Abstract
Aim:
The augmentation of late sodium current (INa.L) not only causes intracellular Na+ accumulation, which results in intracellular Ca2+ overload via the reverse mode of the Na+/Ca2+ exchange current (reverse-INCX), but also prolongs APD and induces early afterdepolarizations (EAD), which can lead to arrhythmia and cardiac dysfunction. Thus, the inhibition of INa.L is considered to be a potential way for therapeutic intervention in ischemia and heart failure. In this study we investigated the effects of tolterodine (Tol), a competitive muscarinic receptor antagonist, on normal and veratridine (Ver)-augmented INa.L, reverse-INCX and APD in isolated rabbit ventricular myocytes, which might contribute to its cardioprotective activity.
Methods:
Rabbit ventricular myocytes were prepared. The INa.L and reverse-INCX were recorded in voltage clamp mode, whereas action potentials and Ver-induced early afterdepolarizations (EADs) were recorded in current clamp mode. Drugs were applied via superfusion.
Results:
Tol (3–120 nmol/L) concentration-dependently inhibited the normal and Ver-augmented INa.L with IC50 values of 32.08 nmol/L and 42.47 nmol/L, respectively. Atropine (100 μmol/L) did not affect the inhibitory effects of Tol (30 nmol/L) on Ver-augmented INa.L. In contrast, much high concentrations of Tol was needed to inhibit the transient sodium current (INa.T) with an IC50 value of 183.03 μmol/L. In addition, Tol (30 nmol/L) significantly shifted the inactivation curve of INa.T toward a more depolarizing membrane potential without affecting its activation characteristics. Moreover, Tol (30 nmol/L) significantly decreased Ver-augmented reverse-INCX. Tol (30 nmol/L) increased the action potential duration (APD) by 16% under the basal conditions. Ver (20 μmol/L) considerably extended the APD and evoked EADs in 18/24 cells (75%). In the presence of Ver, Tol (30 nmol/L) markedly decreased the APD and eliminated EADs (0/24 cells).
Conclusion:
Tol inhibits normal and Ver-augmented INaL and decreases Ver-augmented reverse-INCX. In addition, Tol reverses the prolongation of the APD and eliminates the EADs induced by Ver, thus prevents Ver-induced arrhythmia.
Similar content being viewed by others
Introduction
Previous studies indicated that late sodium current (INa.L), which is tetrodotoxin (TTX)-sensitive1, was increased under various pathological conditions, such as long QT syndrome III, myocardial hypertrophy, heart failure, ischemia, anoxia, and oxidative stress2,3,4,5,6,7,8,9,10. Although it has a much smaller amplitude than the transient sodium current (INa.T) under normal conditions, INa.L plays an important role in determining the plateau of action potential (AP) and action potential duration (APD) under the above pathological conditions11,12. The augmentation of INa.L not only causes intracellular Na+ accumulation, which results in intracellular Ca2+ overload via the reverse mode of the Na+/Ca2+ exchange current (INCX), but also prolongs APD and induces early afterdepolarizations (EAD)11,12,13,14,15,16,17, which can lead to arrhythmia and cardiac dysfunction. Thus, the inhibition of INa.L is considered to be a potential target for therapeutic intervention in ischemia and heart failure1,11,12,13,18,19,20,21,22,23. Although several compounds, including RSD123524 and AZD700925, have been reported to block INa.L, their effective doses were above micromolar26,27. Moreover, these drugs inhibit INa.L and INa.T simultaneously, which can induce cardiac conduction block. Currently, only ranolazine has been approved by the FDA as an effective INa.L blocker for clinical use3,1318,28,29. GS-458967, another efficient INa.L specific inhibitor, has not yet been approved for clinical use and was found to have some potential adverse effects to the central nervous system and peripheral nervous system29. Thus, more research on high affinity INa.L blockers is urgently needed.
Tolterodine (Tol), a muscarinic antagonist, is used in the symptomatic treatment of patients with frequent micturition, urgent micturition and urinary incontinence induced by bladder overactivity, with a peak serum concentration of 7–58 nmol/L30. Recently, Tol has been reported to affect cardiac ion channels30,31. Kang et al reported that Tol could inhibit HERG channel currents (IKr on human) expressed on CHO cells and L-type calcium currents (ICa.L) in guinea pig ventricular myocytes, with an IC50 of 17, 143 (1 Hz), and 1084 nmol/L (0.1 Hz), respectively. The APD at 90% repolarization (APD90) was increased by 4%, 8%, and 16%, respectively, in the presence of 3, 10, and 30 nmol/L Tol in guinea pig ventricular myocytes. Based on these results, Kang et al concluded that Tol did not prolong APD significantly because it blocked both HERG and L-type calcium channels, thus offsetting the effects on APD31. However, this conclusion needs to be further verified. For example, 30 nmol/L Tol significantly inhibited HERG current but slightly decreased ICa.L; thus, in this condition, the prolongation of APD90 should far exceed 16%, which was different from the reported result of a 16% increase in APD90. Furthermore, QT interval prolongation was rarely observed in patients with the application of Tol32,33. We speculate that Tol can inhibit other inward currents associated with APD. Veratridine (Ver)34, an activator of INa.L, is suitable for evoking EAD because it can increase APD to the required extent35,36. Accordingly, this study aims to explore the possible antiarrhythmic mechanisms of Tol by investigating the effects of Tol on normal and Ver-induced INa.L, reverse INCX and APD in rabbit ventricular myocytes.
