Abstract
Aim:
Leflunomide is an immunosuppressive agent marketed as a disease-modifying antirheumatic drug. But it causes severe side effects, including fatal hepatitis and liver failure. In this study we investigated the contributions of hepatic metabolism and transport of leflunomide and its major metabolite teriflunomide to leflunomide induced hepatotoxicity in vitro and in vivo.
Methods:
The metabolism and toxicity of leflunomide and teriflunomide were evaluated in primary rat hepatocytes in vitro. Hepatic cytochrome P450 reductase null (HRN) mice were used to examine the PK profiling and hepatotoxicity of leflunomide in vivo. The expression and function of sodium/bile acid cotransporter (NTCP) were assessed in rat and human hepatocytes and NTCP-transfected HEK293 cells. After Male Sprague-Dawley (SD) rats were administered teriflunomide (1,6, 12 mg·kg−1·d−1, ig) for 4 weeks, their blood samples were analyzed.
Results:
A nonspecific CYPs inhibitor aminobenzotriazole (ABT, 1 mmol/L) decreased the IC50 value of leflunomide in rat hepatocytes from 409 to 216 μmol/L, whereas another nonspecific CYPs inhibitor proadifen (SKF, 30 μmol/L) increased the cellular accumulation of leflunomide to 3.68-fold at 4 h. After oral dosing (15 mg/kg), the plasma exposure (AUC0-t) of leflunomide increased to 3-fold in HRN mice compared with wild type mice. Administration of leflunomide (25 mg·kg−1·d−1) for 7 d significantly increased serum ALT and AST levels in HRN mice; when the dose was increased to 50 mg·kg−1·d−1, all HRN mice died on d 6. Teriflunomide significantly decreased the expression of NTCP in human hepatocytes, as well as the function of NTCP in rat hepatocytes and NTCP-transfected HEK293 cells. Four-week administration of teriflunomide significantly increased serum total bilirubin and direct bilirubin levels in female rats, but not in male rats.
Conclusion:
Hepatic CYPs play a critical role in detoxification process of leflunomide, whereas the major metabolite teriflunomide suppresses the expression and function of NTCP, leading to potential cholestasis.
Similar content being viewed by others
Introduction
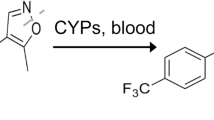
Leflunomide (LEF) is an immunosuppressive agent that mainly inhibits dihydroorotate dehydrogenase, the rate-limiting enzyme in the biosynthesis of pyrimidines. LEF was marketed as a disease-modifying antirheumatic drug in 19981. However, many reports were released to describe its side effects during its clinical application, which included fatal hepatitis and liver failure. Due to these clinical cases of hepatotoxicity, the Food and Drug Administration (FDA) labeled LEF with a black box warning in 2011 (http://www.fda.gov/Safety/MedWatch/SafetyInformation/ucm228392.htm). Several cytochrome P450 enzymes (CYPs), such as CYP1A2, CYP2C19 and CYP3A4, are involved in the biotransformation of LEF into its major metabolite teriflunomide (TER)2. One clinical report showed that a patient co-administered with LEF and the CYP3A inhibitor itraconazole developed fatal hepatitis3. However, the contribution of CYPs to LEF-induced liver toxicity has not yet been elucidated completely, and the limited available in vitro results are controversial. For example, it was suggested that the metabolites of LEF might be more toxic to the liver, as LEF-induced cytotoxicity was attenuated by the nonspecific CYPs inhibitor ABT in immortalized human hepatocytes4. In contrast, another study indicated that LEF cytotoxicity was enhanced by several CYPs inhibitors in primary rat hepatocytes5. As far as we know, there is no direct in vivo studies investigating the role of CYPs in LEF induced hepatotoxicity. Besides, although TER treatment significantly increased aminotransferase level, which leads to discontinue therapy in clinical studies6,7,8, there is no investigation about the liver toxicity of the metabolite of LEF, TER. Therefore, it's worthwhile to investigate the mechanism of TER induced liver toxicity and its contribution to the hepatotoxicity of LEF. At the same time, both LEF and TER were reported to be high affinity substrates of efflux transporter breast cancer resistance protein (BCRP)9. Since there are multiple anti-rheumatic drugs are reported to be the substrates of BCRP10,11,12, and the change of BCRP function may lead to toxicity13, the potential drug-drug interaction risk mediated by BCRP or other transporters should be investigated. Therefore, we want to explore whether transporters are involved in the liver toxicity of LEF and TER.
In this study, we investigated the role of hepatic metabolism and transport in LEF-induced hepatotoxicity. We checked whether LEF toxicity was modulated by CYPs using nonspecific CYPs inhibitors in primary hepatocytes. Then, hepatic cytochrome P450 reductase null (HRN) mice were employed to verify the contribution of CYPs to the plasma concentration of LEF and its liver toxicity. Given that neither LEF nor TER significantly changed the mRNA expression of BCRP in either rat or human hepatocytes; and TER could significantly reduce sodium/bile acid cotransporter (NTCP) expression in human hepatocytes. Rat hepatocytes and NTCP-transfected HEK293 cells were used to investigate the contribution of selected transporters to the hepatotoxicity of LEF and TER. Then, SD rats were orally administered with TER for 4 weeks to further certify in vitro findings about potential mechanism of TER toxicity.
