Abstract
To clarify the effect of killer cell immunoglobulin-like receptor (KIR) ligand incompatibility on outcomes of acute myeloid leukemia (AML) and acute lymphoblastic leukemia (ALL) patients in complete remission after single cord blood transplantation (CBT), we assessed the outcomes of CBT registered in the Japan Society for Hematopoietic Cell Transplantation (JSHCT) database. A total of 643 acute leukemia (357 AML and 286 ALL) patient and donor pairs were categorized according to their KIR ligand incompatibility by determining whether or not they expressed HLA-C, Bw4 or A3/A11 by DNA typing. A total of 128 patient–donor pairs were KIR ligand-incompatible in the graft-versus-host (GVH) direction and 139 patient–donor pairs were incompatible in the host-versus-graft (HVG) direction. Univariate and multivariate analyses showed no significant differences between the KIR ligand-incompatible and compatible groups in the GVH direction for both AML and ALL patients of overall survival, disease-free survival, relapse incidence, non-relapse mortality and acute GVH disease. However, KIR incompatibility in the HVG direction ameliorated engraftment in ALL patients (hazard ratio 0.66, 95% confidence interval 0.47–0.91, P=0.013). Therefore, there were no effects of KIR ligand incompatibility in the GVH direction on single CBT outcomes for acute leukemia patients without anti-thymocyte globulin use. However, it is necessary to pay attention to KIR incompatibility in the HVG direction for engraftment.
Similar content being viewed by others
Introduction
Killer cell immunoglobulin-like receptor (KIR) ligand incompatibility may have some important roles in transplantation outcomes such as leukemia relapse and leukemia-free survival.1, 2, 3, 4 Ruggeri et al.5, 6 reported surprisingly good clinical results that indicated no relapse, no rejection and no acute graft-versus-host disease (GVHD) after human leukocyte antigen (HLA) haplotype-mismatched transplantations with KIR ligand incompatibility in the GVH direction for acute myeloid leukemia (AML) patients. They also reported that donor allogeneic natural killer (NK) cells attacked host antigen-presenting cells (APCs), resulting in the suppression of GVHD. However, results of studies regarding the clinical advantage of KIR ligand incompatibility in allogeneic stem cell transplantation (allo SCT) from an unrelated donor are discrepant. Davies et al.7 reported that there was no effect of KIR ligand incompatibility on outcomes of unrelated bone marrow transplantation without using anti-thymocyte globulin (ATG), whereas Giebel et al.8 reported a good effect of KIR ligand incompatibility on the outcomes of unrelated bone marrow transplantation using ATG as part of GVHD prophylaxis. Morishima et al.9 reported that KIR ligand mismatching induced adverse effects on acute GVHD and rejection in leukemia patients undergoing transplantation with T-cell-replete marrow from an unrelated donor in Japan. It was reported that cord blood transplantation (CBT) for acute leukemia patients in complete remission (CR) from KIR ligand-incompatible donors in the GVH direction was associated with decreased relapse and improved survival.10 In another study, it was shown that KIR ligand mismatch was associated with development of severe acute GVHD and risk of death after double CBT with reduced-intensity conditioning (RIC) regimen.11 Therefore, the role of KIR ligand incompatibility in allo SCT remains controversial. To clarify the effect of KIR ligand incompatibility on the outcomes of AML and acute lymphoblastic leukemia (ALL) patients in CR after single CBT, we assessed the outcomes of CBT registered in the Japan Society for Hematopoietic Cell Transplantation (JSHCT) database between 2001 and 2010 (A Study from the HLA Working Group of the JSHCT).
Materials and methods
Study design and data collection
This study was a retrospective analysis of data from a Japanese nationwide multicenter survey. Data were provided by the HLA Working Group of the JSHCT. Outcomes of 643 acute leukemia (357 AML nd 286 ALL) patients in CR were analyzed. Informed consent was obtained from patients and donors according to the Declaration of Helsinki, and approval was obtained from the Institutional Review Board of Hokkaido University Hospital.
