Abstract
Aim:
To study the protective effects of tiopronin against high fat diet-induced non-alcoholic steatohepatitis in rats.
Methods:
Male Sprague-Dawley rats were given a high-fat diet for 10 weeks. The rats were administered tiopronin (20 mg/kg) or a positive control drug ursodeoxycholic acid (UDCA, 15 mg/kg) via gavage daily from week 5 to week 10. After the rats were sacrificed, serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), total cholesterol (TC), triglyceride (TG), free fatty acids (FFA), high-density lipoprotein (HDL-C) and low-density lipoprotein (LDL-C), and liver homogenate FFA, superoxide dismutase (SOD), glutathione peroxidase (GSH-Px) and malondialdehyde (MDA) were measured using commercial analysis kits. The expression levels of CYP2E1 mRNA and protein were determined using RT-PCR and immunoblot assays, respectively.
Results:
Tiopronin significantly lowered both the serum ALT and AST levels, while only the serum ALT level was lowered by UDCA. Tiopronin significantly decreased the serum and liver levels of TG, TC and FFA as well as the serum LDL-C level, and increased the serum HDL-C level, while UDCA decreased the serum and liver TC levels as well as the serum LDL-C level, but did not change the serum levels of TG, FFA and HDL-C. Tiopronin apparently ameliorated the hepatocyte degeneration and the infiltration of inflammatory cells in the livers, but UDCA did not affect the pathological features of the livers. Both tiopronin and UDCA ameliorated the mitochondrial abnormality in the livers. The benefits of tiopronin were associated with increased SOD and GSH-Px activities, and with decreased MDA activity and CYP2E1 expression in the livers.
Conclusion:
Tiopronin exerts protective effects against non-alcoholic steatohepatitis in rats, which may be associated with its antioxidant properties and regulation of lipid metabolism.
Similar content being viewed by others
Introduction
Non-alcoholic fatty liver disease (NAFLD) is emerging as a common medical problem and is recognized as a cause of potentially progressive liver damage. Within the spectrum of NAFLD, non-alcoholic steatohepatitis (NASH) is considered the critical turning point at which point NAFLD progresses to more advanced stages such as hepatic fibrosis, cirrhosis and even hepatocellular carcinoma.
The pathogenesis of NAFLD is complex, multifactorial and poorly understood. Currently, the popular theory on NASH pathogenesis is the “two-hit” hypothesis1 in which the first hit leads to hepatic steatosis, which makes the liver vulnerable to the second hit. In this stage, steatosis is mediated by an increase in dietary fat intake, the liberation of free fatty acids from adipose tissue, insufficient hepatic lipid secretion and the development of insulin resistance2. The second hit, which leads to steatohepatitis, is mediated by increased oxidative stress subsequent to lipid peroxidation as well as the induction of pro-inflammatory cytokine expression.
Gradual weight loss is the only therapeutic strategy established to be effective in treating NASH. It has been proven that lifestyle modification and regular physiological exercise will regulate the individual's body weight and improve NASH and the associated metabolic syndrome3,4,5. However, if there is no change in the course of disease after adequate lifestyle changes, pharmacological interventions should be considered, especially for those patients at a high risk of progression. There is generally consistent evidence from clinical trials indicating that certain pharmacological agents may be effective in the treatment of NASH.
Tiopronin [N-(2-mercaptopropionyl)-glycine], a chemical compound with a free thiol group, is an oxygen free radical that has been used clinically in the treatment of several disorders linked to abnormal free radical production6,7,8. Tiopronin is readily absorbed after oral administration and is generally reported to be a well-tolerated drug8. The oral administration of 600 mg of tiopronin daily was associated with improvement in liver function in patients with viral chronic hepatitis9,10. It has also been reported that tiopronin is able to reduce fat levels in the liver after acute or prolonged ethanol administration11. The histologic characteristics of NAFLD resemble those of alcoholic fatty liver disease (AFLD), which suggests that both diseases may have a similar pathogenesis and benefit from similar therapies. Tiopronin was used in the treatment of hepatic steatosis in certain clinical trials12,13. Most of these studies have been uncontrolled and open label with a duration of 1 year or less. Only a few have evaluated the effect of treatment on liver histology. Therefore, this study was designed to evaluate the protective effects of tiopronin on high-fat-diet-induced NASH in rats and its mechanism of action.
