Abstract
Aim:
The eicosanoids derived from phospholipids play key roles in inflammation. However, the profiles of serum eicosanoids in subclinical hypothyroidism (SH) patients and the effects of thyroxine replacement therapy (TRT) on these eicosanoids remain unclear. Many studies show that TSH regulates lipid metabolism. As eicosanoids derived from phospholipids play key roles in oxidative stress and immune function and inflammatory process, it was necessary to explore the profiles of serum eicosanoids in SH patients and the effects of thyroxine replacement therapy (TRT) on the eicosanoids.
Methods:
A total of 50 Chinese SH patients and 22 healthy volunteers were recruited. SH patients received TRT (L-T4, 25 and 50 mcg/d for patients with TSH≤10.0 mIU/L and TSH>10.0 mIU/L, respectively) for 3 months. Serum levels of major eicosanoids and cPLA2 were analyzed using LC-MS and clinical biochemical assays.
Results:
The serum levels of cPLA2, eicosanoids (8-isoPGF2a, 11-dehydroTXB2 and 12-HETE) and 11-dehydroTXB2/6-Keto-PGF1a were significantly elevated in SH patients. The serum TSH levels were significantly correlated with the levels of cPLA2 (r=+0.65), 11-dehydroTXB2 (r=+0.32) and 11-dehydroTXB2/6-Keto-PGF1a (r=+0.37). After 3-month TRT, the serum levels of TSH, cPLA2 and the above-mentioned eicosanoids in SH patients were significantly decreased.
Conclusion:
The metabolism of eicosanoids is significantly altered in Chinese SH patients, and TRT can ameliorate the abnormalities of serum eicosanoid levels.
Similar content being viewed by others
Introduction
Subclinical hypothyroidism (SH) is a common endocrine disease characterized by elevated serum thyroid stimulating hormone (TSH) but normal free thyroxine (FT4) and tri-iodothyronine (FT3). SH patients are divided into two groups based on serum TSH level: mild SH (TSH≤10.0 mIU/L, MSH) and severe SH (TSH>10.0 mIU/L, SSH)1. The overall incidence of SH is approximately 4%–20% and is higher in women, the elderly, and patients with autoimmune diseases (16%–20%)2. Because of the absence of obvious clinical symptoms, there may be more undiagnosed SH patients3. Many studies have indicated that SH patients show dyslipidemia, low-intensity chronic inflammation and a hypercoagulable state, which can cause consequences such as cardiac dysfunction, atherosclerosis and neuropsychiatric symptoms4,5,6. SH is an independent risk factor for atherosclerosis and myocardial infarction2,7. Therefore, it was believed that SH patients should be treated with thyroxine as a replacement therapy to reduce the occurrence of atherosclerosis, coronary heart disease and other serious diseases3,8. However, the question of when and how to administer replacement therapy to SH patients is still controversial9,10. Most scholars believe that SSH patients should be treated and that patients benefit from replacement therapy, but conclusions for MSH patients are inconsistent. Even for patients who accept replacement therapy, the way in which to determine the appropriate dose and timing of therapy is also disputed. It has been reported that up to 20% of levothyroxine-treated patients might be receiving excessive doses of thyroid hormone2. Over-replacement therapy also has potential hazards, such as subclinical hyperthyroidism, arrhythmias, cardiovascular and cerebrovascular infarction9,11. Thus, in addition to studying the mechanisms of SH development and its anomalies, more widespread and long-term studies on thyroxine replacement therapy are necessary to reveal the effects of treatment on the abnormalities of SH patients and the incidence of diseases caused by SH.