Materials and methods
Chemicals
LEF (99.5%; batch No 130603) and TER (>99.9%; batch No 121123) were kindly provided by Cinkate Pharmaceutical Intermediates Co, Ltd (Shanghai, China). For in vitro assays, LEF and TER were dissolved in Dimethyl sulfoxide (DMSO). All reagents used for cell culture were purchased from GIBCO unless otherwise specified. Dimethyl sulfoxide (DMSO), proadifen (SKF), aminobenzotriazole (ABT), collagenase (type IV), phenacetin (Phe), tetramethylrhodamine ethyl ester (TMRE), troglitazone (Tro) and 3-methylcholanthrene (3-MC) were purchased from Sigma-Aldrich (St Louis, MO, USA). BD MatrigelTM Basement Membrane Matrix and rat tail collagen (type I) were obtained from BD Biosciences (Palo Alto, CA, USA). 3-(4, 5-Dimethylthiazollthiazol-2-yl)-2, 5-diphenyltetrazolium bromide (MTT) was purchased from Sangon Biotech (Shanghai) Co, Ltd. BSA protein assay kit was obtained from Pierce Chemical (Rockford, IL, USA).
Animals
Male Sprague-Dawley (SD) rats (8 weeks old) and male C57 BL6 mice (6 weeks old) housed in the SPF class experimental animal room were purchased from Shanghai SLAC Laboratory Animal Co, Ltd (Shanghai, China). HRN mice, without metabolic activity, were generated as previously reported14. Male SD rats, male wild-type (WT) and HRN mice (7 weeks old) were housed under standard laboratory conditions (temperature 25±1 °C, humidity 50%±10% and 12 h light/12 h dark cycle) in the institutional animal facility with free access to food and water.
All animal experiments were conducted in compliance with the Guidance for Ethical Treatment of Laboratory Animals, and the experimental protocols were approved by the Institutional Animal Care and Use Committee at the Shanghai Institute of Materia Medica (Shanghai, China). For all animal experiments, LEF or TER was suspended in a 0.5% carboxymethylcellulose sodium solution (CMC-Na+) and administered by intragastric gavage in a volume of 10 mL/kg body weight.
Experimental design
Initially, in in vitro assays, we used rat and human hepatocytes to investigate the interaction between CYPs and LEF, TER. To verify the observed phenomena in in vitro assays, we investigated the contribution of CYPs to LEF-induced hepatotoxicity in HRN mice, and obtained consistent results with these different models, suggesting that the species differences were minimal in this context. Then, we observed TER significantly decreased NTCP expression in human hepatocytes. Therefore, we used rat hepatocytes and NTCP-transfected HEK293 cells to study the effect of TER on NTCP function and got consistent results. Eventually, we conducted in vivo assay in SD rats to confirm the results of in vitro assays. The details of this study design is shown in Figure 1.
Flow chart of the study design. LEF, leflunomide; TER, teriflunomide.
Isolation and culture of primary rat and human hepatocytes
Primary rat hepatocytes were obtained from SD rats using a two-step collagenase digestion method with some modifications15,16. Cell viability, determined via trypan blue exclusion, was greater than 85%. Viable hepatocytes were plated in culture plates coated with type I rat tail collagen and incubated at 37 °C under 5% CO2. The medium was changed after attachment. For the biliary excretion assay, after 24 h, cells were overlaid with 0.25 mg/mL Matrigel in ice-cold medium without fetal bovine serum (FBS) to form a sandwich configuration during the subsequent culture period, as previously described17. Cryopreserved primary human hepatocytes were purchased from GIBCO. After attachment for 6 h, the plating medium was changed to culture medium without FBS for the subsequent culture period.
Quantitative determination of gene expression via RT-PCR
Primary rat and human hepatocytes were treated with 10 μmol/L LEF or TER for 48 h. Total RNA was isolated with the TRIzol reagent (Life Technologies, CA, USA), and cDNA synthesis was performed using the PrimeScript RT Reagent Kit (Takara, Shiga, Japan). Quantitative analysis of the gene expression of several CYPs and transporters was conducted via real-time PCR using a Qiagen Rotor Gene Q instrument (Qiagen, Germany). β-Actin was used for internal normalization. All the primers (Table 1) were synthesized at Sangon Biotech (Shanghai) Co, Ltd.