Ursodeoxycholic acid (UDCA) is a hydrophilic biliary acid known to possess antioxidant properties and cytoprotective, anti-apoptotic, membrane stabilizing and immunomodulative effects14,15,16. It is suggested that UDCA treatment may improve aminotransferase and adiponectin levels as well as the grade of steatosis in NASH patients17,18,19,20. UDCA was also reported to enhance the therapeutic effects of a low-caloric diet in a rat model of NASH21. Thus, it served as a positive control drug in this study.
Materials and methods
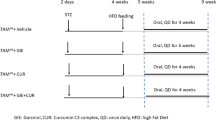
Experimental model and drug treatment
Male Sprague-Dawley rats weighing 180–200 g were obtained from the Experimental Animal Center of Anhui Medical University. The study protocol was approved by the ethics committee of Anhui Medical University. Rats were housed in plastic cages with room temperature of 22±1 °C under a 12-h light:dark cycle and were provided with standard rodent chow and water ad libitum. Rats were given a normal diet for 1 week to adapt to vivarium conditions and then randomly divided into four groups (n=10 per group): a normal control group, a high-fat diet group, a high-fat diet with tiopronin (20 mg/kg) treatment group and a high-fat diet with UDCA (15 mg/kg) treatment group. The NASH model was induced by high-fat emulsion as previously reported22. Briefly, rats were orally treated with the high-fat emulsion (10 mL/kg) at 8:00 AM. each day for 10 weeks, with the exception of the normal control group, which received an equal volume of saline alone. In the treatment groups, 20 mg/kg of tiopronin (Henan Xinyi Pharmaceutical Co, Ltd) or 15 mg/kg of UDCA (Sigma-Aldrich, St Louis, MO, USA) was given via gavage daily at 6:00 PM from the 5th week in rats fed a high-fat diet. UDCA and tiopronin were suspended in 0.5% CMC-Na solution. The normal control and high-fat diet groups were given an equal volume of 0.5% CMC-Na solution. Rats were sacrificed after 10 weeks. Blood samples were collected from the aorta ventralis. The livers were immediately removed and weighed. Specimens of isolated rat livers were fixed in 10% formalin or frozen in liquid nitrogen until use.
Analytical procedures
The serum levels of alanine aminotransferase (ALT), aspartate aminotransferase (AST), total cholesterol (TC), triglyceride (TG), free fatty acids (FFA), high-density lipoprotein (HDL-C), low-density lipoprotein (LDL-C), liver homogenate FFA, superoxide dismutase (SOD), glutathione peroxidase (GSH-Px) and malondialdehyde (MDA) were determined using commercial analysis kits obtained from the Jiancheng Institute of Biotechnology (Nanjing, China) and the Furui Institute of Biotechnology (Beijing, China). Hepatic concentrations of TC and TG were also measured after chloroform–methanol extraction23.
Semi-quantitative reverse transcription-polymerase chain reaction (RT-PCR)
Total RNA was extracted from rat liver tissues using TRIzol reagent (Invitrogen). The first-strand cDNA was synthesized from total RNA using the Thermoscript RT-PCR synthesis kit (Fermentas) according to the manufacturer's instructions. RT-PCR was carried out under the standard protocol using the following primers: β-actin (forward: 5′-TGGAATCCTGTGGCATCCATGAAAC-3′; reverse: 5′-ACGCAGCTCAGTAACAGTCCG-3′); CYP2E1 (forward: 5′-CCTAGCGCACATGGCGGTTCT-3′; reverse: 5′-GCCTCCCTTTGGATGCGGGC-3′). PCR was performed, using the ABI9700, at 94 °C for 2 min, followed by 30–33 cycles of amplification at 94 °C for 36 s, 52 °C for 36 s and 72 °C for 1 min. The band intensities were measured by a densitometer, and the results were normalized with β-actin. The results were repeated in at least three independent experiments under each condition, while each cDNA template was extracted from at least six samples per group.