Dyslipidemia is the major symptom of SH patients. Our previous studies have demonstrated that high-fat feeding dramatically increases the concentration of TSH in the serum, and lipotoxicity may participate in thyroid dysfunction12. Many studies on the influence of thyroxine replacement therapy on the blood lipid characteristics of SH patients are controversial4,13,14. Lipolysis is one of the key steps in lipid metabolism. Its metabolites include many biologically active substances and their precursors and have important physiological and pathological significance. The thyroid is a critical organ for metabolic regulation, and thyroid dysfunction is known to interfere with lipolysis. Some studies have shown that serum PLA2-IIA (the key enzyme for phospholipid metabolism) is significantly increased in SH patients15. The dysfunction of PLA2 accounts for a vast number of diseases and it is a candidate for pharmacological research and intervention16. TSH promotes phospholipid hydrolysis catalyzed by Ca2+-regulated cytosolic phospholipase A2 (cPLA2), thus resulting in the production of many fatty acids, including arachidonic acids (AA, C20: 4, ω-6)17. AA is the precursor of many eicosanoids with different biological activities, such as prostaglandin E2 (PGE2), prostacyclin (PGI2), thromboxane A2 (TXA2), leukotriene B4 (LTB4) and C4 (LTC4). These eicosanoids play important regulatory roles in oxidative stress and immune and inflammatory functions (such as leukocyte and platelet function, bleeding and coagulation, allergic reactions) and are key factors in the development of a variety of diseases, especially inflammatory disease18,19. Eicosanoids include many molecules with different or opposite actions. PGF1a acts as a weak vasodilator. Hence, the increased ratio of 11-dehydroTXB2/6-Keto PGF1a in hypothyroid patients may represent a shift toward vasoconstriction. Numerous studies have shown that many eicosanoids play key roles in the development of atherosclerosis and are new biomarkers and drug therapy targets20,21,22,23. Therefore, whether the eicosanoid profile in SH patients is abnormal and associated with susceptibility to cardiovascular, cerebrovascular and other serious diseases and whether L-T4 replacement therapy (LTR) can affect the eicosanoid profile need to be studied further. However, studies on these issues have not been conducted to date.
In this study, we investigated the levels of major eicosanoids related to inflammation and its key enzyme cPLA2 in the sera of mild and severe SH patients and studied the effects of short-term LTR. The results showed that serum levels of cPLA2 and eicosanoids in SH patients increased significantly and the TSH levels were significantly correlated with all of these indicators. Levothyroxine replacement therapy significantly improved the abnormal levels of serum eicosanoids in SH patients, and this treatment might be appropriate for SH patients. However, more research is needed to determine whether SH patients will ultimately benefit from this treatment.
Materials and methods
Patients and ethical statement
Fifty SH patients (34 females, 16 males) were randomly recruited from the database of SH patients in Ningyang County according to the following diagnostic criteria: serum TSH levels>4.2 mIU/L, normal serum level of FT4 (12-22 pmol/L) and FT3 (3.1–6.8 pmol/L). Twenty-two age- and BMI-matched healthy volunteers were recruited as controls. The BMI and fasting blood glucose (FBG) were not significantly different among all groups. Subjects with acute and chronic diseases (such as tumors, renal/liver disease, diabetes mellitus, infection, and autoimmune diseases), or with a history of radioiodine exposure, thyroidectomy, treatment that might affect thyroid function were excluded, as were those who were taking anti-inflammatory or antiplatelet drugs. The Ethics Committee of Shandong University approved this study. Informed consent was obtained in accordance with the Declaration of Helsinki.
Patient treatment and sample preparation
Baseline data were collected from the recruited subjects. SH patients were divided into the SSH group (TSH>10.0 mlU/mL) (n=20) and the MSH group (4.2<TSH≤10.0 mlU/mL) (n=30) according to serum TSH levels. All the SH patients were treated with LTR. The dose of L-T4 was determined according to the serum TSH levels: 25 mcg q.d. for MSH and 50 mcg q.d. for SSH. Before and 3 months after treatments, blood samples were collected from all subjects after 8–12 h fasting for the following experiments.
