Abstract
Carotid endarterectomy (CEA) is an effective surgical option for stroke prophylaxis in most patients. Restenosis after CEA can lead to re-intervention and adverse events, but the factors predicting restenosis are poorly understood. Apolipoprotein J (ApoJ) is considered to be a novel predictive factor of vascular restenosis and is associated with a large number of processes related to atherosclerosis and cell-cycle phases. The aim of this study was to elucidate the predictive value of Apo J in internal carotid artery (ICA) restenosis following CEA. This retrospective study examined all prospectively collected data for patients who underwent CEA at our surgical department over a 2-year period. The serum ApoJ levels of 100 patients were examined; 56 patients who underwent CEA comprised the vascular group (VG), and 44 patients who underwent minor surgery comprised the control group (CG). ApoJ samples were obtained preoperatively, 24 h after the surgical procedure and at 1, 6 and 12 months thereafter during the follow-up. The preoperative difference in ApoJ levels between the CG and VG was statistically signifcant; the mean values were 39.11±14.16 and 83.03±35.35 μg/mL, respectively. In the VG, the serum ApoJ levels were 112.09±54.40, 71.20±23.70, 69.92±25.76 and 62.25±19.17 μg/mL at postoperative day 1 and at 1, 6 and 12 months post-operatively, respectively, while the ApoJ concentrations of patients in the CG remained unchanged. Further subdivision of the VG into patients with or without restenosis revealed that restenosis patients presented signifcantly higher mean ApoJ values than non-restenosis VG patients. In summary, ApoJ seems to be an important predictor for carotid restenosis at 6 and 12 months postoperatively.
Similar content being viewed by others
Introduction
Carotid endarterectomy (CEA) is the most well-established method for the prevention of stroke due to atherosclerotic disease of the internal carotid artery (ICA)1. The benefit and durability of CEA in preventing stroke have already been published with known results2,3. Restenosis, however, limits the benefit of CEA as it results in an increased incidence of late stroke events and thus creates the need for re-intervention. However, in the last decade, the peri-CEA treatment strategy has been significantly improved with the introduction of Best Medical Treatment (BMT), as suggested by a number of publications and guidelines4,5; however, restenosis remains a major problem6,7,8. Several studies have shown a potential relationship between various factors (eg, homocysteine and lipoprotein a), myointimal hyperplasia and endothelial dysfunction9,10; although this is promising, the exact pathogenesis of carotid atherosclerosis is yet to be defined, and several questions remain unanswered. Apolipoprotein J (ApoJ) or Clusterin is considered a novel predictive factor for vascular restenosis11. In recent years, ApoJ has been studied in new segments of the vascular bed; however, to date, ApoJ remains less investigated than other factors, and conflicting results have been obtained12,13. ApoJ has already been associated with restenosis of the coronary arteries following angioplasty11. Based on this and the current knowledge that ApoJ plays a significant role in a large number of processes related to atherosclerosis and cell-cycle phases, it is speculated that a link between serum ApoJ levels and internal carotid restenosis might exist. The aim of this study was to elucidate the predictive value of ApoJ in ICA restenosis following CEA.
Materials and methods
This is a retrospective analysis of prospectively collected data regarding patients who underwent carotid endarterectomy in our surgical department between November 15st 2012 and November 30st 2014. Before initiating this study, all necessary permissions regarding patient data were obtained from the respective Ethics Committee and were archived for reference purposes.
This study examined the serum ApoJ concentrations of 100 people (Figure 1); of these, 44 healthy individuals with no atherosclerotic disease comprised the Control Group (CG) of the study. These CG patients underwent minimal surgical procedures, such as skin lesion excision for neither inflammatory nor neoplastic cause. During these procedures, no foreign body was implanted. The remaining 56 patients presented significant carotid disease and ICA stenosis, and underwent CEA in our department; these patients comprised the Vascular Group (VG). The recruitment criteria for the VG were asymptomatic carotid disease, significant ICA stenosis requiring CEA, no inflammatory disease, no neoplastic disease, and no peripheral arterial disease of Rutherford grade 3 or higher.
The initial evaluation protocol included blood tests and medical history examination in all cases included in the study. CG patients underwent full physical examination only once during the pre-operative period. In contrast, VG patients were evaluated pre-operatively and on the first post-operative day (POD1) and after the first, sixth and twelfth months post-operatively (POM1, POM6 and POM12, respectively). During follow-ups, blood samples were drawn, and serum ApoJ levels were measured. Duplex scanning was postoperatively performed in both groups of patients at specific intervals (6 and 12 months after the vascular procedure). The Duplex scanning results were evaluated by two independent investigators.
