Abstract
Aim:
To evaluate the relationship between epidermal growth factor receptor (EGFR) mutations and serum carcinoembryonic antigen (CEA) levels in Chinese nonsmokers with pulmonary adenocarcinoma.
Methods:
We sequenced exons 18–21 of the EGFR gene in 98 cases. The patients were divided into two groups based on their pre-treatment serum CEA levels (below or above 5 ng/mL) for analyzing the correlations with EGFR mutations.
Results:
Sixty-seven cases harbored EGFR mutations. The rates of EGFR mutations and exon 19 mutations in the high-CEA group (78.2% and 49.1%, respectively) were significantly higher those in the low-CEA group (55.8% and 20.9%, respectively). Serum CEA levels were found to be the only independent predictor of EGFR mutation (OR 2.837; 95% CI: 1.178–6.829) and exon 19 mutation (OR 3.618; 95% CI: 1.319–9.918). Furthermore, a higher serum CEA level was associated with a higher EGFR mutation rate and a higher exon 19 mutation rate: patients with serum CEA levels <5 ng/mL, ≥5 and <20 ng/mL, ≥20 ng/mL showed the EGFR mutation rate of 55.8%, 74.1%, 82.1%, respectively, and the exon 19 mutation rate of 20.9%, 40.7%, 57.1%, respectively. Patients with EGFR mutations displayed a significantly higher incidence of abnormal serum CEA levels (>5 ng/mL) than patients without EGFR mutations (64.2% vs 38.7%).
Conclusion:
Elevated serum CEA levels predict the presence of EGFR gene mutations in Chinese nonsmokers with pulmonary adenocarcinoma.
Similar content being viewed by others
Introduction
With the advances in molecular biology research on tumors and an increased understanding of the pathogenesis of tumor formation, targeted molecular therapy for advanced and metastatic non-small cell lung cancer (NSCLC) patients has become an important treatment approach. As proven by many large-scale clinical trials, molecular targeted therapy, exemplified by treatments such as epidermal growth factor receptor (EGFR)-tyrosine kinase inhibitors (TKIs), is highly effective in extending the life expectancy of NSCLC patients1,2. Given the good response and low toxicity, treating NSCLC patients who harbor an EGFR mutation with an EGFR-TKI as the first-line treatment is recommended, replacing conventional cytotoxic chemotherapy. However, the treatment effect of EGFR-TKIs varies greatly between different populations. Many studies have shown that Asian nonsmokers with lung adenocarcinoma3,4,5 and patients with EGFR mutation6,7,8 are more responsive to EGFR-TKI treatment. Other researchers reported that Asian nonsmokers with lung adenocarcinoma displayed a high rate of EGFR mutation6,8,9 indicating that mutations in the EGFR gene affect the treatment effects of EGFR-TKIs. It is therefore widely accepted that the presence of EGFR mutations is an indicator of the clinical efficacy of an EGFR-TKI in patients with NSCLC. Based on this concept, National Comprehensive Cancer Network (NCCN) clinical practice guidelines in oncology recommend measuring the local EGFR gene mutations of NSCLC patients before treatment.
Despite this development, it is still rare in current clinical practice to measure EGFR gene mutation. In the Iressa Pan-Asia Study8, although 1038 patients (85.3%) consented to provide tumor specimens, specimens were obtained from 683 patients (56.1%) in the end. Additionally, only 437 patients (35.9%) provided specimens that qualified for EGFR mutation detection, mainly due to the difficulty of obtaining adequate tissue samples. Therefore, for those patients with various reasons for limited availability of biopsy samples to detect EGFR mutation, if an easily measurable biomarker that is predictive of EGFR mutation can be established and accepted, this marker will significantly simplify the process of identifying the patient population that is ideal for EGFR-TKI therapy.
Carcinoembryonic antigen (CEA) levels in the serum have been widely recognized as a diagnostic indicator of lung cancer, and particularly adenocarcinoma10,11,12,13,14,15,16. It has also been reported that the serum CEA level is closely related to the treatment outcome of EGFR-TKIs17,18. These findings raise the question of whether there is any correlation between serum CEA levels and EGFR gene mutations. To answer this question, we designed and performed the current study, which measured serum CEA levels and EGFR gene mutations in histologically confirmed lung adenocarcinomas in Chinese patients without a smoking history. After dividing the patients into two groups by serum CEA level, we analyzed and compared the mutation rates of the EGFR gene (particularly at exon 19 and exon 21) between the two groups with different serum CEA levels. The current study investigated the correlation between serum CEA levels and EGFR gene mutation in Chinese nonsmokers with lung adenocarcinoma and offers to shed light on the potential to identify a patient population that is responsive to EGFR-TKI treatment in the absence of EGFR mutation detection due to limitations in the availability of biopsy samples.