Determination of CYP1A2 enzyme activity
The activity of the CYP1A2 enzyme was measured using its specific substrate phenacetin (Phe 2 μmol/L) as a probe18. After human hepatocytes were treated with LEF (10 μmol/L) and TER (10 μmol/L) for 48 h, 2 μmol/L Phe dissolved in medium was added to the cells, followed by an additional 2 h incubation after the hepatocytes were rinsed with PBS. The concentrations of Phe in medium at 0, 0.5, 1, and 2 h were analyzed via LC–MS/MS (LCMS-8030; Shimadzu, Kyoto, Japan). 3-MC (2 μmol/L) was used as a positive control. Enzymatic activity was normalized according to the protein quantification results.
Cell viability assays
Primary rat hepatocytes were seeded into 96-well plates. The hepatocytes were then treated with various concentrations of LEF and TER (10-1000 μmol/L). Then, the assay was conducted following the instruction as previously described19. For the inhibition assay, hepatocytes were pre-incubated with the nonspecific CYPs inhibitor ABT (1 mmol/L) for 1 h.
Metabolism of LEF and TER in rat hepatocytes
Freshly isolated rat hepatocytes were suspended in 12-well plates. Medium containing LEF or TER (10 μmol/L) was added to the hepatocytes. Subsequently, 100 μL samples were collected at 0, 1, 2 and 4 h respectively and added to 300 μL of ice cold methanol to terminate the reaction. The concentration of LEF and TER in primary rat hepatocytes and medium were determined via liquid chromatography–mass spectrometry tandem mass spectrometry (LC–MS/MS) (LCMS-8030; Shimadzu, Kyoto, Japan) and normalized according to the total protein content. For the inhibition study, primary rat hepatocytes were treated with 30 μmol/L SKF for 30 min before incubated with LEF or TER.
Determination of CLint, scaled of LEF in primary hepatocytes
The scaled intrinsic clearance (CLint, scaled) of LEF was estimated based on the rate of LEF disappearance from the incubation medium, as described previously20. The elimination rate constant, k, for LEF was determined by plotting the natural log of the concentration of LEF according to time in minutes. The elimination rate constant was subsequently used to calculate the half-life (T1/2) of LEF according to T1/2=0.693/k. Then, CLint, in vitro can be derived as follows: CLint, in vitro=(0.693/T1/2)*(V/M), where V/M is equal to the incubation volume per 106 cells. CLint, in vitro was scaled to in vivo CLint, scaled using a hepatocellularity of 120×106 cells/g liver and a human liver weight of 20 g/kg body weight.
Pharmacokinetic and safety study of LEF in WT and HRN mice
In all animal experiments, WT and HRN mice were fasted for 12-14 h prior to the experiment.
Following oral administration of LEF (15 mg/kg), 40 μL of blood (heparin sodium as anti-coagulant) was drawn from the caudal vena cava at designated time points. Plasma was obtained via centrifugation at 4 °C and immediately added to 120 μL of ice-cold acetonitrile containing an internal standard. The plasma concentration of LEF and TER were determined via LC-MS/MS (LCMS-8030; Shimadzu, Kyoto, Japan).
For the survival and toxicity experiments, mice were orally administered with LEF at different doses (0, 25, or 50 mg/kg) once a day, and the number of surviving mice was recorded within 7 d after the treatment. Blood samples were obtained before dissection, and the level of AST and ALT in the serum were analyzed. The animals in the control group only received the vehicle (CMC-Na+).
Accumulation of d8-TCA in freshly isolated primary rat hepatocytes and NTCP-transfected HEK293 cells
Rat hepatocytes and NTCP-transfected HEK293 cells, plated for 4 or 24 h respectively, were washed twice with 300 μL of warm HBSS and then incubated with HBSS for 15 min. Next, 300 μL of d8-TCA (5 μmol/L) dissolved in warm HBSS was added, followed by incubation for an additional 15 min after removing the medium. Then, the solution was removed, and the reaction was terminated by washing with ice cold PBS for three times. The concentration of d8-TCA in the cells was determined via LC–MS/MS (LCMS-8030; Shimadzu, Kyoto, Japan). For the inhibition experiment, cells were incubated with d8-TCA (5 μmol/L) and LEF or TER (10-100 μmol/L) simultaneously. Troglitazone (Tro 20 μmol/L) was used as the positive control. The concentration of d8-TCA in cells was normalized according to total protein content.
Effect of TER on NTCP function in rats
Rats were fasted for 12-14 h prior to the experiment. Then, rats divided into four groups through random allocation were orally administered TER once a day, at multiple doses of 0, 6, and 12 mg/kg. Four weeks later, blood samples were obtained, and the serum level of total bilirubin (TBILI) and direct bilirubin (DBILI) were analyzed. The animals in the control group received only the vehicle.
Blood biochemistry
Serum of rat and mice blood samples were obtained for biochemistry analysis. Alanine aminotransferase (ALT), aspartate aminotransferase (AST), TBILI and DBILI were determined using an Automatic Clinical Analyzer (7080, HITACHI Ltd, Tokyo, Japan).