Serum ApoJ samples were analyzed using an Enzyme Linked-Immunosorbent Assay (ELISA) kit (AdipoGen International), and the normal values were determined to be between 0.001 and 5 μg/mL. Spot ApoJ samples were obtained at the following time points: (i) preoperatively, (ii) at 24 h after the surgical procedure, and (iii) at 1, 6 and 12 months thereafter during the follow up. The samples were stored at room temperature for 30 min and then centrifuged for 20 min at 1000×g. The supernatants were stored in aliquots at ≤20 oC.
Patients' demographics (Table 1) were recorded, in addition to their preoperative comorbidities (Table 2), such as the presence of hypertension (HT), diabetes mellitus (DM), hyperlipidemia (HL), and tobacco smoking status. Furthermore, we recorded the Body Mass Index (BMI; >30 kg/m2 considered as obesity) for all participants and the presence or absence of coronary artery disease (CAD), chronic obstructive pulmonary disease (COPD), and kidney injury (KI).
All CEA procedures were performed via transjugular cervical incision by the same team, which was highly experienced in vascular procedures. This incision is routine for this team because it can be extended proximally to the sternal notch for more proximal lesions of the common carotid artery (CCA). On the other hand, upwards extension of the incision towards the mastoid process provides distal exposure. The surgical technique included the regular use of a shunt, tacking sutures at the distal end of the endarterectomy, and vein patch closure of ICA. No reverse endarterectomy was performed.
According to the protocol of our institution, a vacuum drain was placed along the incision site for anastomosis inspection. If no significant bleeding was detected, the drainage was removed on the 1st post-operative day. In our study, significant bleeding was defined as a neck hematoma endangering airway patency while not draining adequately, the draining of more than 600 mL of blood within 12 h, or as the draining of more than 200 mL of blood during any postoperative hour within the first 24 h. On the 1st post-operative day, the patients were allowed a liquid-consistency diet. Blood samples were collected on the first post-operative day. Patients who underwent CEA were discharged on post-operative day 3 if no complications were present. This study included the recording of postoperative follow-up data at 1, 6 and 12 months.
Restenosis in its broadest sense implies a recurrent narrowing at the site of the initial intervention for an atheromatous stenosis. Some authors have also included residual disease, adjacent (untouched) stenosis and technical defects after surgery14. In this study, ICA restenosis was defined as a >50% decrease in diameter (a 75% decrease in area) based on the Duplex criteria of a systolic peak velocity >1.25 m/s or a peak systolic ratio of 2.015,16.
The VG was further divided into two sub-groups depending on whether ICA restenosis was present or absent at the 6- or 12-month follow-up.
Statistical methods
All statistical analysis data are reported as the mean±standard deviation (SD). P values of less than 0.05 (P<0.05) were considered significant. Repeated measures of ANOVA were conducted to determine differences between time points within the same group for each parameter. Furthermore, post hoc analyses were used to identify differences between the two groups. To estimate possible correlations between the restenosis factor for vascular patients and the pre-operative comorbidities and the corresponding values of serum ApoJ, statistical analysis was performed using Pearson's coefficient.
An age-based CG subgroup analysis of serum ApoJ levels was performed using an independent sample paired t-test to understand how age affects ApoJ levels. The cut-off age for dividing the CG into two sub-groups was set at 48.9 years, close to the group's median of 48.88 years.
All results were analyzed using SPSS version 22 (Statistical Package for the Social Sciences Inc, Chicago, IL, USA).
Results
During the study period, 56 consecutive patients meeting the study criteria underwent CEA for treatment of carotid vascular disease. In addition, 44 healthy non-atherosclerotic individuals who underwent minor surgery without inflammatory or neoplastic cause were recruited to the CG. The gender distribution was similar between the two groups (P<0.05). The VG patients yielded significantly greater values for age and BMI than the CG individuals (Table 1).