Materials and methods
Ethics statement
The study was conducted in accordance with the Declaration of Helsinki and the guidelines set forth by the International Council on Harmonization of Technical Requirements for Registration of Pharmaceuticals for Human Use. The investigators obtained approval from the Institutional Review Board at the Shanghai Chest Hospital, Shanghai Jiao Tong University before initiating the study, and all patients provided written informed consent before any study-related procedures.
Study design
Patient inclusion criteria:
-
1
Diagnosis of lung adenocarcinoma per histology;
-
2
No history of smoking;
-
3
Chinese;
-
4
Never received any prior anti-cancer treatment.
Patient exclusion criteria:
-
1
No samples for EGFR mutation analysis;
-
2
Lung cancer identified as squamous cell carcinoma, small cell lung cancer, or large cell carcinoma;
-
3
History of smoking;
-
4
Non-Chinese;
-
5
Received prior anti-cancer treatment.
Clinicopathological characteristics, including gender, age, and the degree of differentiation, were recorded, and pre-treatment serum was collected for chemiluminescent immunoassay measurement of CEA, cytokeratin 19 fragment antigen 21-1 (CYFRA21-1), neuron specific enolase (NSE), and CA125 levels. An amplification refractory mutation system (ARMS) was used to detect EGFR gene mutation at exons 18–21.
Given that sequencing is still the most accepted technology for the measurement of EGFR gene mutations, to confirm the reliability of ARMS, 20% of samples were randomly selected from samples that were detected by ARMS to have point mutations at exon 19 and exon 21 to undergo sequencing.
We analyzed and compared the correlation between clinicopathological characteristics and EGFR gene mutations (especially at exon 19 and exon 21, which are the most common). We divided patients into high-CEA and low-CEA groups. The mutation rates of the EGFR gene (especially exon 19 and exon 21) were compared between the two groups, and the correlation between serum CEA levels and EGFR gene (especially exon 19 and exon 21) mutation rates was analyzed. In addition, we explored the relationship of the mutant or wildtype EGFR gene with abnormal serum CEA levels.
Specimen collection
Formalin-fixed and paraffin-embedded (FFPE) specimens were collected by surgical biopsy of primary lung adenocarcinoma, bronchoscopy, or percutaneous needle biopsy. H&E staining was applied for the pathological assessment and diagnosis of adenocarcinoma, while ensuring sufficient tumor tissue or cells for mutation detection. Moreover, tumor-rich regions were chosen for gene mutation analysis. The minimum number of slices was 5 μm×4 pieces for surgical biopsy specimens and 5 μm×8 pieces for bronchoscopy or percutaneous needle biopsy specimens.
EGFR mutational analysis
A QIAamp™ DNA FFPE Tissue Kit (Qiagen, Germantown, MD, USA) was used to accomplish DNA extraction and quality control. EGFR gene mutations at exons 18–21 were detected by an ADx-EG01 ARMS™ EGFR 29 Mutations Detection Kit (Amoy Diagnostics Co, Ltd, Xiamen, China). The specific operations and data interpretations were performed as indicated in the kit manual.
To verify the reliability of the ARMS results, we performed direct sequencing on 20% of the samples that exhibited the two mutation types with the highest incidence in this study (exon 19 deletions and exon 21 point mutations).
See Table 1 for information on the PCR primers and reaction system.
The DNA amplified by PCR was sequenced and analyzed using an ABI 3730 XL DNA sequencer (Life Technologies, Grand Island, NY, USA) in both directions.
Statistical analysis
Using SPSS 11.5, the chi-square test was applied to assess the correlation between EGFR gene mutations and every factor involved. Logistic regression models were used to analyze multiple factors. We selected the Forward: LR method for including variables.