Patient population
This study included AML and ALL patients who received single CBT in CR and (1) patients and donors whose HLA-A, B, C and DR alleles were determined by DNA typing as described previously,9 (2) underwent transplantation between 2001 and 2010, (3) received a myeloablative conditioning (MAC) regimen (n=456) as high-dose radiation and chemotherapy usually in combination with cyclophosphamide or an RIC regimen (n=187) defined basically as the use of fludarabine plus low-dose busulfan or melphalan with or without low-dose total body irradiation12 and (4) did not receive ATG as a preparative regimen.
Inhibitory KIR ligand assessment
Patients and donors were categorized according to their KIR ligand incompatibility by determining whether or not they expressed HLA-C group 1 or 2, Bw4 or A3/A11 as initially described by Ruggeri et al.5 and Leung.13 KIR ligand mismatch in the GVH direction was scored when the donor’s KIR ligand was not shared by the patient. KIR ligand mismatch in the HVG direction was scored when the patient’s KIR ligand was not shared by the donor.
Transplant procedures
Differences among patients, disease and transplantation-related factors according to conditioning regimens, and GVHD prophylaxis are shown in Tables 1a and b.
Endpoints
Primary endpoints included overall survival (OS), disease-free survival (DFS), relapse (cumulative incidence of relapse, CIR), non-relapse mortality (NRM) and engraftment. Relapse was defined as clinical and hematological leukemia recurrence. NRM was defined as death during continuous CR after transplantation. Engraftment was defined as a peripheral granulocyte count of >500/μl for three consecutive days after transplantation.
Statistical analysis
Characteristics of patients who received KIR ligand-incompatible CBT in the GVH direction and the compatible group were compared using the χ2-test for categorical variables and the Wilcoxon two-sample test for continuous variables. To compare the prognosis of the incompatible group with that of the compatible group, univariate survival analyses were conducted for OS, DFS, CIR, NRM, engraftment and acute GVHD (grades II–IV). Survival curves of OS and DFS for each group were depicted using the Kaplan–Meier method and compared using the log-rank test. In the analysis of CIR, NRM, engraftment and acute GVHD, cumulative probabilities were estimated on the basis of cumulative incidence curves to accommodate the following competing events: death for relapse, relapse for transplantation-related mortality, death without GVHD for acute GVHD and death without engraftment for neutrophil engraftment. Groups were compared using the Gray test.14 To adjust for potential confounders, multivariate analyses were conducted using the Cox proportional hazards model for OS and DFS, and using the Fine–Gray proportional hazards model for CIR and NRM.15 The variables considered in the multivariate analysis were age at transplantation (40 years or more, 16–39 years and <15 years), performance status before transplantation (2–4 and 0–1), year of transplantation (2006–2009 and 2001–2005), sex (female and male), disease status (CR2 and CR1), conditioning regimens (RIC and MAC), HLA matching and infused cells (>2.5 × 107/kg and <2.5 × 107/kg) as a clinically important prognostic factor. All statistical analyses were conducted using SAS ver 9.2 (SAS Institute Inc., Cary, NC, USA) and R (www.r-project.org, last accessed 5 April 2012).
