Abstract
Aim:
To investigate the in vitro and in vivo percutaneous absorption of seleno-L-methionine (Se-L-M), an ultraviolet (UV)-protecting agent, from aqueous solutions.
Methods:
Aqueous solutions of Se-L-M were prepared in pH 4, 8, and 10.8 buffers. The pH 8 buffer contained 30% glycerol, propylene glycol (PG) and polyethylene glycol (PEG) 400. The in vitro skin permeation of Se-L-M via porcine skin and nude mouse skin was measured and compared using Franz diffusion cells. The in vivo skin tolerance study was performed, which examined transepidermal water loss (TEWL), skin pH and erythema.
Results:
In the excised porcine skin, the flux was 0.1, 11.4 and 8.2 μg·cm−2·h−1 for the pH 4, 8, and 10.8 buffers, respectively. A linear correlation between the flux and skin deposition was determined. According to permeation across skin with different treatments (stripping, delipidation, and ethanol treatments), it was determined that the intracellular route comprised the predominant pathway for Se-L-M permeation from pH 8 buffer. Aqueous solutions of seleno-DL-methionine (Se-DL-M), selenium sulfide and selenium-containing quantum dot nanoparticles were also used as donor systems. The DL form showed a lower flux (7.0 vs 11.4 μg·cm−2·h−1) and skin uptake (23.4 vs 47.3 μg/g) as compared to the L form, indicating stereoselective permeation of this compound. There was no or only negligible permeation of selenium sulfide and quantum dots into and across the skin. With in vivo topical application for 4 and 8 h, the skin deposition of Se-L-M was about 7 μg/g, and values were comparable to each other. The topical application of Se-L-M for up to 5 d did not caused apparent skin irritation. However, slight inflammation of the dermis was noted according to the histopathological examination.
Conclusion:
Se-L-M was readily absorbed by the skin in both the in vitro and in vivo experiments. The established profiles of Se-L-M skin absorption will be helpful in developing topical products of this compound.
Similar content being viewed by others
Introduction
Skin is constantly exposed to prooxidant environmental stresses from an array of sources, such as air pollutants, solar ultraviolet (UV) light, chemical oxidants, microorganisms, and ozone1. Reactive oxygen species (ROS) were implicated in the etiology of several skin disorders including skin cancer and photoaging. Skin cancer constitutes about 30% of all newly diagnosed cancers in the world and solar UV radiation, particularly the UVB component, is an established cause of about 90% of skin cancers2. In recent years, particular antioxidants have gained considerable attention as means of neutralizing ROS. This group includes vitamins (C and E), phytochemicals (carotenoids and polyphenols), and minerals (zinc and selenium)3. There is much evidence to suggest that selenium has an important role in protecting skin from the harmful effects of UVB. Selenium, an essential trace element, is found in many foods, including meat, fish, eggs, dairy products, and grains4. The UVB protection afforded by selenium compounds is attributed to their ability to increase activities of glutathione peroxidase and thioredoxin reductase which are antioxidant selenoenzymes5. In humans, a low selenium status is associated with up to a 4-fold increased risk of developing skin cancer6. Topical selenium compounds also increase the minimum dose of UV radiation required to cause skin reddening and protect against skin damage caused by UVB7, 8. Seleno-L-methionine (Se-L-M), the major component of dietary selenium, represents an organic form of selenium which may provide enhanced protection of the skin9. Se-L-M also decreases the oxidative stress of neurodegenerative diseases, rheumatoid arthritis, and HIV/AIDS10, 11.
Most ingested selenium, whether in organic or inorganic form, is converted by liver metabolism3. In addition, selenium toxicity can produce gastrointestinal problems12. Delivery of pharmacologically active compounds via the skin is an attractive alternative to oral dosing for numerous reasons including stable plasma concentrations, bypass of first-pass effects, and reduction of some side effects13, 14. Topical delivery via the skin may provide direct selenium targeting to attain sufficient activity for skin prevention/therapy. Topical administration may also be a suitable route for selenium to achieve systemic bioavailability to maintain daily necessities and treat systemic disorders.
No evidence currently exists to support the notion that significant amounts of Se-L-M can be delivered into and across the skin. The number of specific metals that was investigated for skin permeation is also limited15. The aim of this work was to establish skin permeation profiles of Se-L-M from various vehicles. The permeation via the skin of other selenium species, such as seleno-DL-methionine (Se-DL-M), selenium sulfide (SeS2), and cadmium selenium (CdSe) quantum dots was also evaluated. Both in vitro and in vivo skin absorption experiments were performed in this study. To study the in vitro potential of these compounds, a permeation study was performed with Franz diffusion cells using excised porcine and nude mouse skin. The optimal pH and type of vehicles for better absorption of Se-L-M were investigated. Possible pathways of this antioxidant via the skin were elucidated using porcine skin treated by stripping, delipidation, oleic acid, and α-terpineol to indicate the specific routes of skin absorption. Possible skin irritation of Se-L-M was studied by histopathology and in vivo bioengineering techniques using nude mice as the animal model.
Materials and methods
Materials
Se-L-M, Se-DL-M, selenium sulfide, Lumidot™ CdSe quantum dots, Lumidot™ CdSe/ZnS quantum dots, oleic acid, and α-terpineol were purchased from Sigma-Aldrich (St Louis, MO, USA). Cellulose membranes with a molecular weight (Mw) cutoff of 3500 (Spectra Por™ 3) were supplied by Spectrum Laboratories (Rancho Dominguez, CA, USA). All other chemicals and solvents were of analytical grade and were used as received.