Results
EGFR gene mutations
Mutations of the EGFR gene were detected in 67 (68.4%) of 98 patients. Among these mutations, 36 were deletions at exon 19, 26 were point mutations at exon 21 (23 were L858R, and 3 were L861Q), and 5 were double mutations (2 were exon 21 L858R with exon 20 mutation, 2 were exon 19 deletion with exon 20 mutation, and 1 was exon 19 deletion with exon 18 mutation). The distribution of the EGFR mutation status of all cases is shown in Figure 1.
Constitutional diagram of EGFR gene mutations in Chinese nonsmokers with pulmonary adenocarcinoma. In 98 cases, 36.7% (36 of 98) harbored EGFR mutations at exon 19, 26.5% (26 of 98) harbored EGFR mutations at exon 21, 5.1% (5 of 98) harbored double exons EGFR mutations, 31.6% (31 of 98) were wild-type.
Direct sequencing analysis to verify ARMS results
Sequencing analysis was performed on 12 samples, which were selected from samples with the two types of mutations with the highest incidence (exon 19 deletions and exon 21 point mutations). Direct sequencing results revealed that 7 of these 12 cases were deletions at exon 19, and 5 were L858R point mutations at exon 21, which was the same as the ARMS results. Thus, the direct sequencing analysis confirmed the reliability an d accuracy of the ARMS method. The direct sequencing results of the 12 samples are shown in Figure 2.
Gene sequence diagram of case 1–12. Note, direct sequencing on selected samples (20% of total) with exon 19 deletion and exon 21 point mutation was performed to verify the reliability of ARMS results.
Patient characteristics
This study included 98 patients, ranging in age from 38 to 76 years, with a median age of 57 years. The profiles of those patients are summarized in Table 2, including gender, age, tumor differentiation, serum CEA levels, and the expression level of other tumor biomarkers, such as CYFRA21-1, NSE, and CA125.
Clinicopathological characteristics and EGFR gene mutations
The distribution of EGFR gene mutations and their associations (in particular, at exon 19 and exon 21) with every clinicopathological characteristic are listed in Table 3.
We found that EGFR gene mutation rates were significantly higher in patients with high serum CEA levels (≥5 ng/mL) than those in patients with low serum CEA levels (<5 ng/mL), with EGFR gene mutation rates at 78.2% and 55.8%, respectively (P=0.018). We also found that the mutation rates of the EGFR gene were positively correlated with the degree of tumor differentiation: the mutation rates were 51.9% in poorly differentiated tumors, 68.6% in moderately differentiated tumors, and 90.0% in well-differentiated tumors (P=0.021).
Mutation rates at EGFR exon 19 were significantly higher in the high-CEA group than those in the low-CEA group, at 49.1% and 20.9%, respectively (P=0.004).
No association was found between mutation at exon 21 and the analyzed clinicopathological characteristics.
Additionally, subgroup analysis (Table 4) indicated that whether male or female, patients with higher serum CEA levels had a much higher rate of EGFR mutation than patients with lower serum CEA levels had. For males, those with low serum CEA levels (<5 ng/mL) and high serum CEA levels (≥5 ng/mL) had EGFR mutation rates of 47.1% and 77.8%, respectively (P=0.05); exon 19 mutation rates of 17.6% and 44.4%, respectively (P=0.038); and exon 21 mutation rates of 17.6% and 33.3%, respectively (P=0.289). For females, those with low serum CEA levels (<5 ng/mL) and high serum CEA levels (≥5 ng/mL) had EGFR mutation rates of 61.5% and 78.4%, respectively (P=0.047); exon 19 mutation rates of 23.1% and 51.4%, respectively (P=0.024); and exon 21 mutation rates of 30.8% and 24.3%, respectively (P=0.570).
Logistic regression analysis of EGFR gene mutation
The results of logistic regression analysis (Table 5) showed that a high level of serum CEA was the only independent predictor of EGFR gene mutation (P=0.020, OR 2.837, 95% CI: 1.178–6.829). A high level of serum CEA was also the only independent predictor of exon 19 mutations (P=0.012, OR 3.618, 95% CI: 1.319–9.918).