Results
Patients and clinical characteristics
Tables 1a and 1b show clinical and biological characteristics of the 286 ALL and 357 AML patients who received single CBT. One hundred and twenty-eight patient–donor pairs (ALL n=59, AML n=69) were KIR ligand-incompatible in the GVH direction and 139 patient–donor pairs (ALL n=65, AML n=74) were incompatible in the HVG direction. Regarding KIR ligand incompatibility in the GVH direction, 59 ALL patients were transplanted with HLA-A, B or C KIR ligand-incompatible cord blood (A3/A11 n=9, Bw4 n=16, C n=24, A+C n=3, B+C n=7) and 69 AML patients were transplanted with HLA-A, B or C KIR ligand-incompatible cord blood (A3/A11 n=11, Bw4 n=31, C n=24, A+C n=2, B+C n=1). Regarding KIR ligand incompatibility in the HVG direction, 65 ALL patients were transplanted with HLA-A, B or C KIR ligand-incompatible cord blood (A3/A11 n=17, Bw4 n=13, C n=35, A+B n=1, A+C n=5) and 74 AML patients were transplanted with HLA-A, B or C KIR ligand-incompatible cord blood (A3/A11 n=14, Bw4 n=14, C n=42, A+C n=4). The number of patients mismatched in both the GVH and HVG directions is quite few (15 ALL patients and 18 AML patients). RIC regimens were used in 187 patients (ALL n=58 and AML n=129). There were no significant differences in other prognostic factors without HLA matching.
Impact of KIR ligand mismatch in the GVH direction on transplantation outcomes
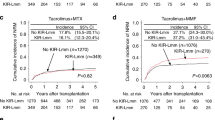
Univariate analysis showed no significant differences between KIR ligand-incompatible and compatible groups in the GVH direction for both AML and ALL patients in OS, DFS, relapse incidence, NRM, acute GVHD and engraftment (P=0.628, P=0.352, P=0.693, P=0.492, P=0.691, P=0.832 for ALL patients and P=0.674, P=0.688, P=0.353, P=0.766, P=0.569, P=0474 for AML patients, respectively; Figures1a and b).
Causes of death are shown in Table 2a. Rates of mortality due to original disease and infections were almost the same in the KIR ligand-compatible and incompatible donor groups.
There were no significant differences in OS, DFS, relapse incidence, NRM, engraftment and acute GVHD between the KIR ligand-incompatible and compatible groups in the GVH direction for both AML and ALL patients by multivariate analysis (hazard ratio (HR) 0.87, P=0.557; HR 0.79, P=0.352; HR 0.95, P=0.91; HR 0.71, P=0.32; HR 1.08, P=0.63; HR 1.06, P=0.83 for ALL patients and HR 0.93, P=0.752; HR 1.02, P=0.945; HR 0.59, P=0.12; HR 0.95, P=0.86; HR 0.97, P=0.89; HR 0.84, P=0.51 for AML patients, respectively; Tables 3a and b). The conditioning regimens (RIC and MAC) did not affect these results.
For ALL patients, age >40 years and CR2 were associated with poor OS (HR 4.25, P<0.001 and HR 2.09, P<0.001, respectively) and also with poor DFS (HR 2.41, P=0.002 and HR 1.67, P=0.011, respectively). Also, age >40 years was associated with higher NRM and lower engraftment rate (HR 6.96, P<0.001 and HR 0.55, P<0.001, respectively). For AML patients, age >40 years and male gender were associated with poor OS (HR 1.93, P=0.057 and HR 1.78, P=0.003, respectively) and also with higher NRM (HR 2.59, P=0.052 and HR 1.71, P=0.031, respectively). Also, male gender was associated with poor DFS (HR 1.48, P=0.033). Infused cell number of >2.5 × 107/kg was associated with higher engraftment rate and MAC regimen was associated with lower engraftment rate (HR 1.369, P=0.018 and HR 0.686, P=0.007, respectively). Age >40 years was associated with lower incidence of GVHD (HR 0.50, P=0.031) and HLA mismatch was associated with higher incidence of GVHD (HR 1.58, P=0.058).
Impact of KIR ligand mismatch in the HVG direction on transplantation outcomes
Univariate analysis showed no significant differences between the KIR ligand-incompatible and compatible groups in the HVG direction for both AML and ALL patients in OS, DFS, relapse incidence, NRM and acute GVHD (P=0.954, P=0.531, P=0.149, P=0.465, P=0.901 for ALL patients and P=0.264, P=0.383, P=0.654, P=0.598, P=0.628 for AML patients, respectively; Figures1c and d). However, there was a significant difference in engraftment between the KIR ligand-incompatible and compatible groups in the HVG direction for ALL patients (P=0.022 for ALL patients and P=0.151 for AML patients).