Regarding to the comorbidities of the examined groups, DM, HT, HL, CAD, COPD and KI occurred in 33.92%, 44.64%, 41.07%, 23.21%, 28.57%, and 3.57% of the VG patients, respectively. By comparison, the healthy population of the CG had significant lower incidences of these diseases: 9.08%, 18.16%, 33.33%, 11.35%, 13.63%, and 2.27%, respectively (Table 2). Furthermore, tobacco smoking was more frequent among the VG patients with an incidence rate of 57.14% compared to 36.32% for the CG patients (P<0.05).
Our follow-up compliance rates on the first post-operative day and at the first, sixth, and twelfth months were 98.21%, 92.85%, 85.76%, and 85.76%, respectively. In total, 5 patients were lost during the follow-up period, and 3 were passed-away due to CEA-unrelated medical reasons.
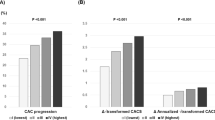
The difference in pre-operative serum ApoJ levels between the CG and VG was significant (P<0.05), and the mean values were 39.11±14.16 and 83.03±35.35 μg/mL, respectively. During the follow-up period, serum ApoJ levels in the VG varied and insignificantly decreased, although these VG ApoJ levels remained significantly higher than the respective values in the CG. Serum ApoJ levels in the VG were 112.09±54.40, 71.20±23.70, 69.92±25.76 and 62.25±19.17 μg/mL on the 1st post-operative day and at the 1st, the 6th and 12th post-operative months, respectively. In contrast, CG serum ApoJ levels remained unchanged during the follow-up period, as the patients in the CG remained free of vascular disease (Figure 2).
Following that, we further divided the VG into two subgroups as follows: a) patients with restenosis following CEA and b) patients without restenosis following CEA, and the link between ApoJ and restenosis was studied. Restenosis was determined as >50% stenosis of the CEA site, as confirmed via Duplex scanning examination performed by two separate investigators. No early restenosis was confirmed with an early post-operative Duplex scanning to confirm the fordable of the anastomosis. Pre-operative mean serum ApoJ levels were a significant prognostic factor for restenosis in the VG (Table 4).
The non-restenosis VG subgroup suffered from DM, HT, HL, CAD, COPD and tobacco smoking at incidence rates of 40%, 48.57%, 31.42%, 57.14%, 25.71%, and 34.28%, respectively (Table 3), whereas the post-CEA restenosis VG patients had incidence rates of 38.46%, 61.53%, 92.3%, 92.3%, 30.76%, and 30.76%, respectively (Table 3). The incidence rates of HT, HL, and CAD were significantly higher (P<0.05) in the stenosis sub-group than in the non-restenosis sub-group. On the other hand, the incidence rates of DM, COPD, and KI were higher in the VG patients with no restenosis; although DM incidence was not significantly higher, KI incidence was significantly higher (P<0.05) in the non-restenosis subgroup than in the restenosis subgroup.
Thirteen of the 48 VG patients had ICA restenosis at 6 months, resulting in a 27% overall restenosis rate. At 12 months, there were no new occurrences of restenosis other than in the previously diagnosed 13 patients. Pre-operative mean serum ApoJ levels were significantly lower in patients who later had restenosis compared to those who did not (P<0.05). ApoJ levels were significantly higher in the non-restenosis group on POD1 (P<0.05). This finding was partially reversed at POM1, when a similar variance existed among ApoJ levels in the two VG subgroups (P<0.05). At both the 6th and the 12th post-operative months, VG patients with restenosis presented significantly higher mean ApoJ values than non-restenosis VG patients (P<0.05) (Figure 3). Serum ApoJ levels are shown in Table 4.
Serum levels of ApoJ in patients with and without internal carotid artery restenosis. NS=No significant difference. *=Significant difference with higher values in the Control group (P<0.05). #=Significant difference with higher values in the restenosis group (P<0.05). POM= Post-Operative Month. POD=Post-Operative Day
The correlations among preoperative comorbidities, ICA restenosis and ApoJ levels were also examined. Statistical analysis revealed that restenosis at POM6 was linked with the levels of serum ApoJ with pre-operative HT, CAD, HL and tobacco smoking in a proportionate manner (P<0.05). Regarding restenosis occurrence at POM12, statistical analysis revealed that the mean value of serum ApoJ was significantly correlated with the incidence of CAD, HL and tobacco smoking (P<0.05).
An age subgroup analysis comparing CG patients over the age of 48.9 years with those under the age of 48.9 years demonstrated a non-significant difference in the ApoJ levels of the two groups; however, both groups had significantly lower ApoJ levels when compared to the VG group.