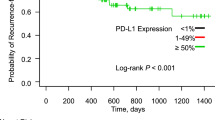
Serum CEA levels and EGFR gene mutations
In this study, the mutation rates of the EGFR gene in patients with <5 ng/mL, 5–20 ng/mL, or ≥20 ng/mL serum CEA were 55.8%, 73.1%, and 82.8%, respectively (P=0.046) (Figure 3). The mutation rates of exon 19 in these three groups were 20.9%, 40.7%, and 57.1%, respectively (P=0.007) (Figure 4). The mutation rates at exon 21 showed no significant difference among the three groups (25.6%, 26.9%, and 27.6%, respectively, P=0.981). These results suggested that serum CEA levels were positively correlated with histological EGFR gene mutation rates, especially for mutations at exon 19.
Proportion of patients with EGFR mutation in different serum CEA levels. 43 cases of serum CEA levels <5 ng/mL; 36 cases of serum CEA levels ≥20 ng/mL; 19 cases of serum CEA levels in between.
Proportion of patients with EGFR exon 19 mutation in different serum CEA levels. 9 cases of serum CEA levels <5 ng/mL; 16 cases of serum CEA levels ≥20 ng/mL; 11 cases of serum CEA levels in between.
EGFR gene types and serum CEA levels
The incidence of abnormal serum CEA levels (≥5 ng/mL) differed between patients with different types of EGFR gene mutations (Figure 5). Patients with a mutant EGFR gene displayed significantly higher CEA levels than patients with a wildtype EGFR gene. Whereas only 38.7% of wildtype patients were found to have an abnormal CEA level, in their mutated counterparts, the incidence was 64.2% (P=0.018). Specifically, 75.0% (P=0.004) of patients with exon 19 mutations and 57.7% (P=0.851) of patients with exon 21 mutations were observed to have abnormal serum CEA levels.
Proportion of patients with CEA abnormal in wild-type or mutant EGFR genes. 31 cases of wild-type; 67 cases of total EGFR mutation with 36 cases of exon 19 mutation and 26 cases of exon 21 mutation.
Discussion
It is well known that the type of EGFR gene is closely associated with EGFR-TKI treatment effects. The Iressa Pan-Asia Study has demonstrated that the presence of a mutation of the EGFR gene in a tumor is a strong predictor of a better outcome when gefitinib is used as the first-line treatment8. The WJTOG3405 study conducted by Mitsudomi et al also proved the importance of EGFR mutation measurement6. It is now well accepted that patients with EGFR gene mutations are more sensitive to EGFR-TKI treatment, with a better treatment outcome6,7,8. It has also been reported that the pre-treatment serum CEA level is associated with EGFR-TKI treatment efficacy; patients with a higher level of pre-treatment serum CEA are more sensitive than patients with normal serum CEA levels19,20,21. Therefore, is there any correlation between serum CEA levels and EGFR gene mutation?
Shoji et al reported that serum CEA levels correlated with EGFR gene mutation in 48 cases with postoperative recurrence of lung adenocarcinomas22. Additionally, researchers found that 59.7%–75.3% Asian nonsmokers with lung adenocarcinomas harbored EGFR gene mutations6,8,9. Thus, is it more relevant to apply serum CEA levels as a predictive biomarker in Asian nonsmokers with lung adenocarcinomas to assess the EGFR-TKI treatment outcome?
To answer this question, we focused on nonsmokers with lung adenocarcinomas, which is a population with a high incidence of EGFR gene mutation, and demonstrated that CEA levels were positively correlated with histological EGFR gene mutations and mutations at exon 19. Moreover, logistic regression analysis showed that a high level of serum CEA was the only independent predictor of EGFR gene mutations, and especially mutations at exon 19. More importantly, our results showed that patients with serum CEA levels ≥20 ng/mL had an EGFR gene mutation rate as high as 82.8%. Therefore, we conclude that in the population of Chinese nonsmokers with pulmonary adenocarcinoma, a high serum CEA level is an indicator of EGFR mutation.
EGFR gene mutation detection is still based on tissue sample analysis. In most Phase 3 trials for EGFR-TKIs, biomarker detection also requires tissue biopsy samples. Because the majority of NSCLC patients have no operative indications at the time of diagnosis, no surgical specimens would be available for the detection of gene mutation in these patients. In patients whose biopsy samples are obtained by bronchoscopy or CT-guided percutaneous lung biopsy, the sample volume limitation often does not allow gene mutation measurement. In addition, many patients with a poor performance status (PS) could not endure invasive biopsy examinations. These constraints ultimately limit the application of EGFR-TKIs to treat NSCLC patients.