Causes of death are shown in Table 2b. Rates of mortality owing to original disease were almost the same in the KIR ligand-compatible and incompatible donor groups. Rate of mortality owing to infection was higher in the KIR ligand-incompatible donor group with ALL.
Also, there were no significant differences in OS, DFS, relapse incidence, NRM and acute GVHD between the KIR ligand-incompatible and compatible groups in the HVG direction for both AML and ALL patients by multivariate analysis (HR 0.84, P=0.457; HR 0.76, P=0.225; HR 1.12, P=0.76; HR 1.06, P=0.85; HR 1.08, P=0.75 for ALL patients and HR 0.73, P=0.197; HR 0.83, P=0.414; HR 0.86, P=0.68; HR 0.88, P=0.66; HR 1.20, P=0.42 for AML patients, respectively; Tables 3c and d). However, there was a significant difference in engraftment between the KIR ligand-incompatible and compatible groups in the HVG direction for ALL patients (HR 0.66, P=0.013). The conditioning regimens (RIC and MAC) did not affect these results.
For ALL patients, age >40 years and CR2 were associated with poor OS (HR 4.33, P<0.001 and HR 2.11, P<0.001, respectively) and also with poor DFS (HR 2.49, P=0.001 and HR 1.70, P=0.009, respectively). Also, age >40 years was associated with higher NRM and lower engraftment rate (HR 6.87, P<0.001 and HR 0.56, P<0.001, respectively). For AML patients, age >40 years and male gender were associated with poor OS (HR 2.00, P=0.045 and HR 1.76, P=0.003, respectively) and also with higher NRM (HR 2.62, P=0.051 and HR 1.69, P=0.032, respectively). Also, male gender was associated with poor DFS (HR 1.48, P=0.032). Infused cell number of >2.5 × 107/kg was associated with higher engraftment rate and MAC regimen was associated with lower engraftment rate (HR 1.387, P=0.014 and HR 0.694, P=0.009, respectively). Age >40 years was associated with lower incidence of GVHD (HR 0.51, P=0.035) and HLA mismatch was associated with higher incidence of GVHD (HR 1.49, P=0.086).
Discussion
The role of KIR ligand incompatibility in allo SCT is controversial with various diseases and conditionings.16, 17 It has been suggested that NK cell alloreactivity is associated with better outcome after allo SCT when a high stem cell dose, extensive T-cell depletion and ATG are used.18, 19 NK cell engraftment is earlier and more robust and T-cell engraftment is delayed after CBT.20, 21 Therefore, CBT may represent a setting in which KIR ligand incompatibility is associated with protection from leukemia relapse. Willemze et al.22 reported transplantation outcomes after single-unit CBT for AML patients (n=94) and ALL patients (n=124). Among those patients, KIR ligand incompatibility was associated with reduced relapse of AML and increased OS. In their study, >80% of the patients were administered ATG or antilymphocyte globulin under MAC. Brunstein et al.23 reported results for 257 patients with single-unit CBT (n=91) and double-unit CBT (n=166) after myeloablative (n=155) and reduced intensity (n=102) conditioning. KIR ligand incompatibility was associated with higher rate of acute GVHD and decreased OS under RIC. In their study, only 30% of the patients were administered ATG. Garfall et al.24 reported outcomes of double-unit CBT for 80 patients with various hematological malignancies including 31 AML patients. Among those patients, KIR ligand incompatibility was not associated with relapse reduction. In their study, >70% of the patients were administered ATG with RIC (Flu/Mel/ATG). Those studies that included different transplantation protocols with different disease distributions after single-unit and double-unit CBT showed conflicting results.25, 26
Lowe et al.27 investigated the relative significance of NK cell and T-cell alloreactivity in 105 pediatric patients who received minimally T-cell-depleted HLA-non-identical bone marrow transplantation. They showed that donor NK cell incompatibility did not improve patient outcome. In contrast, donor T-cell incompatibility was a risk factor for acute GVHD, chronic GVHD and death. Thus, T-cell alloreactivity dominated that of NK cells in minimally T-cell-depleted grafts. It was reported that KIR ligand mismatching induced adverse effects on acute GVHD and rejection and brought no survival benefits to leukemia patients undergoing transplantation