non-synonymous single-nucleotide variants of interest (novel variants, as well as known oncogenic mutations) ranked by percentage mutant burden in clonal eosinophils were: enhancer of zeste homolog 2 (EZH2), EZH2H694R (tumor: 38 reads, 97.4% mutant; control: 32 reads, 3.1% mutant), signal transducer and activator of transcription 5 α (STAT5α), STAT5αV707E (tumor: 30 reads, 67.0% mutant; control: 33 reads, 0.0% mutant) and ethanolamine kinase 1 (ETNK1), ETNK1N244S, (tumor: 38 reads, 50.0%; control: 72 reads, 1.4%; Figure 1).
Left panel: targeted resequencing confirming exome-sequencing results in index case with aggressive systemic mastocytosis (ASM) with associated eosinophilia. Sanger sequencing confirmed the presence of coding region non-synonymous sequence variants in KIT, EZH2, STAT5α and ETNK1 genes in the eosinophil fraction but not in the T-lymphocyte fraction. The percentage mutated alleles of total reads for each fraction and nucleotide/amino acid nomenclature for the observed genetic variation are shown. Right panel: Sanger sequencing traces of various somatic ETNK1 mutations (four mutation types, total ten mutations) identified in our cohort, showing nucleotide and amino acid change for every variant.
We conducted targeted re-sequencing of STAT5α and ETNK1 in healthy controls and additional patient samples to assess whether the aforementioned novel genomic variants in these genes represented recurrent molecular abnormalities and whether they were associated with a specific MPN. Neither of the aforementioned genetic variants was identified in granulocyte-derived DNA from 50 healthy controls. In the first stage, we re-sequenced 125 patients, including 50 patients with SM, and 25 each with primary myelofibrosis, chronic myelomonocytic leukemia (CMML) and primary/idiopathic hypereosinophilia. No additional patients harboring the aforementioned STAT5α variant were identified. We did however identify ETNK1 mutations in exon 3 in nine additional patients (i.e., ten patients in total); of these, six patients (including the index case) exhibited significant eosinophilia (four with SM-AHD (the latter was ‘MPN-NOS’ (MPN-not otherwise specified) and ‘MDS/MPN-NOS’ (myelodysplastic syndrome/MPN-NOS) in two cases each) and one each with ASM and idiopathic hypereosinophilia; Table 1; Figure 1). The remaining four patients with ETNK1 mutations were diagnosed with CMML and notably, none of these cases had associated eosinophilia. Consequently, ETNK1 mutation prevalence in the initial screen was 10/125 (8%). We also screened the subgroup with wild-type ETNK1 (n=115), for mutations in exon 3 of its paralogous gene, ETNK2, however no additional mutations were identified in the latter gene. In the second stage, we conducted targeted re-sequencing of 165 additional MPN patients for ETNK1 mutations. Of the total 290 patients screened, the disease distribution (percentage ETNK1 mutated) was as follows: (i) SM (n=82; 6% mutated), (ii) CMML (n=29; 14% mutated), (iii) idiopathic hypereosinophilia (n=137; <1% mutated), (iv) primary myelofibrosis (n=32; 0% mutated) and (v) Others (n=10; 0% mutated). Of the 82 total SM patients studied, 36 had indolent SM, 26 had SM-AHD and 20 had ASM. Of the 82 SM cases, 25 had significant associated eosinophilia; of these 5/25 patients (20%) carried ETNK1 mutations.