CEA was first identified in rectal adenocarcinoma in 196523. The diagnostic value of serum CEA levels in NSCLC, and particularly adenocarcinoma patients, has already been widely accepted and utilized10,11,12,13,14,15,16. In certain reports, including those of our previous research, it has been found that changes in serum CEA levels are closely associated with chemotherapeutic efficacy and prognosis24,25. Notably, researchers have also found that serum CEA levels could be applied as a predictive biomarker for EGFR-TKI treatment effects17,18. Those previous studies suggest that serum CEA levels possess a certain value in clinical application for the prediction of treatment efficacy and prognosis.
Serum CEA is frequently found to be highly expressed in NSCLC, and especially in adenocarcinoma patients26,27. Additionally, adenocarcinoma patients display significantly higher mutation rates of the EGFR gene than do non-adenocarcinoma patients28. Shoji et al reported that in lung adenocarcinoma patients with post-operative recurrence, serum CEA levels are positively correlated with EGFR mutation rates22. However, our study results clearly demonstrated that Chinese nonsmokers with pulmonary adenocarcinoma, whether male or female, who had serum CEA levels ≥20 ng/mL are the ideal patient population to be targeted for EGFR-TKI therapy. As we known, patients with exon 19 mutations usually have longer PFS and OS. More interestingly, the mutation rate of exon 19 is more closely related to serum CEA levels. Regarding the exon 21 mutation rate, it also appears to correlate with serum CEA levels, but the correlation did not show statistical significance, highlighting the exon 19 mutation rate as a more important factor related to serum CEA levels.
Sordella et al reported that the mutated EGFR gene could abnormally activate the downstream signal transduction pathway and induce transcription factor expression and activation, thus initiating the anti-apoptotic pathway and accelerating cell proliferation, which play an important role in the tumorigenesis of lung cancer29. The mechanism by which EGFR-TKIs inhibit tumor development is the disruption of the EGFR mutation-induced abnormal downstream signaling pathway to induce the apoptosis of tumor cells. CEA is an adhesion protein, and its expression may be upregulated by the EGFR downstream signaling pathway. Wirth et al and Ordonez et al reported that CEA overexpression could inhibit the apoptosis of tumor cells30,31. Based on these studies, we could conclude that CEA might be an anti-apoptotic factor related to EGFR gene mutations, and particularly exon 19 mutation. This hypothesis still needs to be verified by further basic cancer research.
Although the mechanism that underlies the positive correlation between serum CEA levels and EGFR gene mutation remains unclear, serum CEA level determination could still serve as a straightforward indicator in patients who are unable to provide sufficient tissue specimens for EGFR gene mutation detection and could guide individualized treatment strategies. Furthermore, as several studies have noted, the serum CEA level is closely associated with EGFR-TKI treatment efficacy, so this level may also be used as a potential indicator of follow-up and prognosis, especially when the treatment effect is difficult to measure. We are taking this direction in future research on this topic.
Author contribution
Bao-hui HAN designed the research; Bo JIN, Yu DONG, Hui-min WANG, and Jin-su HUANG performed the research; Bo JIN and Yu DONG analyzed the data; and Bo JIN wrote the paper.
References
Shepherd FA, Rodrigues Pereira J, Ciuleanu T, Tan EH, Hirsh V, Thongprasert S, et al. Erlotinib in previously treated non-small-cell lung cancer. N Engl J Med 2005; 353: 123–32.
Kim ES, Hirsh V, Mok T, Socinski MA, Gervais R, Wu YL, et al. Gefitinib versus docetaxel in previously treated (INTEREST): a randomized phase III trial. Lancet 2008; 372: 1809–18.
Kris MG, Natale RB, Herbst RS, Lynch TJ Jr, Prager D, Belani CP, et al. Efficacy of gefitinib, an inhibitor of the epidermal growth factor receptor tyro-sine kinase, in symptomatic patients with non-small cell lung cancer: a randomized trial. JAMA 2003; 290: 2149–58.
Fukuoka M, Yano S, Giaccone G, Tamura T, Nakagawa K, Douillard JY, et al. Multi-institutional randomized phase II trial of gefitinib for previously treated patients with advanced non-small-cell lung cancer. J Clin Oncol 2003; 21: 2237–46.