Materials and methods
Cardiomyocyte isolation
Rabbits of either sex, weighing 1500–2000 g, were purchased from the Animal Experimental Center of Wuhan University of Science and Technology, Wuhan, China, and were anesthetized with ketamine (Fujian Gutian Pharmaceutical Co, Ltd, Gutian, Fujian, China, 30 mg/kg iv) and xylazine (Shanghai Shifeng Biological Technology Co, Ltd, Shanghai, China, 7.5 mg/kg im) 10 min after an intravenous injection of 2000 U of heparin. All efforts were made to minimize animal discomfort and suffering during the experimental process. The heart was excised and retrogradely perfused on a modified Langendorff apparatus with Ca2+-free Tyrode's solutions bubbled with 100% O2 and maintained at 37 °C. The heart was then perfused with Ca2+-free Tyrode's solution containing collagenase type I (0.1 mg/mL) and BSA (0.5 mg/mL) for 40–50 min, and then with KB solution for another 5 min. The left ventricle was cut into small chunks and gently agitated in KB solution. The cells were filtered through nylon mesh and stored in KB solution at 4 °C. The use of animals in this investigation conformed to “the Guide for the Care and Use of Laboratory Animals Regulated by Administrative Regulation of Laboratory Animals of Hubei Province” and was approved by the Institutional Animal Care and Use Committee of the Medical College of Wuhan University of Science and Technology (Wuhan, China).
Whole-cell patch-clamp technique
The conventional whole-cell patch-clamp technique using an EPC-10 amplifier (HEKA Electronic, Lambrecht, Germany) was applied to record transmembrane potentials and ion currents in either current clamp or voltage clamp mode. Patch electrodes were pulled with a two-stage puller (PP-83, Narishige Group, Tokyo, Japan), and their resistances were in the range of 1.0–1.5 MΩ after filling with pipette solution. An 80% compensation of series resistance was achieved without ringing. Currents were filtered at 2 kHz, digitized at 10 kHz, and stored on a computer hard drive for further analysis. All experiments were performed at room temperature (22–24 °C).
The current-voltage (I–V) relationship of INa.L was determined by 300 ms depolarizing pulses to potentials ranging from −90 mV to +40 mV in 10 mV increments from a holding potential of −120 mV. INa.L was measured at the 200 ms of the depolarizing pulse to avoid the influence of INa.T on INa.L37. The voltage dependence of steady-state inactivation for INa.T was determined using 100 ms conditioning pulses from a holding potential of −120 mV, ranging from −100 mV to −45 mV in 5 mV increments, followed by a test pulse to −10 mV for 100 ms. The voltage dependence of steady-state activation for INa.T was determined using a holding potential of −120 mV, ranging from −90 mV to +60 mV in 5 mV increments. The maximum value of INa.T was measured. The INCX was induced by a ramp-pulse protocol ranging from +60 mV to −120 mV continuing for 2000 ms from a holding potential of −40 mV. INCX was measured as the current sensitive to 5 mmol/L Ni2+ at +50 and −100 mV. AP was recorded in current clamp mode by using whole-cell patch-clamp techniques and was evoked by depolarizing current pulses (5 ms duration, 1.5 times the threshold intensity, 0.25 Hz) in ventricular myocytes.
Solutions
Regular Tyrode's solution contained the following (in mmol/L): 135 NaCl, 5.4 KCl, 1 MgCl2, 1.8 CaCl2, 0.33 NaH2PO4, 10 HEPES and 10 glucose (pH 7.4, adjusted with NaOH).
The KB solution contained the following (in mmol/L): 70 KOH, 40 KCl, 3 MgCl2, 20 KH2PO4, 0.5 EGTA, 50 L-glutamic acid, 20 taurine, 10 HEPES, and 10 glucose (pH 7.4, adjusted with KOH).
To record INa.L, the pipette solution contained the following (in mmol/L): 120 CsCl, 1 CaCl2, 5 MgCl2, 5 Na2ATP, 10 TEACl, 11 EGTA and 10 HEPES (pH 7.3, adjusted with CsOH). The bath solutions contained the following (in mmol/L): 135 NaCl, 5.4 CsCl, 1.8 CaCl2, 1 MgCl2, 0.3 BaCl2, 0.33 NaH2PO4, 10 HEPES, 10 glucose and 0.001 nicardipine (pH 7.4, adjusted with NaOH).