Assay of thyroid-related hormones, serum levels of cPLA2 and 8-isoPG2a
Serum levels of FBG, total cholesterol (TC), triglyceride (TG), low-density lipoprotein cholesterol (LDL-C), and high-density lipoprotein cholesterol (HDL-C) were measured directly by using an Architect ci16200 Integrated Chemistry/Immunoassay System (Abbott, IL, USA). Serum levels of FT3, FT4 and TSH were assayed by electrochemiluminescence assays (Cobas E601, Roche Basel, Switzerland) at the clinical laboratory of Shandong Provincial Hospital. Serum levels of cPLA2 were determined with a kit from BlueGene Biotech (Shanghai, China). Briefly, 100 μL samples were added to the antibody pre-coated plate. After binding and washing, the cPLA2 concentration was measured by using a microplate reader. The serum level of 8-isoPG2a was determined using a competitive enzyme immunoassay kit (Cayman Chemical, Ann Arbor, MI, USA) following the manufacturer's manual.
Analysis of the concentration and activity of cPLA2
Peripheral blood mononuclear cells (PBMC) were isolated using LTS 1077 (TBD science, Tianjin, China) according to the manufacturer's instructions. Then, PBMCs were cultured in RPMI-1640 (Solarbio, Beijing, China) with 10% fetal bovine serum (Gibco, ThermoFisher, USA) and stimulated with four concentrations of TSH (0, 1, 2, and 4 μmol/L) for 24 h. After harvesting, the activity of cPLA2 in culture medium and cells was determined using an enzyme immunoassay kit (Cayman Chemical, Ann Arbor, MI, USA) according to the manufacturer's protocol. Before the activity assay, samples were incubated with specific inhibitors of sPLA2 and iPLA2 for 15 min. The concentration of cPLA2 secreted in culture medium and in cells was analyzed as previously mentioned. All of the above results were normalized to the protein concentration. All experiments were independently repeated at least three times.
Assay of serum eicosanoids by liquid chromatography-tandem mass spectrometry (LC-MS/MS)
Serum samples were added into ice-cold Folch solution containing 0.005% (w/v) butylated hydroxytoluene (BHT)24. After being subjected to vortexing and the addition of 1 mL 0.9% (w/v) NaCl, the sample was centrifuged at 2500×g at 4 °C for 10 min. The supernatant was dried and reconstituted with 500 μL methanol. After the pH was adjusted to 3.0, the mixture was incubated for 60 min at 37 °C. Then, 50 μL deuterated internal standard were added and the solution was extracted twice with 1 mL ethyl acetate. Extracts were combined, dried and reconstituted with 200 μL of 50% (v/v) LC mobile phase A (2 mmol/L NH4Ac, pH 5.6) and 50% (v/v) phase B (CH3CN:MeOH, 65:35, v/v), then centrifuged (10 000×g, 10 min, 4 °C). The supernatant was analyzed by LC-MS/MS. Using UltiMate 3000 series (Thermo Fisher Scientific, San Jose, CA, USA), chromatographic separation was performed on C18 columns (2.1 mm×100 mm, 2.8 μm, Acchrom Technologies) with stepwise linear gradient (30% B at 0 min, 50% B at 2 min, 80% B at 5 min, 100% at 17 min, 100% B at 19 min, and 30% B at 19.1 min). The flow rate was 0.2 mL/min. Eicosanoids were detected in the scheduled selected reaction monitoring mode (sSRM) with a Vantage triple quadrupole mass spectrometer (Thermo Fisher Scientific, San Jose, CA, USA). The capillary and vaporizer temperatures were 350 °C and 300 °C, respectively. The Aux Valve Flow was 15.0 and the spray voltage was 3500 V. A 9-point calibration curve (0–10 pg/mL) was prepared by diluted standard solution for the quantitative analysis of eicosanoids. Data were processed using Xcalibur software v1.4 (Thermo Fisher Scientific, San Jose, CA, USA).
Statistical analysis
Data are presented as the mean±standard deviation (SD). Continuous variables were compared among different groups with one-way ANOVA for normally distributed data and the Kruskal-Wallis test for non-normally distributed data. Statistical significance was set at P<0.05. Pearson's correlations and multiple regression analysis were used to assess the correlation between thyroid-related hormones, lipid profiles, cPLA2 and eicosanoids. Data were processed using SPSS 18.0 (SPSS Inc, Chicago, IL, USA).