Statistical analysis
Data are expressed as the mean±standard deviation (SD) unless otherwise stated. Differences between two groups were analyzed using Student's t-test. A one-way ANOVA were used to test statistical significance among groups using GraphPad Prism 5.03. Values of P<0.05 were considered statistically significant.
Results
Effects of LEF and TER on CYPs expression in primary hepatocytes
Following treatment with LEF and TER (10 μmol/L), CYP1A1/2 and CYP7A1 mRNA level were significantly increased by LEF in primary rat hepatocytes (Figure 2A). TER only significantly increased CYP1A2 expression about 6-fold. In primary human hepatocytes, LEF only significantly induced CYP1A1/2 expression, while TER induced both CYP1A2 and CYP7A1 expression (Figure 2B). However, we found that although both LEF and TER significantly increased CYP1A2 mRNA levels, only LEF significantly increased CYP1A1/2 function in human hepatocytes (Figure 2C).
Effect of LEF and TER on the gene expression and function of CYPs. Rat (A) and human (B and C) hepatocytes were treated with LEF and TER (10 μmol/L). Gene expression was measured and shown as the fold induction (A and B). The function of CYP1A2 was measured using the specific substrate phenacetin (Phe 2 μmol/L) as a probe (C). 3-MC (2 μmol/L) was employed as the positive control. The data are presented as the mean±SD (n=3). bP<0.05, cP<0.01 compared with the control.
Inhibition of hepatic CYPs reduced LEF clearance and increased the toxicity of LEF in rat hepatocytes
ABT (1 mmol/L) significantly increased the toxic effect of LEF in primary rat hepatocytes, with reduction in the IC50 value from 409 μmol/L to 216 μmol/L (Figure 3A) being observed. On the contrary, ABT did not show any effect on the cytotoxicity of TER (Figure 3B). Simultaneously, SKF (30 μmol/L) decreased the hepatic intrinsic clearance of LEF, but not TER, in primary rat hepatocytes: the CLint, scaled of LEF decreased from 136 to 73.9 mL·min−1·kg−1 after SKF treatment. And after 4 h incubation, the accumulation of LEF in primary rat hepatocytes increased 3.68-fold after SKF treatment (Figure 3C and 3D). Consistently, LEF decreased the mitochondrial membrane potential (MMP) of primary rat hepatocytes more apparently than TER (supplementary Figure S1).
Effect of the nonspecific CYPs inhibitors ABT (1 mmol/L) and SKF (30 μmol/L) on the cytotoxicity and metabolism of LEF and TER. Cell viability following ABT treatment was determined via the MTT assay (A and B). The concentrations of LEF and TER in rat hepatocytes following SKF treatment were determined via LC–MS/MS (C and D). Data are presented as the mean±SD (n=3 and 6). bP<0.05, cP<0.01 (LEF+SKF treatment vs LEF alone).
Pharmacokinetic profiles of LEF in WT and HRN mice
The plasma concentration of LEF increased in HRN mice compared with WT mice (Figure 4A). The area under the time-concentration curve (AUC0-t) for LEF in HRN mice was 483±470 ng·mL−1·h, compared with 158±110 ng·mL−1·h in WT mice, while the generation of TER (AUC0-t) decreased compared with WT mice (73.9±39.8 μg·mL−1·h in HRN mice vs 380±296 μg·mL−1·h in WT mice) (Figure 4A and 4B). However, no significant difference between HRN mice and WT mice was observed because of great individual difference.
Plasma concentrations of LEF and TER in WT and HRN mice. WT and HRN mice were orally administered with 15 mg/kg LEF. Then, blood samples were obtained, and the concentrations of LEF (A) and TER (B) in plasma were determined. Data are presented as the mean±SD (n=5).
Toxicity evaluation of LEF in WT and HRN mice following continuous oral administration
In WT mice, no test article related death was observed in the 50 mg/kg LEF group (two animals died by accidents in the vehicle control group) (Figure 5A). At 25 mg/kg LEF, there were two HRN mice exhibited moribund signs on the day of dissection. The level of AST and ALT in the serum of HRN mice were significantly increased compared with the control group, whereas these values were not increased in WT mice (Figure 5C). When the dose increased to 50 mg/kg LEF, death of the HRN mice was observed beginning on the 4th d after oral administration, and all of the animals had died 5 d later (Figure 5B).
Comparison of LEF-induced hepatotoxicity in WT and HRN mice. After the administration of multiple doses of LEF (05 and 50 mg/kg) for 7 d, the survival rates of WT (A) and HRN (B) mice were recorded daily. (C) The serum levels of AST and ALT were determined before dissection on the 7th d in the 25 mg/kg LEF treatment and control groups. Data are presented as the mean±SD (n=6). bP<0.05 (LEF treatment vs control in HRN mice).