To record INa.T, the pipette solution contained the following (in mmol/L): 120 CsCl, 1 CaCl2, 5 MgCl2, 5 Na2ATP, 10 TEACl, 11 EGTA, and 10 HEPES (pH 7.3, adjusted with CsOH). The bath solutions contained the following (in mmol/L): 30 NaCl, 105 CsCl, 1 CaCl2, 1 MgCl2, 0.001 nicardipine, 10 HEPES and 10 glucose (pH 7.4, adjusted with CsOH).
To record INCX, the pipette solution contained the following (in mmol/L): 120 CsOH, 20 NaCl, 10 CaCl2, 50 aspartic acid, 3 MgCl2, 20 EGTA, 5 MgATP and 10 HEPES (pH 7.3, adjusted with CsOH). The bath solution contained the following (in mmol/L): 140 NaCl, 2 CaCl2, 2 MgCl2, 5 HEPES and 10 glucose (pH 7.4, adjusted with NaOH). In addition, 20 μmol/L ouabain, 1.0 mmol/L BaCl2, 2.0 mmol/L CsCl and 1.0 μmol/L nicardipine were added to block Na+/K+ exchange current, potassium current and ICa.L, respectively.
To record AP, the pipette solution contained the following (in mmol/L): 120 potassium aspartate, 1 CaCl2, 1 MgSO4, 4 Na2ATP, 0.25 Na3GTP and 10 HEPES (pH 7.3, adjusted with KOH). The bath solution was Tyrode's solution.
Drugs and reagents
TTX and collagenase type I were provided by Tocris (Ellisville, MO, USA) and Gibco (Invitrogen, Paisley, UK), respectively. BSA, taurine, and HEPES were purchased from Roche (Basel, Switzerland). All other chemicals were obtained from Sigma Chemical (Saint Louis, MO, USA). Tol and Ver were stored in the dark at room temperature and −20 °C, respectively. On the day of experimentation, these two drugs were dissolved in dimethyl sulfoxide to create stock solutions from which test solutions were made. The stock solution was diluted with cell external solution to achieve the desired final concentrations immediately before the experiments. The final concentration of dimethyl sulfoxide was less than 0.1%. When the two drugs were used sequentially in an experiment, we applied the second drug after the effect of the first drug achieved a stable level.
Data analysis
All data are presented as the mean±SD and were analyzed using FitMaster (v2x32, HEKA) and SPSS 13.0 software. Current density (pA/pF), ie, the amplitude of the current divided by membrane capacitance, was used for analysis. Figures were plotted with Origin (V7.5, OriginLab Co, MA, USA). Student's t-test was used to determine the difference between two groups of data. Statistical analysis was performed using one-way analyses of variance (ANOVA), followed by the Scheffé test for multiple comparisons. A P-value<0.05 was considered statistically significant.
Current tracings were fitted using Hill or Boltzmann functions with Origin 7.5. The fractional blockade was calculated using the following equation: Fractional blockade=(Icontrol–Idrug)/Icontrol, where Icontrol and Idrug are the current amplitudes in the absence and presence of Tol, respectively. Concentration-effect curves were fitted using the Hill equation as follows: (Icontrol–Idrug)/Icontrol=Bmax/[1+(IC50/D)n], where Bmax was the maximum blockade of currents, IC50 was the concentration of Tol for half-maximum blockade, D was the concentration of Tol, and n was the Hill coefficient. For all IC50 values, all current levels were measured at −20 mV.
Steady-state activation data and inactivation relationships of INa.T were fitted to the Boltzmann equation as follows: Y=1/[1+exp(Vm–V1/2)/k], where Vm was the membrane potential, V1/2 was the half-activation or half-inactivation potential, and k was the slope factor. For the steady-state activation and inactivation curve, Y stood for the relative conductance (G/Gmax) and relative current (I/Imax), respectively.
Results
Effects of Tol on INa.L under normal conditions
INa.L was recorded with 300 ms voltage steps from a holding potential of −120 mV to −20 mV at 0.5 Hz. After the application of 4 μmol/L TTX, INa.T did not change significantly, whereas INa.L was almost completely blocked with densities changing from 0.335±0.017 to 0.076±0.012 (n=8, P<0.01 vs control; Figure 1). In addition, the increased currents induced by 20 μmol/L Ver (from 0.253±0.015 to 1.613±0.032) were almost completely blocked by 4 μmol/L TTX (0.081±0.009; n=6, P<0.01 vs 20 μmol/L Ver; Figure 1A). These results showed that the increased recorded currents were exactly INa.L (Figure 1A).
Effects of tolterodine (Tol) on normal INa.L in rabbit ventricular myocytes. (A) The blockade of 4 μmol/L TTX on normal and Ver-increased INa.L. (B) Typical whole-cell INa.L traces recorded in the absence (control) and presence of 10, 30, and 120 nmol/L Tol. (C) The effects of Tol on the current-voltage relationship of INa.L. *P<0.05, **P<0.01 vs control. (D) The concentration-effect curves were plotted based on data from panel C and fitted using the Hill equation (used all currents values at −20 mV).