We identified 4 novel ETNK1 mutations involving a total 10 patients (N244S=6, N244T=1, N244K=1 and G245A=2; Figure 1). In every case, the mutation was heterozygous and targeted one of two contiguous amino acid residues (N244 or G245) within the predicted kinase domain. ETNK1 is 452 amino acids long, of which residues 100–444 comprise the protein kinase-like domain containing the putative nucleotide-binding site and the catalytic-site in an inter-lobe cleft. There is a high degree of sequence conservation between species in this region (Supplementary Figure 1), indicating a high degree of functional conservation. Computational tools for predicting the functional consequence of sequence changes targeting N244 and G245 suggested that the aforementioned ETNK1 mutations were functionally deleterious (http://snps.biofold.org/phd-snp/phd-snp.html and http://genetics.bwh.harvard.edu/pph2/index.shtml). Four of five patients with SM harbored a concurrent KITD816V mutation; interestingly, one patient was found to have wild-type KIT sequence at this locus despite use of an allele-specific PCR for mutation detection (sensitivity ⩽0.01%; Table 1).3 Although not formally analyzed, aside from presence of significant concurrent eosinophilia in non-CMML patients in our study, there were no other clinical, molecular/cytogenetic, or bone marrow histologic characteristics that were unique to ETNK1-mutated patients as compared with disease-specific non-mutated patients (Table 1). Limited functional studies were conducted wherein human ETNK1 protein (wild-type and N244S mutant) was overexpressed in murine Ba/F3 cells by means of a murine stem cell virus retroviral expression vector. In these studies, no discernable effect on cell proliferation, survival or apoptosis, regardless of ambient interleukin-3 concentrations was noted, as compared with empty vector control (data not shown).
Discussion
We originally reported our discovery of recurrent ETNK1 mutations in MPN patients in June 2014.9 In the current study, we found ETNK1 mutations to be largely restricted to patients with SM with associated eosinophilia (20%) and CMML (14%). Although the association of ETNK1 mutations with eosinophilia was intriguing, it appeared to be restricted to those patients with clonal myeloproliferative eosinophilia. In contrast, in our screening of a large cohort of patients with idiopathic eosinophilia as per WHO criteria (i.e., those lacking histologic, cytogenetic or molecular characteristics of clonal hematopoiesis), only one of 137 patients was found to harbor an ETNK1 mutation. The association of ETNK1 mutations with CMML was somewhat less intriguing given our current knowledge which suggests a high degree of genetic instability inherent to CMML, underscored by the high frequency of somatic mutations in diverse genes and oncogenic pathways identified in genetic screening studies.10 Nevertheless, as with most other recently identified pathogenetically relevant mutations in BCR-ABL1-negative MPNs, ETNK1 mutations were not uniformly associated with a specific MPN in the current study.
ETNK1 is an ethanolamine-specific kinase that catalyzes the phosphorylation of ethanolamine by ATP to yield phosphoethanolamine, which is the first and possibly rate-limiting step committing ethanolamine to the CDP-ethanolamine pathway for biosynthesis of phosphatidylethanolamine (PE) in mammalian tissues.11 PE and phosphatidylcholine (PC) are zwitterionic glycerophospholipids and represent the most abundant phospholipids in eukaryotic cells that are synthesized by two related branches of the Kennedy pathway referred to as the CDP-ethanolamine and CDP-choline pathways, respectively.12 PE has diverse roles including a major role in maintaining cell-membrane architecture and the topology of transmembrane proteins (summarized by Gibellini and Smith13). Further, PE has a major role during cell division in ensuring the proper progression of cytokinesis, and is the precursor for important biologically active molecules such as diacylglycerols, fatty acids and phosphatidic acid. PE also provides for phosphoethanolamine capping of glycophosphatidylinositol that anchors many proteins to the cell surface. Finally, PE phospholipids can exist as plasmalogens that have a key role in membrane dynamics, scavenging of membrane localized free radical species and as a precursor for prostanoid synthesis and intracellular signaling. Disruption of the Drosophila ethanolamine kinase gene, eas, revealed a phenotype of seizure, neuronal failure and paralysis consistent with altered membrane phospholipid composition.14 In murine models, disruption of the ethanolamine kinase-2 and phosphoethanolamine cytidyltransferase genes were associated with neonatal lethality (summarized by Vance and Vance).15 Abnormalities in choline metabolism have emerged as a metabolic hallmark of cancer; overexpression of several enzymes in the PC biosynthetic pathway have been identified and may have a role as prognostic markers in various cancers (summarized by Glunde et al.).16 Further, recent studies have indicated a reciprocal interaction between hyperactive choline metabolism, leading to increased levels of phosphocholine/total choline, and enhanced oncogenic signaling via RAS, PI3K-AKT, and HIF-1α pathways. There is an ongoing phase 1 study of a choline kinase-α inhibitor for the treatment of patients with advanced solid tumors (Clinicaltrials.gov, study# NCT01215864). The aforementioned data make it highly plausible that abnormalities in PE metabolism induced by mutations in relevant enzymes in its biosynthetic pathway such as ETNK1 have a similar role in oncogenesis as seen with altered PC metabolism.