Immunoblot analysis
Liver tissue was homogenized in RIPA lysis buffer. Samples were then centrifuged at 15 000×g for 15 min. Supernatants from each sample were added to a gel-loading buffer and boiled for 5 min. Proteins in loading buffer were subjected to electrophoresis in a 10% SDS-polyacrylamide gel for 3 h. Proteins in the gel were transferred electrophoretically onto a polyvinylidene fluoride membrane (Immobilon-P; Millipore Corp, Bedford, MA, USA) and blocked in 5% nonfat powdered milk in PBS overnight at 4 °C. The membranes were then incubated for 2 h with rabbit polyclonal antibody against mouse CYP2E1 (Millipore Corp, Bedford, MA, USA) (1:2500 dilutions) or β-actin (Beijing Biosynthesis Biotechnology Inc, Beijing, China) (1:2000 dilutions) at room temperature. After four washes in PBS containing 0.05% Tween-20, the membranes were incubated with goat anti-rabbit IgG antibody for 1 h. The membranes were then washed four times in PBS containing 0.05% Tween-20. The signal was visualized using an enhanced chemiluminescence (ECL) detection kit from Pierce (Pierce Biotechnology, Inc, Rockford, IL, USA). Each band of immunoblotting was scanned, and its intensity was analyzed by Image J software.
Morphological evaluation
For histopathological analysis, liver specimens fixed in 10% neutral-buffered formalin were embedded in paraffin, sliced at 5-μm thickness, and stained with hematoxylin and eosin (HE) to detect the degree of hepatic steatosis and inflammation and necrosis. The pathological changes were assessed and photographed under an Olympus BX-51 microscope. Fatty change was graded according to the percentage of hepatocytes containing macrovesicular fat (grade 1: 0%–25%; grade 2: 26%–50%; grade 3: 51%–75%; grade 4, 76%–100%)24. The degree of inflammation and necrosis was expressed as the mean of 10 different fields within each slide. Each slide was then classified on a scale of 0–3 (0: normal; 1: mild; 2: moderate; 3: severe)25.
For ultrastructural analysis, 1-mm3 samples were fixed in glutaraldehyde (2.5%), post-fixed in osmium tetraoxide (2%) and embedded in Spurr's resin. Sections were stained with uranyl acetate (2%, w/v) and lead citrate prior to analysis with electron microscopy (Zeiss EM 109; Oberkochen, Germany). Morphometric measurement of the mitochondrial surface area was performed on the five largest mitochondria per photograph using an image analysis and measuring system (Image Pro Plus V 5.2)24.
Statistical analysis
Data are expressed as the mean±SD, and the statistical analysis was performed using Student's t-test. The Mann-Whitney rank-sum test was used to analyze the degree of histopathological liver steatosis and inflammation. P<0.05 was considered to be significant.
Results
Serum aminotransferase activities
The rats with NASH induced by a high-fat diet developed hepatic damage as evidenced by the increased serum levels of AST and ALT. The administration of tiopronin significantly reduced the AST and ALT activities compared with the model group, while UDCA only decreased serum ALT levels (Table 1).
Serum and liver lipid metabolism
To investigate the possible role of tiopronin in lipid metabolism, which is the key factor in fatty liver formation, the levels of TG, TC, FFA, HDL-C, and LDL-C were analyzed. As shown in Tables 2 and 3, the increased serum and liver levels of TG, TC, and FFA as well as serum LDL-C levels were significantly suppressed, whereas the decreased serum HDL-C level was obviously elevated by tiopronin treatment in rats fed a high-fat diet. Compared with model group rats, UDCA lowered serum and liver TC levels as well as serum levels of LDL-C but did not change serum levels of TG, FFA, and HDL-C (Tables 2 and 3).
Lipid peroxidation and antioxidative enzyme levels
Oxidative stress has been focused upon as a common pathogenic mechanism in various liver diseases and is considered to play a major role in the pathogenesis of NASH as well1. In Table 4, the antioxidant activities of tiopronin were estimated by measuring the hepatic MDA content and levels of SOD and GSH-Px activity. The high-fat diet increased liver MDA levels but decreased liver levels of SOD and GSH-Px activity compared with those observed in the normal control group. Tiopronin treatment significantly reversed these values. These results suggest that the imbalance between oxidative stress generation and antioxidant formation could occur after rats were fed a high-fat diet. Tiopronin may prevent this pathological process, indicating its therapeutic and preventive effect on NASH induced by the ingestion of a high-fat diet (Table 4).