The current-voltage relationship of INa.L was recorded. Tol (6, 10, 30, or 120 nmol/L) inhibited INa.L in a concentration-dependent manner (Figure 1B, 1C). The inhibition rates of INa.L (at −20 mV) were 11.7%±2.1% (n=10, P<0.05 vs control), 29.7%±9.0% (n=10, P<0.01 vs 6 nmol/L), 54.2%±9.3% (n=10, P<0.01 vs 10 nmol/L), 79.4%±9.6% (n=10, P<0.05 vs 30 nmol/L) at 6, 10, 30, 120 nmol/L Tol, respectively, and the value of IC50 was 32.08 nmol/L (Figure 1).
Effects of Tol on increased INa.L induced by Ver
At 20 μmol/L, Ver increased currents densities of INa.L from 0.448±0.015 to 1.601±0.062 (n=10, P<0.01). Tol (3, 6, 10, 30, or 120 nmol/L) suppressed increased INa.L induced by Ver in a concentration-dependent manner (Figures 2A–2C). The inhibition rates of INa.L (at −20 mV) were 8.3%±1.1% (n=10, P<0.05 vs 20 μmol/L Ver), 12.9%±3.2% (n=10, P<0.01 vs 3 nmol/L Tol), 32.4%±5.2% (n=10, P<0.01 vs 6 nmol/L Tol), 49.9%±8.9% (n=10, P<0.05 vs 10 nmol/L Tol), and 68.6%±9.0% (n=10, P<0.05 vs 30 nmol/L Tol) at 3, 6, 10, 30, 120 nmol/L Tol, respectively. The value of IC50 was 42.47 nmol/L (Figure 2D, 2E).
Effects of tolterodine (Tol) on increased INa.L induced by Ver in rabbit ventricular myocytes. (A) Tol 10, 30, and 120 nmol/L suppressed increased INa.L by 20 μmol/L Ver in a concentration-dependent manner. (B) The current recordings at −20 mV from Panel A. (C) Effects of Tol at 3–120 nmol/L on the current-voltage relationship of INa.L induced by 20 μmol/L Ver. *P<0.05, **P<0.01 vs 20 μmol/L Ver. (D) The concentration-effect curves were plotted based on data from panel C (at −20 mV) and fitted using the Hill equation. (E) The time courses of effects of Ver and Tol on INa.L (at −20 mV). (F) In the presence of 100 μmol/L atropine, 30 nmol/L Tol decreased the increased INa.L by 20 μmol/L Ver.
Effects of atropine on increased INa.L induced by Ver
We studied whether the blocking effect of Tol on INa.L was achieved by its binding to the muscarinic (M) receptor. Atropine, a high-performance M receptor antagonist, was used. After the application of 20 μmol/L Ver, the current density of INa.L was increased from 0.310±0.008 pA/pF to 1.668±0.048 pA/pF (n=8, P<0.01) and was not significantly changed after giving 100 μmol/L atropine (1.656±0.039 pA/pF, n=8, P>0.05 vs Ver). However, after the application of 30 nmol/L Tol, the current density of INa.L was decreased to 0.689±0.019 pA/pF (n=8, P<0.01 vs atropine, Figures 2F). These results indicated that Tol's blockade of INa.L was independent of its effect on the M receptor signaling pathway.
Effects of Tol on INa.T
At concentration of 1 μmol/L Tol did not change the density of INa.T (n=10, P>0.05 vs control), whereas 10, 30, 100, and 300 μmol/L Tol decreased the magnitudes of INa.T in a concentration-dependent manner (Figure 3A). The suppression rates of INa.T (at −20 mV) were 14.2%±2.3% (n=10, P<0.05 vs 1 μmol/L Tol), 25.8%±5.3% (n=10, P<0.01 vs 10 μmol/L Tol), 43.7%±5.4% (n=10, P<0.01 vs 30 μmol/L Tol), and 55.3%±6.8% (n=10, P<0.05 vs 100 μmol/L Tol) at 10, 30, 100, and 300 μmol/L Tol, respectively, and the value of IC50 was 183.03 μmol/L (Figures 3A, 3B).
Effects of Tol on INa.T on rabbit ventricular myocytes. (A) The effects of Tol (1, 10, 30, 100, or 300 μmol/L) on the current-voltage relationships of INa.T. *P<0.05, **P<0.01 vs control. (B) The concentration-effect curves are plotted based on data from panel A and fitted using the Hill equation.
The steady-state activation and inactivation curves for INa.T were also examined. For the steady-state activation of INa.T, the values of V1/2 were −39.23±0.08 mV and −39.64±0.11 mV (n=7, P>0.05), and the values of k were 4.29±0.07 and 3.89±0.10 (n=7, P>0.05) before and after application of 30 nmol/L Tol, respectively (Figure 4A, 4B). The steady-state inactivation of INa.T, V1/2 changed from −74.69±1.68 mV to −68.08±0.35 mV (n=7, P<0.05) after the application of 30 nmol/L Tol, and k changed from 11.31±2.07 to 6.41±0.32 (n=7, P<0.05) (Figure 4C, 4D). The inactivation curves of INa.T shifted towards more positive potential with 30 nmol/L Tol.