Although the current study provides novel insights into the potential role of altered glycerophospholipid metabolism in MPN pathogenesis, significant additional work remains to be done. First, the mechanism by which altered levels of CDP-ethanolamine pathway intermediates lead to a growth or survival advantage for the affected clone remains to be determined. Further, it is unclear based upon current data as to whether the aforementioned ETNK1 mutations constitute the driver mutation for the underlying MPN or MDS/MPN. On the basis of the known co-occurrence of other pathogenic mutations in SM (i.e., KITD816V) and CMML (e.g., ASXL1, DNMT3A, CBL), a reasonable assumption is that ETNK1 mutations provide a phenotype-patterning effect (e.g., eosinophilia) and/or incremental growth/survival advantage such as the co-operation seen between TET2 and KITD816V or JAK2V617F mutations.17, 18, 19
References
Horny HP, Metcalfe DD, Bennett JM, Bain BJ, Akin C, Escribano L et al. Mastocytosis. In: Swerdlow SH, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H (eds). WHO Classification of Tumors of Hematopoietic and Lymphoid Tissues 4th edn. International Agency for Research and Cancer (IARC): Lyon, 2008, pp 54–63.
Garcia-Montero AC, Jara-Acevedo M, Teodosio C, Sanchez ML, Nunez R, Prados A et al. KIT mutation in mast cells and other bone marrow hematopoietic cell lineages in systemic mast cell disorders: a prospective study of the Spanish Network on Mastocytosis (REMA) in a series of 113 patients. Blood 2006; 108: 2366–2372.
Lim KH, Tefferi A, Lasho TL, Finke C, Patnaik M, Butterfield JH et al. Systemic mastocytosis in 342 consecutive adults: survival studies and prognostic factors. Blood 2009; 113: 5727–5736.
Pardanani A . Systemic mastocytosis in adults: 2013 update on diagnosis, risk stratification, and management. Am J Hematol 2013; 88: 612–624.
Schwaab J, Schnittger S, Sotlar K, Walz C, Fabarius A, Pfirrmann M et al. Comprehensive mutational profiling in advanced systemic mastocytosis. Blood 2013; 122: 2460–2466.
Tefferi A, Levine RL, Lim KH, Abdel-Wahab O, Lasho TL, Patel J et al. Frequent TET2 mutations in systemic mastocytosis: clinical, KITD816V and FIP1L1-PDGFRA correlates. Leukemia 2009; 23: 900–904.
Pardanani A, Reeder T, Li CY, Tefferi A . Eosinophils are derived from the neoplastic clone in patients with systemic mastocytosis and eosinophilia. Leuk Res 2003; 27: 883–885.
Vardiman JW, Thiele J, Arber DA, Brunning RD, Borowitz MJ, Porwit A et al. The 2008 revision of the World Health Organization (WHO) classification of myeloid neoplasms and acute leukemia: rationale and important changes. Blood 2009; 114: 937–951.
Lasho T, Finke C, Zblewski D, Abdelrahman R, Patnaik M, Knudson R et al. Recurrent Etnk1 kinase domain mutations in systemic mastocytosis with associated eosinophilia. Haematologica 2014; 99: 251–251.