Results
Serum eicosanoid levels were significantly increased in SH and were ameliorated by LTR
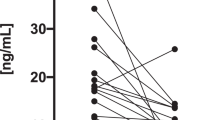
The baseline demographic and clinical characteristics of subjects in this study are shown in Table 1. Eicosanoids play important roles in the regulation of inflammation, coagulation and many other functions. However, the pattern of serum eicosanoids in SH patients remains unclear to date. Therefore, we analyzed the profiles of major eicosanoids in different SH patients before and after LTR treatment, by using LC-MS/MS. The results showed that the serum levels of major eicosanoids (11-dehydroTXB2, 12-HETE and 8-isoPGF2a) and the ratio of 11-dehydroTXB2/6-Keto PGF1a were significantly increased in SH patients compared to controls (Table 2). After three months of LTR, the serum levels of 8-isoPGF2a and 11-dehydroTXB2 as well as the ratio of 11-dehydroTXB2/6-Keto PGF1a were significantly decreased in MSH and SSH patients. Even then, the 11-dehydroTXB2 levels and the ratio of 11-dehydroTXB2/6-Keto PGF1a in SSH patients were still significantly higher than those in healthy individuals. However, these two indicators returned to normal levels in MSH patients (Figure 1A–1C).
L-T4 replacement therapy significantly decreased the serum levels of eicosanoids in SH patients. The serum levels of major eicosanoids in SH patients before and after L-thyroxine replacement (LTR) were measured as described in Materials and methods. After three months of LTR, the serum levels of 8-isoPGF2a (A) and 11-dehydroTXB2 (B) as well as the ratio of 11-dehydroTXB2/6-Keto PGF1a (C) were significantly decreased in mild subclinical hypothyroidism (MSH) and severe subclinical hypothyroidism (SSH) patients. P values are presented in the figure.
Serum cPLA2 levels in SH patients were significantly increased, and LTR ameliorated this abnormality
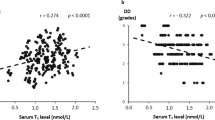
cPLA2 is the key enzyme for phospholipid metabolism and AA production and is the precursor of eicosanoids. Our results showed that cPLA2 concentrations in the MSH and SSH groups were significantly increased compared with those in the control group, and the effect was more pronounced in the SSH group (Figure 2A). After three months of LTR, the serum cPLA2 levels decreased significantly in MSH and SSH patients, and in MSH patients they even returned to levels found in healthy subjects. However, the cPLA2 levels were still significantly higher in SSH patients than in controls (Figure 2B). This result suggested that a long-term LTR may be necessary to recover serum cPLA2 of SSH patients to the levels found in healthy subjects. To reveal the factors involved in the increase of cPLA2, the relationships between cPLA2 levels and FBG, TG, TC, HDL-C, LDL-C, TSH, FT3 or FT4 levels were analyzed in all SH patients without LTR treatment. The results showed that serum levels of cPLA2 had significant and strong positive correlations with TSH (R=0.65, P=3.52×10−9), but not with other indicators (Figure 2C). There were still complex interactions among the above variables except for cPLA2. For example, the correlation coefficient between TC and LDL-C was 0.898 (P=9.63×10−19). Therefore, multiple regression analysis for the above-mentioned indicators was performed; this analysis suggested that the cPLA2 level also had the strongest correlation with serum TSH level (Table 3). All the results indicated that the abnormal levels of serum TSH might be one of the causes of increased serum cPLA2 levels in SH patients. Furthermore, the relationship between TSH and cPLA2 was analyzed in PBMCs of healthy donors. The results showed that TSH significantly increased the expression and activity of intracellular cPLA2, and there was a significant positive correlation between TSH and cPLA2 (Figure 2D). Additionally, the relationship between the concentration/activity of cPLA2 in the culture medium and in cells was analyzed. The results showed that the level of cPLA2 in the culture medium was significantly positively correlated with the activity of intracellular cPLA2, thus implying that the serum level of cPLA2 might also reflect its activity in the cells (Figure 2E).