with T-cell-replete marrow from an unrelated donor in Japan.9 Also, Yabe et al.28 reported that KIR ligand incompatibility had potent adverse effects with a higher incidence of acute GVHD and lower OS without ATG, whereas ATG administration ameliorated most of the adverse effects. Therefore, administration of ATG extensively depletes patient’s and donor’s T cells and becomes a critical factor in attenuating the adverse effects of KIR ligand-incompatible transplantation predominating alloreactive NK cells to induce an antileukemic effect. NK cell cytotoxicity toward a particular target cell is regulated by a balance of activating and inhibitory cell–cell contacts. The absence of HLA class I on a target cell allows other activating signals to dominate.29, 30 Inhibitory NK receptors protect self-HLA-expressing normal tissue from NK cells. The second property of an inhibitory NK receptor is to educate or license NK cells to acquire function. NK cells acquire function following engagement of inhibitory receptors with self-ligands after their differentiation from hematopoietic progenitors. Therefore, allo SCT provides a unique environment for NK cell education and NK cell development from hematopoietic stem cells in a short period.31
We analyzed the effects of KIR ligand incompatibility in both GVH and HVG directions on single CBT outcomes in 643 acute leukemia patients in CR (ALL n=286 and AML n=357) without ATG in Japan. In contrast to the results of previous studies indicating that KIR ligand mismatching induced adverse effects on GVHD and survival in leukemia patients undergoing transplantation with T-cell-replete marrow from an unrelated donor in Japan,27, 28 our study did not show any positive or negative effects of KIR ligand incompatibility in either the GHV or HVG direction on OS, DFS, CIR, NRM and acute GVHD after single CBT without ATG. CBT may be tolerable to KIR ligand incompatibility in terms of transplantation outcomes such as GVHD, OS and DFS. Therefore, the source of stem cell may also be important to determine the clinical advantage of NK cell alloreactivity after unrelated SCT. We also analyzed transplantation outcomes for only patients with engraftment; however, there were no differences in OS and DFS between patients who received KIR ligand-compatible and incompatible transplantations (data not shown). There was also no difference in outcomes of KIR ligand-compatible and incompatible transplantations in acute leukemia patients combined with ALL and AML in CR. However, multivariate analysis showed a significantly lower rate of engraftment in ALL patients who were KIR ligand incompatible in the HVG direction than compatible patients (HR 0.66, 95% confidence interval 0.47–0.91, P=0.013). Also, AML patients who were KIR ligand incompatible in the HVG direction tended to have a lower rate of engraftment (HR 0.799, 95% confidence interval 0.59–1.084, P=0.15). It has been reported that NK epitope mismatching in the rejection direction was associated with an increased probability of rejection after unrelated bone marrow transplantation.9, 32 Signaling lymphocytic activation molecule (SLAM)-associated protein-related adaptors and SLAM family receptors were reported to act together in a mechanism that was essential for the elimination of hematopoietic cells but not non-hematopoietic cells by NK cells.33 Therefore, alloreactive NK cells induced by KIR ligand incompatibility in the HVG direction may attack donor hematopoietic cells to ameliorate donor cell engraftment after CBT with blood containing a relatively small number of hematopoietic stem cells. Administration of ATG as a preparative regimen may be important to obtain some positive effects of KIR ligand incompatibility in the GVH direction on CBT outcomes such as survival and relapse. The present study suggests that it is not necessary to consider KIR ligand compatibility in the GVH direction at CBT without ATG for transplantation outcomes. Also, there is the possibility that KIR ligand incompatibility in the GVH direction induces a graft-versus-leukemia effect for acute leukemia if patients receive ATG as a preparative regimen. On the other hand, it may be necessary to pay attention to KIR ligand compatibility in the HVG direction for engraftment after CBT.