Discussion
The aim of this study was to examine and clarify whether ApoJ can be used as a predictive factor for ICA restenosis post-CEA. At present, ICA restenosis occurring post-CEA remains a significant treatment dilemma for vascular surgeons because the restenosis threshold over which patients should undergo new surgical or endovascular treatment is controversial. Therefore, post-CEA ICA restenosis is a current medical problem that remains to be addressed. ICA restenosis occurs in a bimodal distribution. Neointimal hyperplasia is considered the main cause of restenosis within the first 2 post-operative years after CEA, but restenosis is considered to be the result of underlying atherosclerotic disease thereafter8.
Serum ApoJ levels in the healthy individuals comprising the control group (CG), who underwent minor surgical procedures such as excision of skin lesions, remained at the same low values both before and after the procedure. Although constant serum ApoJ concentrations were expected for patients in the CG, it was necessary to demonstrate that minor surgical procedures and manipulations do not alter ApoJ levels because ApoJ does not contribute to postoperative wound healing and tissue remodeling. Therefore, it is safe to conclude that the constant levels of serum ApoJ in the CG patients provide evidence supporting the above hypothesis, although a study involving a larger population and including various surgical procedures carried out on the CG patients should be conducted.
Previously, it has been reported that ApoJ levels are elevated in patients with significant atherosclerotic load, coronary disease and/or in older patients compared to healthy non-atherosclerotic individuals17,18. Compared to CG ApoJ levels, VG serum ApoJ levels were significantly higher during the interval from the pre-operative period to POM12 (Figure 2). This result is partially expected because ApoJ has a biosensing role and is triggered by inflammation and upregulated by atherosclerosis1, and atherosclerosis plays a central role in ICA stenosis.
It could be argued that the higher ApoJ levels in the VG patients are related to the significantly older age of these patients compared to CG19; however, after performing an age subgroup analysis for the CG patients, no significant difference in the ApoJ levels of the two age sub-groups was found. This shows that although CG patients older than 48.9 years presented insignificantly higher ApoJ levels compared to the younger CG patients, they had significantly lower ApoJ levels compared to the VG patients. Therefore, it can be concluded that age is not the main factor affecting ApoJ levels or that it is a less influential factor than atherosclerosis. Another mechanism by which age might affect the ApoJ concentration is that atherosclerotic load increases with age19.
A more complicated picture emerges when the peri-operative ApoJ levels of the two VG sub-groups are compared. The restenosis VG subgroup showed a statistically significant increase of ApoJ at POM6 and POM12; however, importantly, the restenosis subgroup had paradoxically and significantly lower preoperative ApoJ levels than the non-restenosis subgroup. ApoJ is involved in numerous physiological intracellular and extracellular processes. Apart from the role of ApoJ in lipid transportation, it also plays a significant role in the differentiation of vascular smooth muscle cells (VSMCs), immune system regulation, and oxidative stress. As a result, ApoJ plays a role in the atherosclerotic process by relieving the atherosclerotic load. ApoJ also exhibits cytoprotective and anti-inflammatory actions and interacts with a plethora of known inflammatory proteins, such as C-reactive protein. In the blood, ApoJ interacts with ApoA-I and ApoE particles, forming high-density lipids (HDLs), which are known to protect the aortic wall against atherosclerosis. ApoJ has also been identified to alter the process of VSMC migration, adhesion, and proliferation, contributing to restenosis after vascular wall injury11. Although all these mechanisms explain the lower pre-operative ApoJ levels in the restenosis subgroup, further investigation of this pre-operative finding is warranted.
Post-operative ApoJ levels at POD1 and POM1 were similar between the two VG sub-groups. At the POM6 follow-up, 13 patients presented restenosis and significantly higher ApoJ levels compared to the other VG patients. This statistically significant difference persisted at the POM12 follow-up, although the absolute value declined. The ApoJ levels of the restenosis VG subgroup never decreased to become equal to or lower than the respective pre-operative levels, while the non-restenosis subgroup had ApoJ levels lower than the pre-operative levels by POM1 up to POM12.