Histological analysis
Rats fed high-fat diet for 10 weeks not only developed a high degree of hepatic steatosis with severe cytoplasmic vacuoles and swelling of the hepatocytes but also exhibited more prominent inflammation, which was corroborated by morphological evidence of an abundance of inflammatory cells (Figure 1B), whereas no histological abnormalities were observed in normal control rats (Figure 1A). Hepatocyte degeneration and the infiltration of inflammatory cells were all apparently ameliorated in the rats treated with tiopronin (Figure 1C). UDCA treatment did not affect the histological features of the liver (Table 5 and Figure 1D).
Histological images of liver tissues from rats in which steatohepatitis was induced by a high-fat emulsion reveal the anti-steatohepatitis effects of tiopronin. There were no histological abnormalities observed in rats fed a normal diet (A). Rats fed high-fat diet for 10 weeks developed a high degree of steatosis and inflammation (B). Hepatocyte degeneration and the infiltration of inflammatory cells were all apparently ameliorated by tiopronin treatment in rats fed high-fat diet (C). UDCA treatment did not affect the histological features of the liver in the rats fed high-fat diet (D). The magnification is ×400.
Ultrastructural analysis of morphological changes in the mitochondria
Accumulating evidence indicates that mitochondrial dysfunction plays a key role in the physiopathology of NASH26. In this study, mitochondria in the livers of rats fed a high-fat diet exhibited degenerative changes such as mitochondrial swelling, matrix rarefication and cristae loss. These changes were ameliorated by tiopronin and UDCA treatment (Table 5 and Figure 2).
Electron microscopy of hepatic mitochondria. Mitochondria in the rats fed the high-fat emulsion diet showed degenerative changes with mitochondrial swelling, rarefied matrices and cristae loss (B) (arrows). These changes were prominent in most of the mitochondria in the rats fed the high-fat emulsion diet but were rare in the mitochondria in the normal diet-fed rats (A). These changes were also ameliorated by tiopronin (C) and UDCA (D) treatment in the rats fed a high-fat diet. The magnification is ×15 000.
Hepatic CYP2E1 expression
Previous studies showed that alterations of CYP2E1 contributed to NASH27. Therefore, we analyzed the effect of tiopronin on the expression of CYP2E1 in the rat liver with NASH. During the 10 weeks of dietary treatment, mRNA and protein levels of CYP2E1 in the rat liver were significantly increased. In contrast, tiopronin treatment reduced the expression of CYP2E1 in rats fed a high-fat diet (Figures 3 and 4).
The effect of tiopronin on hepatic CYP2E1 mRNA expression in rats fed a high-fat diet. The mRNA levels were normalized to those of β-actin. RT-PCR analysis reveals that the mRNA expression of CYP2E1 was significantly increased in rats fed a high-fat diet. In contrast, tiopronin treatment reduced the expression of CYP2E1 in rats fed a high-fat diet. Data are expressed as the mean±SD (n=6). cP<0.01 vs normal diet. fP<0.01 vs high fat. 1, normal diet; 2, high fat; 3, high fat+tiopronin.
Effect of tiopronin on hepatic CYP2E1 protein expression in rats fed a high-fat diet. The protein was corrected by β-actin. Immunoblot analysis showed that the protein expression of CYP2E1 was significantly increased in rats fed a high-fat diet. In contrast, tiopronin treatment reduced the expression of CYP2E1 in rats fed a high-fat diet. Data are expressed as the mean±SD (n=6). cP<0.01 vs normal diet. fP<0.01 vs high fat.
Discussion
This study reveals that tiopronin, which contains an SH-group and is generally considered an antioxidant, protects against the accumulation of lipid in the rat liver induced by a high-fat diet. The protective effect of tiopronin is mediated through the downregulation of TG, TC, FFA, and LDL-C and the elevation of HDL-C. Histological examination showed that the histological changes associated with liver injury were also remarkably ameliorated after tiopronin treatment. These results demonstrate that tiopronin has protective effects against steatohepatitis induced by a high-fat diet in rats.
Although steatosis represents a form of lipotoxicity, its pathogenesis remains poorly understood. Free fatty acids (FFAs) appear to be important mediators of lipotoxicity, both as potential cellular toxins and by inducing lipid over-accumulation28. Furthermore, FFAs not only promote hepatic lipotoxicity via a lysosomal pathway29 but are also the most important source of reactive oxygen species (ROS)30,31. Some studies suggest that the excessive accumulation of saturated FFAs in liver cells directly induces mitochondrial dysfunction and oxidative stress32. Mitochondrial abnormality plays a role in the onset and progression of NASH in correlation with oxidative stress33. In this study, FFA levels in both the serum and liver were reduced by tiopronin treatment, and mitochondrial morphological changes were also reproduced in rats fed a high-fat diet. These results indicate that tiopronin may be a potential candidate to protect against the steatohepatitis induced by a high-fat diet.