Effects of Tol on steady-state activation and inactivation of INa.T in rabbit ventricular myocytes. (A and C) The steady-state activation and inactivation current recordings of INa.T in myocytes before and after superfusion with 30 nmol/L Tol. (B and D) The steady-state activation and inactivation curves of INa.T before and after application of 30 nmol/L Tol. Conductivities were normalized against the maximum conductivity on each condition (B). Currents were normalized against the maximum currents at −100 mV for each cell (D). The data were fitted using the Boltzmann equation.
Effects of Tol on reverse INCX induced by Ver
At concentration of 20 μmol/L Ver increased the forward INCX from −0.872±0.102 pA/pF to −1.165±0.109 pA/pF (n=10, P<0.05) and the reverse INCX from 2.806±0.235 pA/pF to 4.101±0.304 pA/pF (n=10, P<0.01). In the presence of 20 μmol/L Ver, 30 nmol/L Tol decreased these values to −0.933±0.109 pA/pF and 3.357±0.259 pA/pF (n=10, P<0.05 vs Ver for both), respectively (Figures 5A–5C). In another group experiment, 4 μmol/L TTX also inhibited the increased forward and reverse INCX induced by Ver (Figures 5D–5F).
Effects of Tol and TTX on increased INCX induced by Ver. (A and D) The current-time relationship curves were constructed under conditions of control (no drug, trace c), 20 μmol/L Ver (trace a), 20 μmol Ver plus 30 nmol/L Tol (trace b, A) or 20 μmol/L Ver plus 4 μmol/L TTX (trace b, D), and 5 mmol/L Ni2+ (trace d) in the presence of 20 μmol/L Ver. (B and E) Ni2+-sensitive INCX obtained by subtracting the data in trace d from the data in traces a, b and c in panel A or panel D. (C and F) Mean current densities of INCX under different conditions. *P<0.05, **P<0.01 vs control. #P<0.05, ##P<0.01 vs Ver.
Effects of Tol on AP
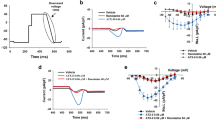
The experiments were divided into four groups. In group 1, 30 nmol/L Tol prolonged APD90 to some extent (n=12, P<0.05 vs control) (Figure 6A, Table 1). In group 2, 200 nmol/L E-4031 (an Ikr specific antagonist) significantly prolonged APD90 (n=12, P<0.05 vs control) and 30 nmol/L Tol plus E-4031 further extended APD90 slightly (n=12, P>0.05 vs E-4031) (Figure 6B, Table 1). In group 3, 20 μmol/L Ver significantly extended APD90 and evoked EAD in 18 of 24 cells (75%). In the presence of Ver, 30 nmol/L Tol reversed APD90 and eliminated EADs induced by Ver from 18/24 to 0/24 cells (Figure 6C, Table 2). In group 4, the myocytes were sequentially treated with no drug (control), 20 μmol/L Ver, and Ver plus 4 μmol/L TTX. TTX also shortened the prolongation of APD90 (n=12, P<0.05 vs Ver) and eliminated EADs induced by Ver from 8/12 to 0/12 (Figure 6D, Table 2). In all groups, Tol had no effect on the resting potential, AP amplitude and Vmax (Tables 1, 2).
Effects on Tol on APs in rabbit ventricular myocytes. (A) The effects of 30 nmol/L Tol on normal AP waveforms. (B) The effects of 30 nmol/L Tol on AP waveforms induced by 200 nmol/L E-4031. The myocytes were sequentially treated with no drug (control), 200 nmol/L E-4031, and 200 nmol/L E-4031 plus 30 nmol/L Tol. (C and D) The effects of 30 nmol/L Tol (C) or 4 μmol/L TTX (D) on AP waveforms induced by 20 μmol/L Ver. The myocytes were sequentially treated with no drug (control), 20 μmol/L Ver, and 20 μmol/L Ver plus 30 nmo l/L Tol (C) or 20 μmol/L Ver plus 4 μmol/L TTX (D).
Discussion
Tol, a competitive, nonselective antimuscarinic compound, is developed for the treatment of an overactive bladder32,38,39. Millions of patients have benefited from Tol treatment40. Furthermore, little has been reported regarding the fatal proarrhythmic effects of Tol in either early clinical tests or follow-up studies32,33,38,41. In recent years, studies have shown that Tol can reduce heart rate variability, while its effect on arrhythmia remains unknown42,43.
In this study, Tol inhibited normal and Ver-augmented INa.L in a concentration-dependent manner, with IC50 values of 32.08 nmol/L and 42.47 nmol/L, respectively (Figures 1, 2). In the presence of atropine, 30 nmol/L Tol also decreased the enlarged INa.L induced by Ver, which demonstrated that its blocking effects on INa.L were not a result of M receptor signaling pathway blockage (Figure 2F). Tol did not modify the steady-activation curve but shifted the steady-inactivation curve of INa.T toward a more positive voltage, which indicated that Tol accelerated the rate of inactivation of sodium channels (Figure 4D).