We did not perform KIR genotyping in our cohort study; however, recent data have suggested an important role of KIR polymorphisms and KIR genotype in transplantation outcomes of allo SCT.34, 35 NK cell alloreactivity is regulated by a balance of activating and inhibitory cell–cell contacts. Although phenotypes of the KIR repertoire are personalized by various conditions,36 however, not only simple algorithm on ligands for inhibitory KIR but also KIR genotypes may be useful for predicting clinically relevant NK cell alloreactivity in a future study.
References
Ruggeri L, Capanni M, Mancusi A, Urbani E, Perruccio K, Burchielli E et al. Alloreactive natural killer cells in mismatched hematopoietic stem cell transplantation. Blood Cells Mol Dis 2004; 33: 216–221.
Moretta L, Locatelli F, Pende D, Marcenaro E, Mingari MC, Moretta A . Killer Ig-like receptor-mediated control of natural killer cell alloreactivity in haploidentical hematopoietic stem cell transplantation. Blood 2011; 117: 764–771.
Velardi A, Ruggeri L, Mancusi A . Killer-cell immunoglobulin-like receptors reactivity and outcome of stem cell transplant. Curr Opin Hematol 2012; 19: 319–323.
Tsirigotis PD, Resnick IB, Shapira M . The role of natural killer cells in hematopoietic stem cell transplantation. Ann Med 2012; 44: 130–145.
Ruggeri L, Capanni M, Urbani E, Perruccio K, Shlomchik WD, Tosti A et al. Effectiveness of donor natural killer cell alloreactivity in mismatched hematopoietic transplants. Science 2002; 295: 2097–2100.
Ruggeri L, Mancusi A, Capanni M, Urbani E, Carotti A, Aloisi T et al. Donor natural killer cell allorecognition of missing self in haploidentical hematopoietic transplantation for acute myeloid leukemia: challenging its predictive value. Blood 2007; 110: 433–440.
Davies SM, Ruggieri L, DeFor T, Wagner JE, Weisdorf DJ, Miller JS et al. Evaluation of KIR ligand incompatibility in mismatched unrelated donor hematopoietic transplants. Killer immunoglobulin-like receptor. Blood 2002; 100: 3825–3827.
Giebel S, Locatelli F, Lamparelli T, Velardi A, Davies S, Frumento G et al. Survival advantage with KIR ligand incompatibility in hematopoietic stem cell transplantation from unrelated donors. Blood 2003; 102: 814–819.
Morishima Y, Yabe T, Matsuo K, Kashiwase K, Inoko H, Saji H et al. Effects of HLA allele and killer immunoglobulinlike receptor ligand matching on clinical outcome in leukemia patients undergoing transplantation with T-cell–replete marrow from an unrelated donor. Biol Blood Marrow Transplant 2007; 13: 315–328.
Farag SS, Bacigalupo A, Eapen M, Hurley C, Dupont B, Caligiuri MA et al. The effect of KIR ligand incompatibility on the outcome of unrelated donor transplantation: a report from the center for international blood and marrow transplant research, the european blood and marrow transplant registry, and the Dutch registry. Biol Blood Marrow Transplant 2006; 12: 876–884.
Hsu K, Gooley T, Malkki M, Pinto-Agnello C, Dupont B, Bignon J-D et al. KIR ligands and prediction of relapse after unrelated donor hematopoietic cell transplantation for hematologic malignancy. Biol Blood Marrow Transplant 2006; 12: 828–836.