L-T4 replacement therapy significantly decreased the serum levels of cPLA2 in SH patients. (A) The serum levels of cPLA2 in mild subclinical hypothyroidism (MSH) and severe subclinical hypothyroidism (SSH) patients were significantly increased compared to those in healthy individuals. *P<0.05 vs control. #P<0.05 vs MSH. (B) After three months of LTR, the serum cPLA2 levels decreased significantly in MSH and SSH patients and even returned to normal levels in MSH patients, but were still significantly higher in SSH patients than in controls. (C) Pearson's correlation analysis demonstrated that the serum level of cPLA2 had a significant and strong positive correlation with the TSH level. (D) PBMC were isolated from healthy adults and were stimulated in vitro with four concentrations of TSH (0, 1, 2 and 4 μmol/L) for 24 h. Then, the concentration and activity of cPLA2 in PBMCs was analyzed. The correlation coefficient (R) and P value are presented in the figure. TSH significantly increased the expression and activity of intracellular cPLA2. There was a close relationship between TSH and cPLA2. CL: cell lysate. (E) The activity of intracellular cPLA2 and the cPLA2 concentration in culture medium was determined. Then, Pearson's correlation was analyzed. CCM: cell culture medium; CL: cell lysate. The results indicated that the level of cPLA2 secreted in the culture medium was significantly positively correlated with the activity of intracellular cPLA2.
Serum levels of eicosanoids in SH patients were related to many factors, including TSH
To reveal the factors involved in the abnormalities of serum eicosanoids in SH patients, the correlations between serum levels of eicosanoids and thyroid-related hormones (FT3, FT4, TSH), cPLA2, blood lipids (TC, TG, HDL-C, LDL-C) in SH patients were analyzed. The results showed that 8-isoPGF2a was significantly positively correlated with TSH, cPLA2, TC, TG and LDL-C. Whereas 6-Keto PGF1a showed a significant negative correlation with TSH and TC, the correlation was weak. 5-HETE had a weak but significant positive correlation with TC and LDL-C. In addition, TSH was significantly positively correlated to 11-dehydroTXB2 and the ratio of 11-dehydroTXB2/6-Keto PGF1α. However, HDL-C, FT3 and other factors were not significantly correlated with eicosanoids and the ratio of 11-dehydroTXB2/6-Keto PGF1a (Table 4). These complex correlations indicated that the factors affecting eicosanoids in SH patients are very intricate, and further in-depth studies are needed to reveal the mechanisms behind these intricate correlations.
Discussion
Although SH patients have no overt clinical symptoms and their serum levels of FT3 and FT4 are normal, they present with clear abnormalities, such as lipid metabolism, bleeding and coagulation, inflammation, and reproduction4,15,25,26. This suggested that increased TSH levels may play key roles in abnormalities in SH patients and are worthy of further study. Many studies have shown that TSH regulates lipid metabolism through extrathyroidal functions. However, studies of the effects of TSH on phospholipid metabolism are still relatively scarce. It has been reported that TSH attenuates prostacyclin (PGI2) levels, resulting in endothelial dysfunction and promoting the release of AA by activating PLA2 by IP3 or Ca2+27,28. Our study indicated that the elevated TSH levels in SH patients were closely related to abnormal levels of many bioactive eicosanoids produced from AA metabolism. 12-HETE is an important proinflammatory cytokine and is the metabolite of AA catalyzed by 12-LOX29. The serum levels of 12-HETE is substantially increased in SH patients, especially in SSH patients. 11-dehydroTXB2 and 6-keto-PGF1a are the stable hydrolyzed products of TXA2 and PGI2, respectively, which are important metabolites of AA catalyzed by the COX enzyme. The TXA2/PGI2 ratio increases significantly in serum of SH patients, and this causes platelet aggregation and the release of various bioactive substances, including 5-hydroxytryptamine, which damages blood vessels30,31. TXA2 is a key endothelium-derived contracting factor (EDCF), that plays a role in the endothelial dysfunction that accompanies aging, atherosclerosis, myocardial infarction and essential hypertension32. 8-isoPGF2a is produced directly from arachidonic acid oxidation by oxygen free radicals instead of by the COX enzyme33. It is the most widely distributed isoprostane and is recognized as a good marker of oxidative stress34. Our results showed that 8-isoPGF2a gradually increased along with the aggravation of SH. This indicated that oxidative stress was enhanced along with the exacerbation of SH, namely, the increase of TSH levels. All of these results implied that TSH might play non-classical extrathyroidal roles in proinflammatory functions, platelet activation and the enhancement of oxidative stress through eicosanoids. These effects might be important mechanisms underlying the susceptibility of SH patients to atherosclerosis, coronary heart disease and other serious cardiovascular diseases35.