The higher pre-operative ApoJ concentration in the non-restenosis subgroup and the decreasing ApoJ concentrations in both sub-groups over time might also be all related to differences in the complex processes and triggering of the ApoJ clusters, both nuclear and secretory. This imbalance between the two ApoJ clusters and the two contradictory effects of the respective clusters on atherosclerosis have recently been reported, but the mechanism behind these findings remains unverified20. The higher pre-operative ApoJ level in the non-restenosis subgroup might also be explained by the fact that ApoJ could be upregulated by the presence of the atherosclerotic plaque in the ICA, and once this atherosclerotic plaque is removed, VSMC proliferation does not represent a strong enough stimulus to trigger a high ApoJ concentration. This hypothesis would also explain why the ApoJ concentration increased over time in the stenosis subgroup.
Based on these findings, some conclusions can be reached. A low pre-operative ApoJ level and a consistently higher post-operative ApoJ level compared to pre-operative levels by POM1 and later could be related to the development of ICA restenosis. On the contrary, high pre-operative levels are not indicative of future ICA restenosis, which is supported by the fact that ApoJ levels gradually decreased below the pre-operative concentration by POM1. Therefore, the predictive role of ApoJ for post-CEA ICA restenosis might be grounded in the trend of increasing ApoJ concentrations at POM1 or later compared to the corresponding pre-operative value.
Based on our results, it is clear that the significantly higher ApoJ levels in the VG compared to the CG and the significant increase of ApoJ levels in the restenosis VG subgroup, which is proportional to postoperative time after POM6, demonstrate a clear link between ICA atherosclerosis and restenosis and ApoJ levels.
Apart from the ApoJ levels, a number of comorbidities (DM, HT, HL, CAD, COPD, KI) and tobacco smoking were also studied in the two groups (VG and CG) as well as in the two VG subgroups. Patients in the VG group presented a significantly higher incidence of all the studied comorbidities apart from KI. The restenosis subgroup presented a significantly higher incidence of HT, HL, and CAD (all are related to atherosclerosis) but a significantly lower incidence of DM, COPD, and KI compared to the non-restenosis subgroup. Tobacco smoking was more frequent in the VG than in the CG and was also more frequent in the restenosis VG subgroup compared to the non-restenosis subgroup.
This study had several limitations. The small number of patients recruited in the VG group might not provide sufficient statistical evidence supporting the final conclusions. The number of patients is considered sufficient for an initial evaluation of the predictive value of ApoJ for post-CEA ICA restenosis, but a study involving a larger population is necessary to confirm and further support the findings. The lower preoperative ApoJ level in the restenosis subgroup compared to the non-restenosis patients is partially explained by the different roles of the two ApoJ clusters, but this should also be confirmed in a larger study. Age affects ApoJ levels in an unknown manner, and despite our age subgroup analysis, future studies should compare groups of patients with insignificant age differences to minimize the effect of age on the ApoJ levels of the subjects.
This study demonstrates that Apo J is a significant and independent predictor for carotid restenosis at POM6 and POM12 follow-ups. Tobacco smoking, HT, HL and CAD were all significantly associated with post-CEA ICA restenosis.
Despite the promising findings obtained, all of the conclusions need further support from more extensive studies to provide a clear understanding of the complex pathways by which ApoJ affects both VSMCs and the atherosclerotic process. A very interesting point to explore in future studies would be to determine the time interval between POM1 and POM6 at which ApoJ levels between restenosis and non-restenosis subgroups differ significantly but at which ICA restenosis has not yet occurred.
Author contribution
Anastasios MASKANAKIS, Despina PERREA, Sotirios GEORGOPOULOS, and Chris BAKOYIANNIS designed research; Anastasios MASKANAKIS, Nikolaos PATELIS, and Georgios KARAOLANIS wrote the paper; Anastasios MASKANAKIS, Spyridon DAVAKIS, Chris KLONARIS, Sotirios GEORGOPOULOS, and Chris BAKOYIANNIS collected data; Spyridon DAVAKIS and Dimitrios SCHIZAS analyzed data; Anastasios MASKANAKIS and Nikolaos PATELIS revised manuscript; Nikolaos PATELIS and Spyridon DAVAKIS revised manuscript; Anastasios MASKANAKIS, Theodoros LIAKAKOS, Dimitrios SCHIZAS, Despina PERREA, Chris KLONARIS, Sotirios GEORGOPOULOS, and Chris BAKOYIANNIS critically reviewed the paper.
References
Ballotta E, Da Giau G, Piccoli A, Baracchini C. Durability of carotid endarterectomy for treatment of symptomatic and asymptomatic stenoses. J Vasc Surg 2004; 40: 270–8.