Thatcher N, Chang A, Parikh P, Rodrigues Pereira J, Ciuleanu T, von Pawel J, et al. Gefitinib plus best supportive care in previously treated patients with refractory advanced non-small cell lung cancer: results from a randomized, placebo-controlled, multicentre study (Iressa Survival Evaluation in Lung Cancer). Lancet 2005; 366: 1527–37.
Mitsudomi T, Morita S, Yatabe Y, Negoro S, Okamoto I, Tsurutani J, et al. Gefitinib versus cisplatin plus docetaxel in patients with non-small-cell lung cancer harbouring mutations of the epidermal growth factor receptor (WJTOG3405): an open label, randomised phase 3 trial. Lancet Oncol 2010; 11: 121–8.
Inoue A, Kobayashi K, Usui K, Maemondo M, Okinaga S, Mikami I, et al. First-line gefitinib for patients with advanced non-small-cell lung cancer harboring epidermal growth factor receptor mutations without indication for chemotherapy. J Clin Oncol 2009; 27: 1394–400.
Mok TS, Wu YL, Thongprasert S, Yang CH, Chu DT, Saijo N, et al. Gefitinib or carboplatin-paclitaxel in pulmonary adenocarcinoma. N Engl J Med 2009; 361: 947–57.
Li C, Fang R, Sun Y, Han X, Li F, Gao B, et al. Spectrum of oncogenic driver mutations in lung adenocarcinomas from East Asian never smokers. PLoS One 2011; 6: e28204.
Trapé J, Buxo J, Pérez de Olaguer J, Vidal C . Tumor markers as prognostic factors in treated non-small cell lung cancer. Anticancer Res 2003; 23: 4277–81.
Kasimir-Bauer S, Schleucher N, Weber R, Neumann R, Seeber S . Evaluation of different markers in non-small cell lung cancer: prognostic value of clinical staging, tumor cell detection and tumor marker analysis for tumor progression and overall survival. Oncol Rep 2003; 10: 475–82.
Pujol JL, Molinier O, Ebert W, Daurès JP, Barlesi F, Buccheri G, et al. CYFRA 21-1 is a prognostic determinant in non-small-cell lung cancer: results of a meta-analysis in 2063 patients. Br J Cancer 2004; 90: 2097–105.
Muley T, Dienemann H, Ebert W . CYFRA 21-1 and CEA are independent prognostic factors in 153 operated stage I NSCLC patients. Anticancer Res 2004; 24: 1953–6.
Barlési F, Gimenez C, Torre JP, Doddoli C, Mancini J, Greillier L, et al. Prognostic value of combination of Cyfra 21-1, CEA and NSE in patients with advanced non-small-cell lung cancer. Respir Med 2004; 98: 357–62.
Molina R, Filella X, Augé JM, Fuentes R, Bover I, Rifa J, et al. Tumor markers (CEA, CA 125, CYFRA 21-1, SCC and NSE) in patients with non-small-cell lung cancer as an aid in histological diagnosis and prognosis. Comparison with the main clinical and pathological prognostic factors. Tumor Biol 2003; 24: 209–18.
Lee JH, Chang JH . Diagnostic utility of serum and pleural fluid carcinoembryonic antigen, neuron-specific enolase, and cytokeratin 19 fragments in patients with effusions from primary lung cancer. Chest 2005; 128: 2298–303.
Xu Y, Chen L, Tian Q, Yang Z, Zhao W, Wang P, et al. Application of epidermal growth factor receptor tyrosine kinase inhibitor as the first-line therapy in patients with advanced non-small cell lung cancer. Zhongguo Fei Ai Za Zhi 2010; 13: 48–53.
Kappers I, Vollebergh MA, van Tinteren H, Korse CM, Nieuwenhuis LL, Bonfrer JM, et al. Soluble epidermal growth factor receptor (sEGFR) and carcinoembryonic antigen (CEA) concentration in patients with non-small cell lung cancer: correlation with survival after erlotinib and gefitinib treatment. Ecancermedicalscience 2010; 4: 178.
Okamoto T, Nakamura T, Ikeda J, Maruyama R, Shoji F, Miyake T, et al. Serum carcinoembryonic antigen as a predictive marker for sensitivity to gefitinib in advanced non-small cell lung cancer. Eur J Cancer 2005; 41: 1286–90.