Oxidative stress and alterations in the pro-oxidant-antioxidant balance are commonly implicated as the 'second hit' in the steatotic liver, which promotes the progression from steatosis to steatohepatitis1. The proinflammatory, pro-fibrogenic effects of the aldehyde end-products of lipid peroxidation (MDA and 4-hydroxynonenol) potentially account for all of the typical histological features observed in NAFLD34. It has been shown that MDA, an index of lipid peroxidation and oxidative stress, damages cells and tissues. SOD is responsible for neutralizing the most common free radical, which is known as superoxide. It also aids the body's utilization of copper, zinc and manganese. GSH-Px, along with SOD, is one of the body's endogenous antioxidants and is well known to protect liver cells against oxidative damage through chemical or enzymatic reactions. It has also been reported that tiopronin, like glutathione, is able to protect against ethanol-induced fatty liver by preventing fat accumulation and mitochondrial injury. This increases the proportion of reactive SH groups in the mitochondrial membrane9,11,13. In this study, the markers of oxidative stress included increased hepatic MDA content and decreased levels of SOD and GSH-Px. Tiopronin successfully reversed these changes. These data suggest that the therapeutic effects of tiopronin against steatohepatitis in rats may be associated with preventing the development of oxidative stress and mitochondrial abnormalities.
Although different studies point to the damaged respiratory chain as a main source of mitochondrial ROS in NASH, some data suggest that the ectopic expression of cytochrome P450 2E1 (CYP2E1) in mitochondria could also play a role in ROS overproduction. Previous studies have shown that CYP2E1 is the major catalyst for the formation of lipid peroxides in mice35. CYP2E1 has been shown to play a key role in the pathogenesis of alcoholic liver injury, including alcoholic steatohepatitis36. Its pathogenic role in NASH has also been recognized in both animal experiments and human studies27,37. A recent study has also shown that tiopronin exerts its hepatoprotective activity against isoniazid-induced hepatotoxicity by reducing free radical generation in addition to its role as a scavenger via the inhibition of hepatic CYP2E138. In this study, the protein expression of CYP2E1 was also significantly decreased by tiopronin treatment in rats fed a high-fat diet. To summarize, tiopronin exerts its protective activity against steatohepatitis by preventing oxidative stress through the inhibition of hepatic CYP2E1.
In conclusion, our current investigation for the first time shows that the protective effects of tiopronin on NASH are associated with the regulation of lipid metabolism and the amelioration of mitochondrial abnormalities through the prevention of oxidative stress as well as the inhibition of hepatic CYP2E1 expression. These results have shed some light on the clinical therapeutic potential of tiopronin in treating NASH.
Author contribution
Jun LI, Yu-hong ZOU, and Jian-qing WANG designed research; Jian-qing WANG and Cheng HUANG performed research; Chao LU and Lei ZHANG contributed new reagents or analytic tools; Yong JIN, Xiong-wen LÜ, and Li-ping LIU analyzed data; Jian-qing WANG wrote the paper; and Yu-hong ZOU and Cheng HUANG revised the paper.
References
Day CP, James OF . Steatohepatitis: a tale of two “hits”? Gastroenterology 1998; 114: 842–5.
Te Sligte K, Bourass I, Sels JP, Driessen A, Stockbrugger RW, Koek GH . Non-alcoholic steatohepatitis: review of a growing medical problem. Eur J Intern Med 2004; 15: 10–21.
Huang MA, Greenson JK, Chao C, Anderson L, Peterman D, Jacobson J, et al. One-year intense nutritional counseling results in histological improvement in patients with non-alcoholic steatohepatitis: a pilot study. Am J Gastroenterol 2005; 100: 1072–81.
Stratopoulos C, Papakonstantinou A, Terzis I, Spiliadi C, Dimitriades G, Komesidou V, et al. Changes in liver histology accompanying massive weight loss after gastroplasty for morbid obesity. Obes Surg 2005; 15: 1154–60.