Executive Committee for the Asymptomatic Carotid Atherosclerosis Study. Endarterectomy for asymptomatic carotid artery stenosis. JAMA 1995; 273: 1421–8.
Babu MA, Meissner I, Meyer FB. The durability of carotid endarterectomy: long-term results for restenosis and stroke. Neurosurgery 2013; 72: 835–8
Paraskevas KI, Mikhailidis DP, Veith FJ, Spence JD. Definition of best medical treatment in asymptomatic and symptomatic carotid artery stenosis. Angiology 2016; 67: 411–9.
Paraskevas KI, Mikhailidis DP, Veith FJ. Comparison of the five 2011 guidelines for the treatment of carotid stenosis. J Vasc Surg 2012; 55: 1504–8.
Naylor R, Hayes PD, Payne DA, Allroggen H, Steel S, Thomson MM, et al. Randomized trial of vein versus Dacron patching during carotid endarterectomy: long term results. J Vasc Surg 2004; 39: 985–93.
Arquizan C, Trinquart L, Touboul PJ, Long A, Feasson S, Terriat B, et al. Restenosis is more frequent after carotid stenting than after endarterectomy: the EVA-3S study. Stroke 2011; 42: 1015–20.
Goel SA, Guo LW, Liu B, Kent KC. Mechanisms of post-intervention arterial remodelling. Cardiovasc Res 2012; 96: 363–71.
Bakoyiannis C, Karaolanis G, Moris D, Palla V, Skrapari I, Bastounis E, et al. Homocysteine as a risk factor of restenosis after carotid endarterectomy. Int Angiol 2015; 34: 166–71.
Miner SE, Hegele RA, Sparkes J, Teitel JM, Bowman KA, Connelly PW, et al. Homocysteine, lipoprotein(a), and restenosis after percutaneous transluminal coronary angioplasty: a prospective study. Am Heart J 2000; 140: 272–8.
Yang N, Qin Q. Apolipoprotein J: a new predictor and therapeutic target in cardiovascular disease? Chin Med J 2015; 128: 2530.
Park S, Mathis KW, Lee IK. The physiological roles of apolipoprotein J/clusterin in metabolic and cardiovascular diseases. Rev Endocr Metab Disord 2014; 15: 45–53.
Trougakos IP. The molecular chaperone apolipoprotein J/clusterin as a sensor of oxidative stress: implications in therapeutic approaches - a mini-review. Gerontology 2013; 59: 514–23.
Sadideen H, Taylor PR, Padayachee TS. Restenosis after carotid endarterectomy. Int J Clin Pract 2006; 60:1625–30.
Aburahma AF. Duplex criteria for determining ≥50% and ≥80% internal carotid artery stenosis following carotid endarterectomy with patch angioplasty. Vascular 2011; 19: 15–20.
Horrocks M. When should I reoperate for recurrent stenosis. In: Carotid artery surgery: a problem-based approach. London: Harcourt Publishers Ltd; 2000. p 371–374.
In: Naylor AR, Mackey WC, eds. Carotid artery surgery: a problem-based approach. London: Harcourt Publishers Ltd; 2000. p 371–4
Bürkle A, Moreno-Villanueva M, Bernhard J, Blasco M, Zondag G, Hoeijmakers JH, et al. MARK-AGE biomarkers of ageing. Mech Ageing Dev 2015; 151: 2–12.
Poulakou MV, Paraskevas KI, Wilson MR, Iliopoulos DC, Tsigris C, Mikhailidis DP, et al. Apolipoprotein J and leptin levels in patients with coronary heart disease.In vivo 2008; 22: 537–42.
Antonelou MH, Kriebardis AG, Stamoulis KE, Trougakos IP, Papassideri IS. Apolipoprotein J/Clusterin is a novel structural component of human erythrocytes and a biomarker of cellular stress and senescence. PLoS One 2011; 6: e26032.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Maskanakis, A., Patelis, N., Karaolanis, G. et al. Apolipoprotein J as a predictive biomarker for restenosis after carotid endarterectomy: a retrospective study. Acta Pharmacol Sin 39, 1237–1242 (2018). https://doi.org/10.1038/aps.2017.146
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2017.146
Keywords
This article is cited by
-
Circulating biomarkers for cardiovascular diseases: the beats never stop
Acta Pharmacologica Sinica (2018)