Giralt S, Ballen K, Rizzo D, Bacigalupo A, Horowitz M, Pasquini M et al. Reduced-intensity conditioning regimen workshop: defining the dose spectrum. Report of a workshop convened by the center for international blood and marrow transplant research. Biol Blood Marrow Transplant 2009; 15: 367–369.
Leung W . Use of NK cell activity in cure by transplant. Br J Haematol 2011; 155: 14–29.
Pepe MS, Mori M . Kaplan-Meier, marginal or conditional probability curves in summarizing competing risks failure time data? Stat Med 1993; 12: 737–751.
Fine JP, Gray RJ . A proportional hazards model for the subdistribution of a competing risk. J Am Stat Assoc 1999; 94: 496–509.
Farag SS, Fehniger TA, Ruggeri L, Velardi A, Caligiuri MA . Natural killer cell receptors: new biology and insights into the graft-versus-leukemia effect. Blood 2002; 100: 1935–1947.
Parham P . MHC class I molecules and KIRs in human history, health and survival. Nat Rev Immunol 2005; 5: 201–214.
Miller JS, Cooley S, Parham P, Farag SS, Verneris M, McQueen K et al. Missing KIR ligands are associated with less relapse and increased graft-versus-host disease (GVHD) following unrelated donor allogeneic HCT. Blood 2007; 109: 5058–5861.
Hsu KC, Keever-Taylor CA, Wilton A, Pinto C, Heller G, Arkun K et al. Improved outcome in HLA-identical sibling hematopoietic stem-cell transplantation for acute myelogenous leukemia predicted by KIR and HLA genotypes. Blood 2005; 105: 4878–4884.
Tanaka J, Sugita J, Asanuma S, Arita K, Shono Y, Kikutchi M et al. Increased number of CD16+CD56dim NK cells in peripheral blood mononuclear cells after allogeneic cord blood transplantation. Hum Immunol 2009; 70: 701–705.
Jacobson CA, Turki AT, McDonough SM, Stevenson KE, Kim HT, Kao G et al. Immune reconstitution after double umbilical cord blood stem cell transplantation: comparison with unrelated peripheral blood stem cell transplantation. Biol Blood Marrow Transplant 2012; 18: 565–574.
Willemze R, Rodrigues CA, Labopin M, Sanz G, Michel G, Socieål G et al. KIR-ligand incompatibility in the graft-versus-host direction improves outcomes after umbilical cord blood transplantation for acute leukemia. Leukemia 2009; 23: 492–500.
Brunstein CG, Wagner JE, Weisdorf DJ, Cooley S, Noreen H, Barker JN et al. Negative effect of KIR alloreactivity in recipients of umbilical cord blood transplant depends on transplantation conditioning intensity. Blood 2009; 113: 5628–5634.
Garfall A, Kim HT, Sun L, Ho VT, Armand P, Koreth J et al. KIR ligand incompatibility is not associated with relapse reduction after double umbilical cord blood transplantation. Bone Marrow Transplant 2013; 48: 1000–1002.
Willemze R, Ruggeri A, Purtill D, Rodrigues CA, Gluckman E, Rocha V et al. Is there an impact of killer cell immunoglobulin-like receptors and KIR-ligand incompatibilities on outcomes after unrelated cord blood stem cell transplantation? Best Pract Res Clin Haematol 2010; 23: 283–290.
Sideri A, Neokleous N, Brunet De La Grange P, Guerton B, Le Bousse Kerdilles MC, Uzan G et al. An overview of the progress on double umbilical cord blood transplantation. Haematologica 2011; 96: 1213–1220.
Lowe EJ, Turner V, Handgretinger R, Horwitz EM, Benaim E, Hale GA et al. T-cell alloreactivity dominates natural killer cell alloreactivity in minimally T-cell-depleted HLA-non-identical paediatric bone marrow transplantation. Br J Haematol 2003; 123: 323–326.