It is generally accepted that SSH patients should be treated with LTR. However, the questions of how to evaluate the efficacy and necessity of LTR for LSH patients remain controversial. Some studies have demonstrated that LTR reduces oxidative stress and inflammation in SH patients36,37. This study suggested that LTR may improve many abnormalities in SH patients, including increased levels of proinflammatory eicosanoids, which were closely correlated with elevated TSH levels. This improvement might contribute to a reduced incidence of atherosclerosis and other diseases. Our results also indicated that short-term LTR might be sufficient for MSH patients because the serum levels of TSH, cPLA2 and many eicosanoids in MSH patients were normalized after LTR for three months. However, it should be noted that our study had the limitations of a small sample size and short-term treatment. Currently, a study with a larger sample size and a longer treatment period is in progress.
In conclusion, this study show that serum levels of cPLA2, the key enzyme of arachidonic acid metabolism, and major eicosanoids were significantly increased in SH patients compared to healthy individuals. The significant correlation between TSH level and these abnormalities implies that TSH might play crucial roles in their development. Short-term LTR significantly improved the above-mentioned abnormalities. These results provide new insights into L-T4 replacement therapy from the viewpoint of arachidonic acid and inflammation and suggest that SSH patients should be treated with LTR. However, more in-depth studies should be performed to determine the ultimate benefit of LTR for SH patients.
Author contribution
Jia-jun ZHAO designed this study; Jin XU, Meng ZHAO and Zhe WANG collected samples from patients; Yan ZHANG, Bing-chang ZHANG, Yong-feng SONG and Hai-qing ZHANG conducted the experiments and analyzed the data; Qun-ye ZHANG and Lin GAO wrote the manuscript.
References
Baumgartner C, Blum MR, Rodondi N . Subclinical hypothyroidism: summary of evidence in 2014. SwissMed Wkly 2014; 144: w14058.
Cooper DS, Biondi B . Subclinical thyroid disease. Lancet 2012; 379: 1142–54.
Tseng FY, Lin WY, Lin CC, Lee LT, Li TC, Sung PK, et al. Subclinical hypothyroidism is associated with increased risk for all-cause and cardiovascular mortality in adults. J Am Coll Cardiol 2012; 60: 730–7.
Zhao M, Yang T, Chen L, Tang X, Guan Q, Zhang B, et al. Subclinical hypothyroidism might worsen the effects of aging on serum lipid profiles: a population-based case-control study. Thyroid 2015; 25: 485–93.
Selmer C, Olesen JB, Hansen ML, von Kappelgaard LM, Madsen JC, Hansen PR, et al. Subclinical and overt thyroid dysfunction and risk of all-cause mortality and cardiovascular events: a large population study. J Clin Endocrinol Metab 2014; 99: 2372–82.
Demartini B, Ranieri R, Masu A, Selle V, Scarone S, Gambini O . Depressive symptoms and major depressive disorder in patients affected by subclinical hypothyroidism: a cross-sectional study. J Nerv Ment Dis 2014; 202: 603–7.
Hak AE, Pols HA, Visser TJ, Drexhage HA, Hofman A, Witteman JC . Subclinical hypothyroidism is an independent risk factor for atherosclerosis and myocardial infarction in elderly women: the Rotterdam Study. Ann Intern Med 2000; 132: 270–8.