Effect of LEF and TER on the expression and function of NTCP
Neither LEF nor TER significantly altered the expression of the selected transporters, ie, P-glycoprotein (P-gp), BCRP, bile salt export pump (BSEP) and NTCP in primary rat hepatocytes (Figure 6A). In primary human hepatocytes, neither LEF nor TER had an effect on the expression of BSEP and BCRP, with the exception of a significant reduction in NTCP expression (Figure 6B). However, it was found that only TER, but not LEF, significantly reduced the uptake of d8-TCA in primary rat hepatocytes and NTCP-transfected HEK293 cells (Figure 6C and 6D). In addition, LEF and TER had no effect on the biliary excretion index (BEI) value of d8-TCA in sandwich-cultured rat hepatocytes (SCRHs) (Supplementary Figure S2).
Effect of LEF and TER on the gene expression and function of NTCP. Rat (A) and human (B) hepatocytes were treated with LEF and TER. Gene expression was measured and presented as the fold induction. Rat hepatocytes (C) and NTCP-transfected HEK293 cells (D) were co-treated with d8-TCA and LEF or TER, after which the accumulation of d8-TCA in the cells was measured. Troglitazone (Tro-20 μmol/L) was used as the positive control. Data are presented as the mean±SD (n=3). cP<0.01 compared with the control.
Consistently, it was found that TER long term treatment significantly increased the level of TBILI and DBILI in the serum of female rats (Table 2).
Discussion
Several studies have demonstrated that LEF is a ligand of the Aryl Hydrocarbon Receptor (AhR)21,22,23, which regulates the expression of CYP1A1/2. Consistently, we determined that LEF significantly induced CYP1A1/2 expression in both primary rat and human hepatocytes (Figure 2). CYP1A1/2 could also be induced by TER in human hepatocytes to a less extent. However, it seems the CYP inhibition instead of CYP induction plays critical roles in the toxicity process of LEF. In this study, it was found that nonspecific CYPs inhibitors SKF and ABT could significantly increase LEF accumulation and cytotoxicity in primary rat hepatocytes (Figure 3). Shi et al claimed that CYPs inhibitors could enhance the liver toxicity of both LEF and TER in primary rat hepatocytes5; however, our data revealed that CYPs only directly contributed to LEF-related, rather than TER-related, detoxification in primary rat hepatocytes. In fact, the mitochondrial membrane potential of primary rat hepatocytes did show more sensitive to LEF than TER (supplementary Figure S1).
Many reports demonstrated that the polymorphism of several CYPs, such as CYP1A2 and CYP2C19, could affect the liver toxicity of LEF in patients with rheumatoid arthritis24,25,26, which could be indirect evidences that CYPs play a critical role in the detoxification of LEF in the body. Our studies with HRN mice are the first direct in vivo evidences that hepatic CYPs are involved in the clearance and toxicity of LEF. The plasma concentration and AUC0-t value of LEF were found to be much higher in HRN mice than in WT mice following single dose of LEF (15 mg/kg), and these mice also showed lower TER exposure in their plasma (Figure 4). Unexpectedly, one of the HRN mice died 10 h after LEF was administered, which may be attributed to the broad variability of LEF pharmacokinetic parameters, as reported previously27. This variability may also explain the great variation in the AUC0-t value of LEF and TER observed in this study. These results suggested that the plasma concentration of LEF may increase when CYPs were knocked out, which could lead to enhanced liver toxicity. In fact, after continuous dosing, at the 25 mg/kg LEF, serum AST and ALT were significantly increased only in the HRN mice (Figure 5C). And the survival rate of HRN mice was significantly lower than that of WT mice when LEF dosage increased to 50 mg/kg for 7 d.
Since LEF and TER are both high affinity substrates of BCRP9, their impacts on liver transporters expression were also explored. It was found they had no effects on the mRNA expression of the selected efflux transporters (BCRP, BSEP), with the exception of the down-regulation of NTCP in human hepatocytes after 48 h of treatment (Figure 6B). Primary rat hepatocytes and NTCP-transfected HEK293 cells were used to further investigate the influences of LEF and TER on the function of NTCP. It was found that TER, but not LEF, could significantly reduce the accumulation of d8-TCA in primary rat hepatocytes, and it inhibited d8-TCA accumulation in NTCP-transfected HEK293 cells in a dose-dependent manner (Figure 6C and 6D). Neither LEF nor TER could directly inhibit the function of BSEP (Supplementary Figure S2). Furthermore, only TER significantly induced the expression of CYP7A1, a rate-limiting enzyme in the biosynthesis of bile acid, by approximately 6-fold in human hepatocytes (Figure 2B). Many drugs disrupt homeostatic mechanisms by directly inhibiting bile acid transporters, such as NTCP or BSEP, leading to bile acid-induced hepatotoxicity28,29,30. Our results implied TER may have similar impacts on the homeostasis of bile acid.