Yabe T, Matsuo K, Hirayasu K, Kashiwase K, Kawamura-Ishii S, Tanaka H et al. Donor killer immunoglobulin-like receptor (KIR) genotype-patient cognate KIR ligand combination and antithymocyte globulin preadministration are critical factors in outcome of HLA-C-KIR ligand-mismatched T cell-replete unrelated bone marrow transplantation. Biol Blood Marrow Transplant 2008; 14: 75–87.
Krzewski K, Strominger JL . The killer’s kiss: the many functions of NK cell immunological synapses. Curr Opin Cell Biol 2008; 20: 597–605.
Cheent K, Khakoo SI . Natural killer cells: integrating diversity with function. Immunology 2009; 126: 449–457.
Murphy WJ, Parham P, Miller JS . NK cells--from bench to clinic. Biol Blood Marrow Transplant 2012; 18: S2–S7.
De Santis D, Bishara A, Witt CS, Nagler A, Brautbar C, Slavin S et al. Natural killer cell HLA-C epitopes and killer cell immunoglobulin-like receptors both influence outcome of mismatched unrelated donor bone marrow transplants. Tissue Antigens 2005; 65: 519–528.
Dong Z, Cruz-Munoz ME, Zhong MC, Chen R, Latour S, Veillette A . Essential function for SAP family adaptors in the surveillance of hematopoietic cells by natural killer cells. Nat Immunol 2009; 10: 973–980.
Cooley S, Weisdorf DJ, Guethlein LA, Klein JP, Wang T, Le CT et al. Donor selection for natural killer cell receptor genes leads to superior survival after unrelated transplantation for acute myelogenous leukemia. Blood 2010; 116: 2411–2419.
Venstrom JM, Pittari G, Gooley TA, Chewning JH, Spellman S, Haagenson M et al. HLA-C-dependent prevention of leukemia relapse by donor activating KIR2DS1. N Engl J Med 2012; 367: 805–816.
Yawata M, Yawata N, Draghi M, Partheniou F, Little AM, Parham P . MHC class I-specific inhibitory receptors and their ligands structure diverse human NK-cell repertoires toward a balance of missing self-response. Blood 2008; 112: 2369–2380.
Acknowledgements
This study was supported in part by a Grant-in-Aid from the Ministry of Health, Labor and Welfare of Japan and a Japanese Grant-in-Aid for Scientific Research.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 3.0 Unported License. To view a copy of this license, visit http://creativecommons.org/licenses/by-nc-sa/3.0/
About this article
Cite this article
Tanaka, J., Morishima, Y., Takahashi, Y. et al. Effects of KIR ligand incompatibility on clinical outcomes of umbilical cord blood transplantation without ATG for acute leukemia in complete remission. Blood Cancer Journal 3, e164 (2013). https://doi.org/10.1038/bcj.2013.62
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/bcj.2013.62
Keywords
This article is cited by
-
Coexistence of HLA and KIR ligand mismatches as a risk factor for viral infection early after cord blood transplantation
Bone Marrow Transplantation (2022)
-
Improved outcomes of single-unit cord blood transplantation for acute myeloid leukemia by killer immunoglobulin-like receptor 2DL1-ligand mismatch
Bone Marrow Transplantation (2022)
-
Reduced leukemia relapse through cytomegalovirus reactivation in killer cell immunoglobulin-like receptor-ligand-mismatched cord blood transplantation
Bone Marrow Transplantation (2021)
-
Altered effect of killer immunoglobulin-like receptor–ligand mismatch by graft versus host disease prophylaxis in cord blood transplantation
Bone Marrow Transplantation (2021)
-
HLA-DPB1 mismatch induces a graft-versus-leukemia effect without severe acute GVHD after single-unit umbilical cord blood transplantation
Leukemia (2018)