Luyckx FH, Lefebvre PJ, Scheen AJ . Non-alcoholic steatohepatitis: association with obesity and insulin resistance, and influence of weight loss. Diabetes Metab 2000; 26: 98–106.
Dioguardi N, Ideo G, De Franchis R, Ronchi G . Controlled clinical trial of 2-mercapto-propionyl-glycine in chronic hepatopathies. Minerva Med 1976; 67: 676–81.
Ichikawa H, Imaizumi K, Tazawa Y, Obara Y, Ishikawa Y, Tobari I, et al. Effect of tiopronin on senile cataracts. A double-blind clinical study. Ophthalmologica 1980; 180: 293–8.
Sany J, Combe B, Verdie-Petibon D, Tagemouati A, Daures JP . Long-term tolerability of tiopronin (Acadione) in the treatment of rheumatoid arthritis. Apropos of 140 personal cases. Rev Rhum Mal Osteoartic 1990; 57: 105–11.
Ichida F, Shibasaki K, Takino T, Suzuki H, Fujisawa K, Inoue K, et al. Therapeutic effects of tiopronin on chronic hepatitis: a double-blind clinical study. J Int Med Res 1982; 10: 325–32.
Kim ES, Glisson BS . Treatment of metastatic head and neck cancer: chemotherapy and novel agents. Cancer Treat Res 2003; 114: 295–314.
Hirayama C, Kishimoto Y, Wakushima T, Murawaki Y . Mechanism of the protective action of thiol compounds in ethanol-induced liver injury. Biochem Pharmacol 1983; 32: 321–5.
Yilong C . Clinical evaluation on the effect of tiopronin in nonalcoholic steatohepatitis. China Modern Doctor 2008; 46: 37–8.
Surrenti C, Arcangeli A, Casini A . The antisteatosic activity of 2-MPG (Thiola). Study with the (BSF) dynamic test and with liver biopsy before and after the treatment. Minerva Med 1978; 69: 4251–6.
Ljubuncic P, Tanne Z, Bomzon A . Ursodeoxycholic acid suppresses extent of lipid peroxidation in diseased liver in experimental cholestatic liver disease. Dig Dis Sci 2000; 45: 1921–8.
Buko VU, Lukivskaya OY, Zavodnik LV, Sadovnichy VV, Petushok NE, Tauschel ND . Antioxidative effect of ursodeoxycholic acid in the liver of rats with oxidative stress caused by gamma-irradiation. Ukr Biokhim Zh 2002; 74: 88–92.
Chang CY, Argo CK, Al-Osaimi AM, Caldwell SH . Therapy of NAFLD: antioxidants and cytoprotective agents. J Clin Gastroenterol 2006; 40: S51–60.
Balmer ML, Siegrist K, Zimmermann A, Dufour JF . Effects of ursodeoxycholic acid in combination with vitamin E on adipokines and apoptosis in patients with nonalcoholic steatohepatitis. Liver Int 2009; 29: 1184–8.
Georgescu EF, Georgescu M . Therapeutic options in non-alcoholic steatohepatitis (NASH). Are all agents alike? Results of a preliminary study. J Gastrointestin Liver Dis 2007; 16: 39–46.
Laurin J, Lindor KD, Crippin JS, Gossard A, Gores GJ, Ludwig J, et al. Ursodeoxycholic acid or clofibrate in the treatment of non-alcohol-induced steatohepatitis: a pilot study. Hepatology 1996; 23: 1464–7.
Dufour JF, Oneta CM, Gonvers JJ, Bihl F, Cerny A, Cereda JM, et al. Randomized placebo-controlled trial of ursodeoxycholic acid with vitamine in nonalcoholic steatohepatitis. Clin Gastroenterol Hepatol 2006; 4: 1537–43.
Fan JG, Zhong L, Tia LY, Xu ZJ, Li MS, Wang GL . Effects of ursodeoxycholic acid and/or low-calorie diet on steatohepatitis in rats with obesity and hyperlipidemia. World J Gastroenterol 2005; 11: 2346–50.
Zou Y, Li J, Lu C, Wang J, Ge J, Huang Y, et al. High-fat emulsion-induced rat model of nonalcoholic steatohepatitis. Life Sci 2006; 79: 1100–7.
Folch J, Lees M, Sloane Stanley GH . A simple method for the isolation and purification of total lipides from animal tissues. J Biol Chem 1957; 226: 497–509.