Lioudaki E, Mavroeidi NG, Mikhailidis DP, Ganotakis ES . Subclinical hypothyroidism and vascular risk: an update. Hormones (Athens) 2013; 12: 495–506.
Khandelwal D, Tandon N . Overt and subclinical hypothyroidism: who to treat and how. Drugs 2012; 72: 17–33.
Monzani A, Prodam F, Rapa A, Moia S, Agarla V, Bellone S, et al. Endocrine disorders in childhood and adolescence. Natural history of subclinical hypothyroidism in children and adolescents and potential effects of replacement therapy: a review. Eur J Endocrinol 2013; 168: R1–11.
Somwaru LL, Arnold AM, Joshi N, Fried LP, Cappola AR . High frequency of and factors associated with thyroid hormone over-replacement and under-replacement in men and women aged 65 and over. J Clin Endocrinol Metab 2009; 94: 1342–5.
Shao SS, Zhao YF, Song YF, Xu C, Yang JM, Xuan SM, et al. Dietary high-fat lard intake induces thyroid dysfunction and abnormal morphology in rats. Acta Pharmacol Sin 2014; 35: 1411–20.
Ito M, Kitanaka A, Arishima T, Kudo T, Nishihara E, Kubota S, et al. Effect of L-thyroxine replacement on apolipoprotein B-48 in overt and subclinical hypothyroid patients. Endocr J 2013; 60: 65–71.
Benvenga S . Effect of thyroxine on low density lipoprotein oxidation another thyroid hormone nongenomic effect. J Clin Endocrinol Metab 1998; 83: 3377–8.
Shojaei Nik MH, Darabi M, Ziaee A, Hajmanoochehri F . Serum phospholipase A2-IIA, hs-CRP, and lipids in women with subclinical hypothyroidism. Int J Endocrinol Metab 2014; 12: e16967.
Hu MM, Zhang J, Wang WY, Wu WY, Ma YL, Chen WH, et al. The inhibition of lipoprotein-associated phospholipase A2 exerts beneficial effects against atherosclerosis in LDLR-deficient mice. Acta Pharmacol Sin 2011; 32: 1253–8.
Philp NJ, Grollman EF . Thyrotropin and norepinephrine stimulate the metabolism of phosphoinositides in FRTL-5 thyroid cells. FEBS Lett 1986; 202: 193–6.
Miller E, Morel A, Saso L, Saluk J . Isoprostanes and neuroprostanes as biomarkers of oxidative stress in neurodegenerative diseases. Oxid Med Cell Longev 2014; 2014: 572491.
Alhouayek M, Muccioli GG . COX-2-derived endocannabinoid metabolites as novel inflammatory mediators. Trends Pharmacol Sci 2014; 35: 284–92.
Rago B, Fu C . Development of a high-throughput ultra performance liquid chromatography-mass spectrometry assay to profile 18 eicosanoids as exploratory biomarkers for atherosclerotic diseases. J Chromatogr B Analyt Technol Biomed Life Sci 2013; 936: 25–32.
Xu X, Zhang XA, Wang DW . The roles of CYP450 epoxygenases and metabolites, epoxyeicosatrienoic acids, in cardiovascular and malignant diseases. Adv Drug Deliv Rev 2011; 63: 597–609.
Capra V, Back M, Barbieri SS, Camera M, Tremoli E, Rovati GE . Eicosanoids and their drugs in cardiovascular diseases: focus on atherosclerosis and stroke. Med Res Rev 2013; 33: 364–438.
Ting HJ, Murray WJ, Khasawneh FT . Repurposing an old drug for a new use: glybenclamide exerts antiplatelet activity by interacting with the thromboxane A(2) receptor. Acta Pharmacol Sin 2010; 31: 150–9.
Yin H, Davis T, Porter NA . Simultaneous analysis of multiple lipid oxidation products in vivo by liquid chromatographic-mass spectrometry (LC-MS). Methods Mol Biol 2010; 610: 375–86.