Tol also inhibited INa.T in a concentration-dependent manner (Figure 4). In contrast with an IC50 of 32.08 nmol/L for INa.L, the IC50 for INa.T was 183.03 μmol/L, which indicated that Tol specifically inhibited INa.L. The ratio of suppressions of INa.L and INa.T (IC50INa.T/IC50INa.L) was 5705, compared with values of 38 and 2.7 for ranolazine and lidocaine, respectively18, which shows that Tol has a high affinity blockade effect on INa.L. Thus, selectively inhibiting INa.L with only negligible effect on INa.T at nmol/L concentration, Tol could have little effect on membrane depolarization, cell excitability and conductibility, thereby preventing arrhythmogenic and other adverse effects.
Under pathological conditions, the increase in INa.L results in a rise of intracellular Na+ and subsequent intracellular Ca2+ overload by increasing reverse INCX. The accumulation of Ca2+ can cause cell injury, electrical activity disorder and ventricular systolic dysfunction, which aggravates myocardial ischemia and hypoxia. The entire process can develop into a vicious circle3,4,13,14. Our previous study indicates that 2 μmol/L TTX (no report regarding its effects on ion channels except INa.L) suppresses the reverse INCX under normal and hypoxic conditions by inhibiting INa.L11. In this study, Tol inhibited the reverse INCX increased by Ver (Figures 5A–5C). Therefore, we speculate that Tol can protect myocytes from injury by preventing abnormal Ca2+ influx caused by the increase in reverse INCX.
Kang et al31 reported that Tol blocked both the HERG channels and L-type Ca2+ channels simultaneously but did not significantly prolong APD, (a maximal 16% extension of APD90). In their study, 30 nmol/L Tol significantly inhibited HERG current but slightly decreased Ca2+ current. According to these results, APD90 should have been prolonged significantly, which would be markedly different from their report of just a 16% extension of APD90. In our present study 30 nmol/L Tol blocked normal and Ver-increased INa.L. In our AP study, 30 nmol/L Tol extended APD90 by 16% under normal conditions, which was consistent with the result reported by Kang et al, and had little effects on the prolongation of APD induced by E-4031 (Figure 6B and Table 1). Based on the above-mentioned results, we speculate that Tol's simultaneous inhibition of IKr and INa.L can explain the fact that 30 nmol/L Tol weakly prolonged the APD in normal ventricular myocytes. Ver significantly extended APD90 and evoked EAD in 18 of 24 cells (75%). In the presence of Ver, 30 nmol/L Tol reversed APD90 and eliminated EADs induced by Ver (Figure 6C and Table 2), which indicates that Tol inhibits arrhythmia induced by Ver. As a multi-ion channel blocker, Tol has complex electrophysiological properties. It is possible that Tol inhibits arrhythmias by inhibiting INa.L, reversing prolongation of APD90 and eliminating EADs induced by Ver.
In conclusion, Tol inhibited normal and Ver-increased INa.L in a concentration-dependent manner and decreased Ver-augmented reverse INCX. In addition, Tol reversed the prolongation of APD and eliminated EADs induced by Ver. These findings point to the potential of Tol as a high affinity INa.L blocker to inhibit arrhythmias induced by increased INa.L with few undesirable adverse effects.
Author contribution
Chao WANG, An-tao LUO, and Ji-hua MA designed the research; Chao WANG, Lei-lei WANG, Chi ZHANG, Zhen-zhen CAO, and Pei-hua ZHANG performed the research; Chao WANG, Lei-lei WANG, Chi ZHANG, Zhen-zhen CAO, Pei-hua ZHANG, Xin-rong FAN, and Ji-hua MA analyzed the data; Chao WANG, Lei-lei WANG, Chi ZHANG, and An-tao LUO wrote the paper.
References
Saint DA . The cardiac persistent sodium current: an appealing therapeutic target? Br J Pharmacol 2008; 153: 1133–42.
Valdivia CR, Chu WW, Pu J, Foell JD, Haworth RA, Wolff MR, et al. Increased late sodium current in myocytes from a canine heart failure model and from failing human heart. J Mol Cell Cardiol 2005; 38: 475–83.
Ju YK, Saint DA, Gage PW . Hypoxia increases persistent sodium current in rat ventricular myocytes. J Physiol 1996; 497: 337–47.
Luo AT, Cao ZZ, Xiang Y, Zhang S, Qian CP, Fu C, et al. Ketamine attenuates the Na+-dependent Ca2+ overload in rabbit ventricular myocytes in vitro by inhibiting late Na+ and L-type Ca2+ currents. Acta Pharmacol Sin 2015; 36: 1327–36.