Vrenken et al (2008) reported that TER protects rat hepatocytes from bile acid-induced apoptosis31. Our data may provide an alternative explanation for this observation: the protective role of TER may arise from its inhibition of NTCP function, which leads to less bile acid accumulation in hepatocytes and less apoptosis. However, from another perspective, down-regulation of NTCP and disturbance of bile acid circulation may lead to liver toxicity over the long term32,33,34. In fact, the elimination half-life of TER is approximately 2 weeks, which is thought to result from a combination of extremely low hepatic clearance and enterohepatic recycling27,35. Therefore, the toxicological effect of TER on NTCP expression and function may be sustained over long periods of time. In fact, the level of TBILI and DBILI in female rat serum increased significantly after four weeks treatment of TER (12 mg/kg) (Table 2). This finding implied that TER may have impact on bile acid circulation, which may lead to cholestasis and bile duct injury36. However, since bile acid is the direct biomarker of cholestasis37, bile acid levels in serum will be determined in the future to further verify this hypothesis. In addition, this phenomenon was not observed in male animals, which may be attributed to sex-specific differences in the tissue distribution of TER27.
In summary, CYPs are critical to the detoxification process of LEF-induced liver toxicity. Inactivate hepatic CYPs significantly increase the concentration of LEF in primary hepatocytes and HRN mice, enhancing the hepatotoxicity induced by LEF. Transporters, rather than CYPs, play a unique role in the liver toxicity induced by TER, the major metabolite of LEF. TER significantly decreases the expression and function of NTCP, which may disturb bile acid circulation and cause potential bile acid-related liver issues.
Author contribution
Lei-lei MA, Yang LUAN, Guo-yu PAN participated in research design; Lei-lei MA, Jing WANG, Zhi-tao WU, Le WANG, Chen CHEN, Xuan NI, Yun-fei LIN, Yi-yi CAO conducted experiments; Lei-lei MA, Zhi-tao WU, Xue-feng ZHANG performed data analysis; Lei-lei MA, Yang LUAN, Guo-yu PAN wrote the manuscript.
Abbreviations
ABT, Aminobenzotriazole; ALT, alanine aminotransferase; AST, aspartate aminotransferase; BSEP, bile salt export pump; BEI, biliary excretion index; BCRP, breast cancer resistance protein; CMC-Na+, carboxymethylcellulose sodium; CYPs, cytochrome P450 enzymes; DBILI, direct bilirubin; DDI, drug-drug interaction; HRN, hepatic cytochrome P450 reductase null; LEF, leflunomide; 3-MC, 3-methylcholanthrene; P-gp, P-glycoprotein; Phe, phenacetin; SKF, proadifen; SCRHs, sandwich-cultured rat hepatocytes; CLint, scaled, scaled intrinsic clearance; NTCP, sodium/bile acid cotransporter; TER, teriflunomide; TMRE, tetramethylrhodamine ethyl ester; TBILI, total bilirubin; Tro, troglitazone.
References
Alcorn N, Saunders S, Madhok R . Benefit-risk assessment of leflunomide: an appraisal of leflunomide in rheumatoid arthritis 10 years after licensing. Drug Saf 2009; 32: 1123–34.
Kalgutkar AS, Nguyen HT, Vaz AD, Doan A, Dalvie DK, McLeod DG, et al. In vitro metabolism studies on the isoxazole ring scission in the anti-inflammatory agent lefluonomide to its active alpha-cyanoenol metabolite A771726: mechanistic similarities with the cytochrome P450-catalyzed dehydration of aldoximes. Drug Metab Dispos 2003; 31: 1240–50.
Legras A, Bergemer-Fouquet AM, Jonville-Bera AP . Fatal hepatitis with leflunomide and itraconazole. Am J Med 2002; 113: 352–3.
Seah QM, New LS, Chan EC, Boelsterli UA . Oxidative bioactivation and toxicity of leflunomide in immortalized human hepatocytes and kinetics of the non-enzymatic conversion to its major metabolite, A77 1726. Drug Metab Lett 2008; 2: 153–7.
Shi Q, Yang X, Greenhaw J, Salminen WF . Hepatic cytochrome P450s attenuate the cytotoxicity induced by leflunomide and its active metabolite A77 1726 in primary cultured rat hepatocytes. Toxicol Sci 2011; 122: 579–86.
Confavreux C, Li DK, Freedman MS, Truffinet P, Benzerdjeb H, Wang D, et al. Long-term follow-up of a phase 2 study of oral teriflunomide in relapsing multiple sclerosis: safety and efficacy results up to 8.5 years. Mult Scler 2012; 18: 1278–89.
Miller AE, Wolinsky JS, Kappos L, Comi G, Freedman MS, Olsson TP, et al. Oral teriflunomide for patients with a first clinical episode suggestive of multiple sclerosis (TOPIC): a randomised, double-blind, placebo-controlled, phase 3 trial. Lancet Neurol 2014; 13: 977–86.
Tallantyre E, Evangelou N, Constantinescu CS . Spotlight on teriflunomide. Int MS J 2008; 15: 62–8.
Kis E, Nagy T, Jani M, Molnár E, Jánossy J, Ujhellyi O, et al. Leflunomide and its metabolite A771726 are high affinity substrates of BCRP: implications for drug resistance. Ann Rheum Dis 2009; 68: 1201–7.