Laway BA, War FA, Shah S, Misgar RA, Kumar Kotwal S . Alteration of lipid parameters in patients with subclinical hypothyroidism. Int J Endocrinol Metab 2014; 12: e17496.
Annerbo S, Lokk J . A clinical review of the association of thyroid stimulating hormone and cognitive impairment. ISRN Endocrinol 2013; 2013: 856017.
Tian L, Zhang L, Liu J, Guo T, Gao C, Ni J . Effects of TSH on the function of human umbilical vein endothelial cells. J Mol Endocrinol 2014; 52: 215–22.
Szabo J, Foris G, Keresztes T, Csabina S, Varga Z, Bako G, et al. Heterogeneous signal pathways through TSH receptors in porcine thyroid cells following stimulation with Graves' immunoglobulin G. Eur J Endocrinol 1998; 139: 355–8.
Chakrabarti SK, Cole BK, Wen Y, Keller SR, Nadler JL . 12/15-lipoxy_genase products induce inflammation and impair insulin signaling in 3T3-L1 adipocytes. Obesity (Silver Spring) 2009; 17: 1657–63.
Smith DD, Tan X, Tawfik O, Milne G, Stechschulte DJ, Dileepan KN . Increased aortic atherosclerotic plaque development in female apolipoprotein E-null mice is associated with elevated thromboxane A2 and decreased prostacyclin production. J Physiol Pharmacol 2010; 61: 309–16.
Kobayashi T, Tahara Y, Matsumoto M, Iguchi M, Sano H, Murayama T, et al. Roles of thromboxane A(2) and prostacyclin in the development of atherosclerosis in apoE-deficient mice. J Clin Invest 2004; 114: 784–94.
Wong MS, Vanhoutte PM . COX-mediated endothelium-dependent contractions: from the past to recent discoveries. Acta Pharmacol Sin 2010; 31: 1095–102.
Morrow JD, Minton TA, Badr KF, Roberts LJ 2nd . Evidence that the F2-isoprostane, 8-epi-prostaglandin F2 alpha, is formed in vivo. Biochim Biophys Acta 1994; 1210: 244–8.
Kostapanos MS, Spyrou AT, Tellis CC, Gazi IF, Tselepis AD, Elisaf M, et al. Ezetimibe treatment lowers indicators of oxidative stress in hypercholesterolemic subjects with high oxidative stress. Lipids 2011; 46: 341–8.
Madathil A, Hollingsworth KG, Blamire AM, Razvi S, Newton JL, Taylor R, et al. Levothyroxine improves abnormal cardiac bioenergetics in subclinical hypothyroidism: a cardiac magnetic resonance spectroscopic study. J Clin Endocrinol Metab 2015; 100: E607–10.
Razvi S, Ingoe L, Keeka G, Oates C, McMillan C, Weaver JU . The beneficial effect of L-thyroxine on cardiovascular risk factors, endothelial function, and quality of life in subclinical hypothyroidism: randomized, crossover trial. J Clin Endocrinol Metab 2007; 92: 1715–23.
Marfella R, Ferraraccio F, Rizzo MR, Portoghese M, Barbieri M, Basilio C, et al. Innate immune activity in plaque of patients with untreated and L-thyroxine-treated subclinical hypothyroidism. J Clin Endocrinol Metab 2011; 96: 1015–20.
Acknowledgements
This work was supported in part by the Chinese National Key Basic Research Project (2012CB524900, 2011CB503906) and the National Natural Science Foundation of China (81230018, 81370890, 81430020 and 81471006).
Author information
Authors and Affiliations
Corresponding authors
PowerPoint slides
Rights and permissions
About this article
Cite this article
Zhang, Y., Zhang, Bc., Xu, J. et al. Thyroxine therapy ameliorates serum levels of eicosanoids in Chinese subclinical hypothyroidism patients. Acta Pharmacol Sin 37, 656–663 (2016). https://doi.org/10.1038/aps.2015.149
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2015.149