Zhao LD, Li JL, Wang Y, Wang B, Wang HY, Hao XZ, et al. Factors affecting the sensitivity of EGFR-TKI treatment in advanced non-small cell lung cancer. Zhonghua Zhong Liu Za Zhi 2011; 33: 217–21.
Jung M, Kim SH, Lee YJ, Hong S, Kang YA, Kim SK, et al. Prognostic and predictive value of CEA and CYFRA 21-1 levels in advanced non-small cell lungcancer patients treated with gefitinib or erlotinib. Exp Ther Med 2011; 2: 685–93.
Shoji F, Yoshino I, Yano T, Kometani T, Ohba T, Kouso H, et al. Serum carcinoembryonic antigen level is associated with epidermal growth factor receptor mutations in recurrent lung adenocarcinomas. Cancer 2007; 110: 2793–8.
Gold P, Freedman SO . Demonstration of tumor-specific antigens in human colonic carcinoma by immunological tolerance and absorption techniques. J Exp Med 1965; 121: 439–62.
Jin B, Huang AM, Zhong RB, Han BH . The value of tumor markers in evaluating chemotherapy response and prognosis in Chinese patients with advanced non-small cell lung cancer. Chemotherapy 2010; 56: 417–23.
Ishiguro F, Fukui T, Mori S, Katayama T, Sakakura N, Hatooka S, et al. Serum carcinoembryonic antigen level as a surrogate marker for the evaluation of tumor response to chemotherapy in nonsmall cell lung cancer. Ann Thorac Cardiovasc Surg 2010; 16: 242–7.
Molina R, Agusti C, Mañe JM, Filella X, Jo J, Joseph J, et al. CYFRA 21-1 in lung cancer: comparison with CEA, CA 125, SCC and NSE serum levels. Int J Biol Markers 1994; 9: 96–101.
Yoshino I, Ichinose Y, Nagashima A, Takeo S, Motohiro A, Yano T, et al. Clinical characterization of node-negative lung adenocarcinoma: results of a prospective investigation. J Thorac Oncol 2006; 1: 825–31.
Molina R, Augé JM, Bosch X, Escudero JM, Viñolas N, Marrades R, et al. Usefulness of serum tumor markers, including progastrin-releasing peptide, in patients with lung cancer: correlation with histology. Tumor Biol 2009; 30: 121–9.
Sordella R, Bell DW, Haber DA, Settleman J . Gefitinib-sensitizing EGFR mutations in lung cancer activate anti-apoptotic pathways. Science 2004; 305: 1163–7.
Wirth T, Soeth E, Czubayko F, Juhl H . Inhibition of endogenous carcinoembryonic antigen (CEA) increases the apoptotic rate of colon cancer cells and inhibits metastatic tumor growth. Clin Exp Metastasis 2002; 19: 155–60.
Ordoñez C, Screaton RA, Ilantzis C, Stanners CP . Human carcinoembryonic antigen functions as a general inhibitor of anoikis. Cancer Res 2000; 60: 3419–24.
Acknowledgements
This work was supported by Key projects of Biomedicine Department, Science and Technology Commission of Shanghai Municipality (Project No 11411951200) and Shanghai Chest Hospital, Shanghai Jiao Tong University, Shanghai, China (Project No Y211-12).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Jin, B., Dong, Y., Wang, Hm. et al. Correlation between serum CEA levels and EGFR mutations in Chinese nonsmokers with lung adenocarcinoma. Acta Pharmacol Sin 35, 373–380 (2014). https://doi.org/10.1038/aps.2013.164
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2013.164
Keywords
This article is cited by
-
Detection of EGFR gene polymorphisms in non-small cell lung cancer Egyptian patients: a case–control study
Genes and Environment (2023)
-
Identification of EGFR mutation status in male patients with non-small-cell lung cancer: role of 18F-FDG PET/CT and serum tumor markers CYFRA21-1 and SCC-Ag
EJNMMI Research (2023)
-
Correlation between carcinoembryonic antigen (CEA) expression and EGFR mutations in non-small-cell lung cancer: a meta-analysis
Clinical and Translational Oncology (2023)
-
Predicting EGFR mutation, ALK rearrangement, and uncommon EGFR mutation in NSCLC patients by driverless artificial intelligence: a cohort study
Respiratory Research (2022)