Jani M, Szabó P, Kis E, Molnár E, Glavinas H, Krajcsi P . Kinetic characterization of sulfasalazine transport by human ATP-binding cassette G2. Biol Pharm Bull 2009; 32: 497–9.
Chen ZS, Robey RW, Belinsky MG, Shchaveleva I, Ren XQ, Sugimoto Y, et al. Transport of methotrexate, methotrexate polyglutamates, and 17beta-estradiol 17-(beta-D-glucuronide) by ABCG2: effects of acquired mutations at R482 on methotrexate transport. Cancer Res 2003; 63: 4048–54.
Tiwari AK, Sodani K, Wang SR, Kuang YH, Ashby CR, Chen X, et al. Nilotinib (AMN107, Tasigna) reverses multidrug resistance by inhibiting the activity of the ABCB1/Pgp and ABCG2/BCRP/MXR transporters. Biochem Pharmacol 2009; 78: 153–61.
Loue C, Garnier N, Bertrand Y, Bleyzac N . High methotrexate exposure and toxicity in children with t(9;22) positive acute lymphoblastic leukaemia treated with imatinib. J Clin Pharm Ther 2015. doi:10.1111/jcpt.12298.
Gu J, Weng Y, Zhang QY, Cui H, Behr M, Wu L, et al. Liver-specific deletion of the NADPH-cytochrome P450 reductase gene: impact on plasma cholesterol homeostasis and the function and regulation of microsomal cytochrome P450 and heme oxygenase. J Biol Chem 2003; 278: 25895–901.
Liu X, LeCluyse EL, Brouwer KR, Lightfoot RM, Lee JI, Brouwer KL . Use of Ca2+ modulation to evaluate biliary excretion in sandwich-cultured rat hepatocytes. J Pharmacol Exp Ther 1999; 289: 1592–9.
Wu ZT, Qi XM, Sheng JJ, Ma LL, Ni X, Ren J, et al. Timosaponin A3 induces hepatotoxicity in rats through inducing oxidative stress and down-regulating bile acid transporters. Acta Pharmacol Sin 2014; 35: 1188–98.
Swift B, Pfeifer ND, Brouwer KL . Sandwich-cultured hepatocytes: an in vitro model to evaluate hepatobiliary transporter-based drug interactions and hepatotoxicity. Drug Metab Rev 2010; 42: 446–71.
Kanazawa H, Okada A, Igarashi E, Higaki M, Miyabe T, Sano T, et al. Determination of midazolam and its metabolite as a probe for cytochrome P450 3A4 phenotype by liquid chromatography-mass spectrometry. J Chromatogr A 2004; 1031: 213–8.
Chung JY, Kim JY, Kim WR, Lee SG, Kim YJ, Park JE, et al. Abundance of aryl hydrocarbon receptor potentiates benzo[a]pyrene-induced apoptosis in Hepa1c1c7 cells via CYP1A1 activation. Toxicology 2007; 235: 62–72.
McGinnity DF, Soars MG, Urbanowicz RA, Riley RJ . Evaluation of fresh and cryopreserved hepatocytes as in vitro drug metabolism tools for the prediction of metabolic clearance. Drug Metab Dispos 2004; 32: 1247–53.
Hu W, Sorrentino C, Denison MS, Kolaja K, Fielden MR . Induction of cyp1a1 is a nonspecific biomarker of aryl hydrocarbon receptor activation: results of large scale screening of pharmaceuticals and toxicants in vivo and in vitro. Mol Pharmacol 2007; 71: 1475–86.
O'Donnell EF, Kopparapu PR, Koch DC, Jang HS, Phillips JL, Tanguay RL, et al. The aryl hydrocarbon receptor mediates leflunomide-induced growth inhibition of melanoma cells. PLoS One 2012; 7: e40926.
O'Donnell EF, Saili KS, Koch DC, Kopparapu PR, Farrer D, Bisson WH, et al. The anti-inflammatory drug leflunomide is an agonist of the aryl hydrocarbon receptor. PLoS One 2010; 5. pii: e13128.
Bohanec Grabar P, Grabnar I, Rozman B, Logar D, Tomsic M, Suput D, et al. Investigation of the influence of CYP1A2 and CYP2C19 genetic polymorphism on 2-cyano-3-hydroxy-N-[4-(trifluoromethyl)phenyl]-2-butenamide (A77 1726) pharmacokinetics in leflunomide-treated patients with rheumatoid arthritis. Drug Metab Dispos 2009; 37: 2061–8.
Bohanec Grabar P, Rozman B, Tomsic M, Suput D, Logar D, Dolzan V . Genetic polymorphism of CYP1A2 and the toxicity of leflunomide treatment in rheumatoid arthritis patients. Eur J Clin Pharmacol 2008; 64: 871–6.