Wang W, Ma J, Zhang P, Luo A . Redox reaction modulates transient and persistent sodium current during hypoxia in guinea pig ventricular myocytes. Pflugers Arch 2007; 454: 461–75.
Zhou H, Ma JH, Zhang PH, Luo AT . Vitamin C pretreatment attenuates hypoxia-induced disturbance of sodium currents in guinea pig ventricular myocytes. J Membr Biol 2006; 211: 81–7.
Ahern GP, Hsu SF, Klyachko VA, Jackson MB . Induction of persistent sodium current by exogenous and endogenous nitric oxide. J Biol Chem 2000; 275: 28810–5.
Cheng J, Valdivia CR, Vaidyanathan R, Balijepalli RC, Ackerman MJ, Makielski JC . Caveolin-3 suppresses late sodium current by inhibiting nNOS-dependent S-nitrosylation of SCN5A. J Mol Cell Cardiol 2013; 61: 102–10.
Luo A, Ma J, Zhang P, Zhou H, Wang W . Sodium channel gating modes during redox reaction. Cell Physiol Biochem 2007; 19: 9–20.
Ma JH, Luo AT, Zhang PH . Effect of hydrogen peroxide on persistent sodium current in guinea pig ventricular myocytes. Acta Pharmacol Sin 2005; 26: 828–34.
Wang XJ, Wang LL, Fu C, Zhang PH, Wu Y, Ma JH . Ranolazine attenuates the enhanced reverse Na+-Ca2+ exchange current via inhibiting hypoxia-increased late sodium current in ventricular myocytes. J Pharmacol Sci 2014; 124: 365–73.
Zhang S, Ma JH, Zhang PH, Luo AT, Ren ZQ, Kong LH . Sophocarpine attenuates the Na+-dependent Ca2+ overload induced by Anemoniasulcata toxin-increased late sodium current in rabbit ventricular myocytes. J Cardiovasc Pharmacol 2012; 60: 357–66.
Belardinelli L, Shryock JC, Fraser H . Inhibition of the late sodium current as potential cardioprotective principle: effects of the late sodium current inhibitor ranolazine. Heart 2006; 92: iv6–iv14.
Hammarström AK, Gage PW . Hypoxia and persistent sodium current. Eur Biophys J 2002; 31: 323–30.
Levi AJ, Dalton GR, Hancox JC, Mitcheson JS, Issberner J, Bates JA, et al. Role of intracellular sodium overload in the genesis of cardiac arrhythmias. J Cardiovasc Electrophysiol 1997; 8: 700–21.
Pezhouman A, Madahian S, Stepanyan H, Ghukasyan H, Qu Z, Belardinelli L, et al. Selective inhibition of late sodium current suppresses ventricular tachycardia and fibrillation in intact rat hearts. Heart Rhythm 2014; 11: 492–501.
Song Y, Shryock JC, Belardinelli L . An increase of late sodium current induces delayed afterdepolarizations and sustained triggered activity in atrial myocytes. Am J Physiol Heart Circ Physiol 2008; 294: H2031–9.
Hale SL, Shryock JC, Belardinelli L, Sweeney M, Kloner RA . Late sodium current inhibition as a new cardioprotective approach. J Mol Cell Cardiol 2008; 44: 954–67.
Maltsev VA, Undrovinas A . Late sodium current in failing heart: friend or foe? Prog Biophys Mol Biol 2008; 96: 421–51.
Song Y, Shryock JC, Wagner S, Maier LS, Belardinelli L . Blocking late sodium current reduces hydrogen peroxide-induced arrhythmogenic activity and contractile dysfunction. J Pharmacol Exp Ther 2006; 318: 214–22.
Sossalla S, Wagner S, Rasenack EC, Ruff H, Weber SL, Schöndube FA, et al. Ranolazine improves diastolic dysfunction in isolated myocardium from failing human hearts — role of late sodium current and intracellular ion accumulation. J Mol Cell Cardiol 2008; 45: 32–43.
Undrovinas A, Maltsev VA . Late sodium current is a new therapeutic target to improve contractility and rhythm in failing heart. Cardiovasc Hematol Agents Med Chem 2008; 6: 348–59.
Zaza A, Belardinelli L, Shryock JC . Pathophysiology and pharmacology of the cardiac “late sodium current”. Pharmacol Ther 2008; 119: 326–39.
Weeke P, Andersson C, Brendorp B, Torp-Pedersen C . Vernakalant (RSD1235) in the management of atrial fibrillation: a review of pharmacological properties, clinical efficacy and safety. Future Cardiol 2008; 4: 559–67.
Persson F, Carlsson L, Duker G, Jacobson I . Blocking characteristics of hERG, hNav1.5, and hKvLQT1/hminK after administration of the novel anti-arrhythmic compound AZD7009. J Cardiovasc Electrophysiol 2005; 16: 329–41.
Orth PM, Hesketh JC, Mak CK, Yang Y, Lin S, Beatch GN, et al. RSD1235 blocks late INa and suppresses early afterdepolarizations and torsades de pointes induced by class III agents. Cardiovasc Res 2006; 70: 486–96.