Jankowska AM, Makishima H, Tiu RV, Szpurka H, Huang Y, Traina F et al. Mutational spectrum analysis of chronic myelomonocytic leukemia includes genes associated with epigenetic regulation: UTX, EZH2, and DNMT3A. Blood 2011; 118: 3932–3941.
Lykidis A, Wang J, Karim MA, Jackowski S . Overexpression of a mammalian ethanolamine-specific kinase accelerates the CDP-ethanolamine pathway. J Biol Chem 2001; 276: 2174–2179.
Kennedy EP, Weiss SB . The function of cytidine coenzymes in the biosynthesis of phospholipides. J Biol Chem 1956; 222: 193–214.
Gibellini F, Smith TK . The Kennedy pathway–de novo synthesis of phosphatidylethanolamine and phosphatidylcholine. IUBMB Life 2010; 62: 414–428.
Pavlidis P, Ramaswami M, Tanouye MA . The Drosophila easily shocked gene: a mutation in a phospholipid synthetic pathway causes seizure, neuronal failure, and paralysis. Cell 1994; 79: 23–33.
Vance DE, Vance JE . Physiological consequences of disruption of mammalian phospholipid biosynthetic genes. J Lipid Res 2009; 50 (Suppl): S132–S137.
Glunde K, Bhujwalla ZM, Ronen SM . Choline metabolism in malignant transformation. Nat Rev Cancer 2011; 11: 835–848.
De Vita S, Schneider RK, Garcia M, Wood J, Gavillet M, Ebert BL et al. Loss of function of TET2 cooperates with constitutively active KIT in murine and human models of mastocytosis. PloS One 2014; 9: e96209.
Soucie E, Hanssens K, Mercher T, Georgin-Lavialle S, Damaj G, Livideanu C et al. In aggressive forms of mastocytosis, TET2 loss cooperates with c-KITD816V to transform mast cells. Blood 2012; 120: 4846–4849.
Kameda T, Shide K, Yamaji T, Kamiunten A, Sekine M, Taniguchi Y et al. Loss-of-TET2 has dual roles in murine myeloproliferative neoplasms: disease sustainer and disease accelerator. Blood 2014, e-pub ahead of print 13 November 2014.
Acknowledgements
We thank the Mayo Clinic core genomic sequencing facility for exome sequencing.
Author Contributions
AP, TLL and AT designed the study and analyzed the data. TLL conducted primary analysis of the exome-sequencing data, cloning of ETNK1 and functional experiments. TLL and CMF performed Sanger sequencing for mutation validation. DZ and MP provided patients for the study. RPK analyzed molecular/cytogenetic data. DC and CAH reviewed bone marrow histology. TLL and AP wrote the first draft of the manuscript. All authors reviewed the draft, provided input for revisions and approved the final version of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies this paper on Blood Cancer Journal website
Supplementary information
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-NoDerivs 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-nd/4.0/
About this article
Cite this article
Lasho, T., Finke, C., Zblewski, D. et al. Novel recurrent mutations in ethanolamine kinase 1 (ETNK1) gene in systemic mastocytosis with eosinophilia and chronic myelomonocytic leukemia. Blood Cancer Journal 5, e275 (2015). https://doi.org/10.1038/bcj.2014.94
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bcj.2014.94
This article is cited by
-
Mutations in chronic myelomonocytic leukemia and their prognostic relevance
Clinical and Translational Oncology (2021)
-
ETNK1 mutations induce a mutator phenotype that can be reverted with phosphoethanolamine
Nature Communications (2020)
-
Diagnostik und Management des myelodysplastischen Syndroms
Der Onkologe (2019)
-
Diagnostik und Management der myelodysplastischen Syndrome*
InFo Hämatologie + Onkologie (2019)
-
Targeting few to help hundreds: JAK, MAPK and ROCK pathways as druggable targets in atypical chronic myeloid leukemia
Molecular Cancer (2018)