Wiese MD, Schnabl M, O'Doherty C, Spargo LD, Sorich MJ, Cleland LG, et al. Polymorphisms in cytochrome P450 2C19 enzyme and cessation of leflunomide in patients with rheumatoid arthritis. Arthritis Res Ther 2012; 14: R163.
Rozman B . Clinical pharmacokinetics of leflunomide. Clin Pharmacokinet 2002; 41: 421–30.
Padda MS, Sanchez M, Akhtar AJ, Boyer JL . Drug-induced cholestasis. Hepatology 2011; 53: 1377–87.
Dawson S, Stahl S, Paul N, Barber J, Kenna JG . In vitro inhibition of the bile salt export pump correlates with risk of cholestatic drug-induced liver injury in humans. Drug Metab Dispos 2012; 40: 130–8.
Fattinger K, Funk C, Pantze M, Weber C, Reichen J, Stieger B, et al. The endothelin antagonist bosentan inhibits the canalicular bile salt export pump: a potential mechanism for hepatic adverse reactions. Clin Pharmacol Ther 2001; 69: 223–31.
Vrenken TE, Buist-Homan M, Kalsbeek AJ, Faber KN, Moshage H . The active metabolite of leflunomide, A77 1726, protects rat hepatocytes against bile acid-induced apoptosis. J Hepatol 2008; 49: 799–809.
Rodrigues AD, Lai Y, Cvijic ME, Elkin LL, Zvyaga T, Soars MG . Drug-induced perturbations of the bile acid pool, cholestasis, and hepatotoxicity: mechanistic considerations beyond the direct inhibition of the bile salt export pump. Drug Metab Dispos 2014; 42: 566–74.
Henríquez-Hernández LA, Flores-Morales A, Santana-Farré R, Axelson M, Nilsson P, Norstedt G, et al. Role of pituitary hormones on 17alpha-ethinylestradiol-induced cholestasis in rat. J Pharmacol Exp Ther 2007; 320: 695–705.
Wang T, Zhou ZX, Sun LX, Li X, Xu ZM, Chen M, et al. Resveratrol effectively attenuates α-naphthyl-isothiocyanate-induced acute cholestasis and liver injury through choleretic and anti-inflammatory mechanisms. Acta Pharmacol Sin 2014; 35: 1527–36.
Li J, Yao HW, Jin Y, Zhang YF, Li CY, Li YH, et al. Pharmacokinetics of leflunomide in Chinese healthy volunteers. Acta Pharmacol Sin 2002; 23: 551–5.
Vinken M, Maes M, Vanhaecke T, Rogiers V . Drug-induced liver injury: mechanisms, types and biomarkers. Curr Med Chem 2013; 20: 3011–21.
Watanabe T, Miyake M, Shimizu T, Kamezawa M, Masutomi N, Shimura T, et al. Utility of bilirubins and bile acids as endogenous biomarkers for the inhibition of hepatic transporters. Drug Metab Dispos 2015; 43: 459–66.
Acknowledgements
We are grateful to Cinkate Pharmaceutical Intermediates Co, Ltd (Shanghai, China) for providing leflunomide and teriflunomide as gifts. We thank Dr Lei GUO (NCTR, USA) for helpful discussions and comments. We thank Dr Jun GU (New York State Department of Health, USA) for kindly providing the HRN mice.
This project is supported by the Key Projects of National Science and Technology Program, China (Grant No 2012ZX09301001-006, 012ZX09302003 and 2012ZX09301001), and National Science and Technology Major Project “Key New Drug Creation and Manufacturing Program”, China (Grant No 2012ZX09303-001).
Author information
Authors and Affiliations
Corresponding authors
Additional information
Supplemental information is available at the Acta Pharmacologica Sinica's website.
Supplementary information
Supplemental Figure S1
Cytotoxicity of LEF and TER in primary rat hepatocytes. (JPG 149 kb)
Supplemental Figure S2
Effect of LEF and TER on the biliary excretion of d8-TCA. (JPG 224 kb)
Supplemental Methods
Measurement of the mitochondrial membrane potential (MMP) (DOC 126 kb)
Rights and permissions
About this article
Cite this article
Ma, Ll., Wu, Zt., Wang, L. et al. Inhibition of hepatic cytochrome P450 enzymes and sodium/bile acid cotransporter exacerbates leflunomide-induced hepatotoxicity. Acta Pharmacol Sin 37, 415–424 (2016). https://doi.org/10.1038/aps.2015.157
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2015.157
Keywords
This article is cited by
-
New equation to decipher the relationship between carbon isotopic composition of methane and maturity of gas source rocks
Science China Earth Sciences (2021)
-
Leflunomide increased the renal exposure of acyclovir by inhibiting OAT1/3 and MRP2
Acta Pharmacologica Sinica (2020)
-
Drug interactions in the treatment of rheumatoid arthritis and psoriatic arthritis
Rheumatology International (2020)
-
Formation mechanism of condensates, waxy and heavy oils in the southern margin of Junggar Basin, NW China
Science China Earth Sciences (2017)