Persson F, Andersson B, Duker G, Jacobson I, Carlsson L . Functional effects of the late sodium current inhibition by AZD7009 and lidocaine in rabbit isolated atrial and ventricular tissue and Purkinje fibre. Eur J Pharmacol 2007; 558: 133–43.
Eckhardt LL, Teelin TC, January CT . Is ranolazine an antiarrhythmic drug? Am J Physiol Heart Circ Physiol 2008; 294: H1989–91.
Koltun DO, Parkhill EQ, Elzein E, Kobayashi T, Notte GT, Kalla R, et al. Discovery of triazolopyridinone GS-458967, a late sodium current inhibitor (Late INai) of the cardiac Nav1.5 channel with improved efficacy and potency relative to ranolazine. Bioorg Med Chem Lett 26: 3202–6.
Martin RL, Su Z, Limberis JT, Palmatier JD, Cowart MD, Cox BF, et al. In vitro preclinical cardiac assessment of tolterodine and terodiline: multiple factors predict the clinical experience. J Cardiovasc Pharmacol 2006; 48: 199–206.
Kang J, Chen XL, Wang H, Ji J, Reynolds W, Lim S, et al. Cardiac ion channel effects of tolterodine. J Pharmacol Exp Ther 2004; 308: 935–40.
Layton D, Pearce GL, Shakir SA . Safety profile of tolterodine as used in general practice in England: results of prescription-event monitoring. Drug Saf 2001; 24: 703–13.
Millard R, Tuttle J, Moore K, Susset J, Clarke B, Dwyer P, et al. Clinical efficacy and safety of tolterodine compared to placebo in detrusor overactivity. J Urol 1999; 161: 1551–5.
Chevalier M, Amuzescu B, Gawali V, Todt H, Knott T, Scheel O, et al. Late cardiac sodium current can be assessed using automated patch-clamp. F1000Res 2014; 3: 245.
Horváth B, Hegyi B, Kistamás K, Váczi K, Bányász T, Magyar J, et al. Cytosolic calcium changes affect the incidence of early afterdepolarizations in canine ventricular myocytes. Can J Physiol Pharmacol 2015; 93: 527–34.
Kong LH, Ma JH, Zhang PH, Luo AT, Zhang S, Ren ZQ, et al. Involvement of veratridine-induced increase of reverse Na+/Ca2+ exchange current in intracellular Ca2+ overload and extension of action potential duration in rabbit ventricular myocytes. Acta Physiol Sin 2012; 64: 433–43.
Maltsev VA, Sabbah HN, Higgins RS, Silverman N, Lesch M, Undrovinas AI . Novel, ultraslow inactivating sodium current in human ventricular cardiomyocytes. Circulation 1998; 98: 2545–52.
Malone-Lee JG, Walsh JB, Maugourd MF . Tolterodine: a safe and effective treatment for older patients with overactive bladder. J Am Geriatr Soc 2001; 49: 700–5.
Rovner ES . Tolterodine for the treatment of overactive bladder: a review. Expert Opin Pharmacother 2005; 6: 653–66.
Garely AL, Burrows L . Benefit-risk assessment of tolterodine in the treatment of overactive bladder in adults. Drug Saf 2004; 27: 1043–57.
Larsson G, Hallén B, Nilvebrant L . Tolterodine in the treatment of overactive bladder: analysis of the pooled phase II efficacy and safety data. Urology 1999; 53: 990–8.
Olshansky B, Ebinger U, Brum J, Egermark M, Viegas A, Rekeda L . Differential pharmacological effects of antimuscarinic drugs on heart rate: a randomized, placebo-controlled, double-blind, crossover study with tolterodine and darifenacin in healthy participants > or =50 years. J Cardiovasc Pharmacol Ther 2008; 13: 241–51.
Hsiao SM, Chang TC, Wu WY, Chen CH, Yu HJ, Lin HH . Comparisons of urodynamic effects, therapeutic efficacy and safety of solifenacin versus tolterodine for female overactive bladder syndrome. J Obstet Gynaecol Res 2011; 37: 1084–91.
Acknowledgements
This work was supported by the National Natural Science Foundation of China (No 81072637). We also thank Ms Na LUO of the University of Hong Kong for her editorial assistance with this paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, C., Wang, Ll., Zhang, C. et al. Tolterodine reduces veratridine-augmented late INa, reverse-INCX and early afterdepolarizations in isolated rabbit ventricular myocytes. Acta Pharmacol Sin 37, 1432–1441 (2016). https://doi.org/10.1038/aps.2016.76
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2016.76
Keywords
This article is cited by
-
Barbaloin inhibits ventricular arrhythmias in rabbits by modulating voltage-gated ion channels
Acta Pharmacologica Sinica (2018)
-
Modification of distinct ion channels differentially modulates Ca2+ dynamics in primary cultured rat ventricular cardiomyocytes
Scientific Reports (2017)