Kirsch R, Clarkson V, Shephard EG, Marais DA, Jaffer MA, Woodburne VE, et al. Rodent nutritional model of non-alcoholic steatohepatitis: species, strain and sex difference studies. J Gastroenterol Hepatol 2003; 18: 1272–82.
Avni Y, Shirin H, Aeed H, Shahmurov M, Birkenfeld S, Bruck R . Thioacetamide-induced hepatic damage in a rat nutritional model of steatohepatitis. Hepatol Res 2004; 30: 141–7.
Begriche K, Igoudjil A, Pessayre D, Fromenty B . Mitochondrial dysfunction in NASH: causes, consequences and possible means to prevent it. Mitochondrion 2006; 6: 1–28.
Weltman MD, Farrell GC, Liddle C . Increased hepatocyte CYP2E1 expression in a rat nutritional model of hepatic steatosis with inflammation. Gastroenterology 1996; 111: 1645–53.
Mavrelis PG, Ammon HV, Gleysteen JJ, Komorowski RA, Charaf UK . Hepatic free fatty acids in alcoholic liver disease and morbid obesity. Hepatology 1983; 3: 226–31.
Feldstein AE, Werneburg NW, Canbay A, Guicciardi ME, Bronk SF, Rydzewski R, et al. Free fatty acids promote hepatic lipotoxicity by stimulating TNF-alpha expression via a lysosomal pathway. Hepatology 2004; 40: 185–94.
Halliwell B . Free radicals, antioxidants, and human disease: curiosity, cause, or consequence? Lancet 1994; 344: 721–4.
Morris AA . Mitochondrial respiratory chain disorders and the liver. Liver 1999; 19: 357–68.
Li Z, Berk M, McIntyre TM, Gores GJ, Feldstein AE . The lysosomal-mitochondrial axis in free fatty acid-induced hepatic lipotoxicity. Hepatology 2008; 47: 1495–503.
Kojima H, Sakurai S, Uemura M, Fukui H, Morimoto H, Tamagawa Y . Mitochondrial abnormality and oxidative stress in nonalcoholic steatohepatitis. Alcohol Clin Exp Res 2007; 31: S61–6.
Uzun MA, Koksal N, Kadioglu H, Gunerhan Y, Aktas S, Dursun N, et al. Effects of N-acetylcysteine on regeneration following partial hepatectomy in rats with nonalcoholic fatty liver disease. Surg Today 2009; 39: 592–7.
Leclercq IA, Farrell GC, Field J, Bell DR, Gonzalez FJ, Robertson GR . CYP2E1 and CYP4A as microsomal catalysts of lipid peroxides in murine nonalcoholic steatohepatitis. J Clin Invest 2000; 105: 1067–75.
Lieber CS . Cytochrome P-4502E1: its physiological and pathological role. Physiol Rev 1997; 77: 517–44.
Chalasani N, Gorski JC, Asghar MS, Asghar A, Foresman B, Hall SD, et al. Hepatic cytochrome P450 2E1 activity in nondiabetic patients with nonalcoholic steatohepatitis. Hepatology 2003; 37: 544–50.
Yue J, Dong G, He C, Chen J, Liu Y, Peng R . Protective effects of thiopronin against isoniazid-induced hepatotoxicity in rats. Toxicology 2009; 264: 185–91.
Acknowledgements
The research presented in this paper was financially supported by the National Natural Science Foundation of China (No 30873081 and 81072686) and Natural Science Foundation of Anhui Province (No 1208085QH143).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Wang, Jq., Zou, Yh., Huang, C. et al. Protective effects of tiopronin against high fat diet-induced non-alcoholic steatohepatitis in rats. Acta Pharmacol Sin 33, 791–797 (2012). https://doi.org/10.1038/aps.2012.19
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2012.19
Keywords
This article is cited by
-
Evaluate the value of prolonging the duration of tiopronin for injection administration in preventing hepatotoxicity
Scientific Reports (2024)
-
Allisartan isoproxil reduces mortality of stroke-prone rats and protects against cerebrovascular, cardiac, and aortic damage
Acta Pharmacologica Sinica (2021)
-
Prospective analysis of tiopronin in prevention of sorafenib and antiviral therapy inducing liver toxicity in advanced hepatitis B virus-related hepatocellular carcinoma
Medical Oncology (2015)