Animals
Specific pathogen-free (SPF) pigs (1 week old) were supplied by the Animal Technology Institute Taiwan (Miaoli, Taiwan, China). Female nude mice (8 weeks old) were obtained from the National Laboratory Animal Center (Taipei, Taiwan, China). The animal experiment protocol was reviewed and approved by the Institutional Animal Care and Use Committee of Chang Gung University. Animals were housed and handled according to institutional guidelines.
Preparation of skin membranes
Full-thickness skin was excised from the dorsal region of pigs and mice. Subcutaneous fat, tissues, blood vessels, and epidermal hairs were carefully removed before use. The skin was stripped 20 times with adhesive tape in the study to obtain stratum corneum (SC)-stripped skin. To obtain delipidized skin, the SC side was pretreated with chloroform-methanol (2:1) for 2 h. Five percent oleic acid or α-terpineol in a 25% ethanol/water medium was used to pretreat the skin mounted on a Franz cell for 2 h before the in vitro skin permeation experiment.
In vitro skin permeation
Porcine or nude mouse skin with or without pretreatment was mounted on the receptor compartment of a Franz cell with the SC side facing upwards into the donor compartment. The receptor was filled with 5.5 mL of pH 7.4 citrate-phosphate buffer, and maintained at 37 °C under constant stirring. The donor compartment was occluded by parafilm and filled with 0.5 mL of vehicle containing Se-L-M or other selenium species at determined concentrations. The available diffusion area between the compartments was 0.79 cm2. At appropriate intervals, 300-μL aliquots of the receptor medium were withdrawn and immediately replaced with an equal volume of fresh medium.
At the end of the in vitro experiment (24 h), the skin was removed from the cell and the skin surface was cleaned with a cotton wool swab immersed in water and methanol three times each for removing any contaminent. The skin was weighed, cut with scissors, positioned in a glass homogenizer containing 1 mL of 0.1 mol/L HCl, and homogenized for 10 min at 300 revolutions per minute. The resulting solution was centrifuged for 10 min at 10 000 revolutions per minute and then filtered through a polyvinylidene difluoride membrane with a pore size of 0.45 μm. All samples were analyzed by graphite furnace atomic absorption spectrophotometry (Z-5000, Hitachi, Tokyo, Japan). The wavelength set for selenium was 196 nm. At the range 0–40 μg/L, the concentration of selenium was linearly proportional to its absorbance. The limit of detection (LOD) of selenium was determined to be 3 μg/L. The intra- and inter-assay precision and accuracy values were evaluated at the concentration range 0–40 μg/L. The overall precision, defined by the relative standard deviation (RSD), ranged from 0.4% to 3.1% on average. Analytical accuracy, expressed as the percentage difference between the mean of measured value and the known concentration, varied from -3.3% to 2.1%.
In vivo skin permeation
Nude mice were used as the animal model in the in vivo experiment. All animals were starved overnight prior to the experiment. A glass cylinder with an available area of 0.79 cm2 was placed on the dorsal skin with glue (Instant Super Glue™, Kokuyo, Tokyo, Japan). An aliquot of 0.2 mL of pH 8 citrate-phosphate buffer with Se-L-M at a concentration of 0.2% (w/v) was added to the cylinder. The application times of the vehicle were 4 and 8 h. The procedures for washing and extraction of the compound from the skin were the same as for the in vitro experiment.
In vivo skin tolerance test
A 0.6-mL aliquot of pH 8 buffer with 0.2% or 0.3% Se-L-M was uniformly spread over a sheet of non-woven polyethylene cloth (1.5 cm×1.5 cm), which was then applied to the back area of a nude mouse. The polyethylene cloth was fixed with Tegaderm™ adhesive dressing (3M, St Paul, MN, USA) and Fixomull™ stretch adhesive tape (Beiersdorf AG, Hamburg, Germany). After 24 h, the cloth was removed, and the treated skin area was swabbed clean with a cotton wool swab. The vehicle was applied daily for 5 d. After withdrawal of the vehicle, transepidermal water loss (TEWL), colorimetric parameters, and the pH of the applied skin were measured. These measurements were evaluated daily. TEWL was recorded using a Tewameter™ (TM300, Courage and Khazaka, Köln, Germany). Measurements taken at a stable level were performed 30 s after application of the TEWL probe to the skin. TEWL was automatically calculated and expressed in g·m−2·h−1. The skin-surface pH was determined by a Skin-pH-Meter™ PH905 (Courage and Khazaka). A spectrocolorimeter (CD100, Yokogawa Electrical, Tokyo, Japan) was used to measure the skin erythema (a*) according to recommendations of the Commission Internationale de l'Eclarirage (CIE). When recording color values, the measuring head was held perpendicular to the back skin. The reading was obtained within a few seconds on the display. The temperature and relative humidity in the laboratory were kept at 26 °C and 55%, respectively. The sample number for each experiment was six.
Histopathological examination
The dorsal skin of nude mouse was excised after topical administration of pH 8 buffer with 0.2% or 0.3% Se-L-M for 5 d. Each skin specimen was dehydrated using ethanol, embedded in paraffin wax, and stained with hematoxylin and eosin. For each skin sample, three different sites were examined and evaluated under light microscopy (Eclipse 4000, Nikon, Tokyo, Japan). Digital photomicrographs were then processed with Adobe PhotoDeluxe (Adobe Systems, San Jose, CA, USA).
Statistical analysis
Statistical analyses of differences between the various treatments were performed using an unpaired Student's t-test. A 0.05 level of probability (P<0.05) was taken as the level of significance. An analysis of variance (ANOVA) test was also used if necessary.
Results
Optimization of vehicles for in vitro skin permeation of Se-L-M
Optimization of topical drug bioavailability is an essential objective for the effective treatment of skin disorders. The pH and composition of vehicles, and the applied dose were shown to be major variables influencing the diffusivity of permeants. The effects of the pH 4–10.8 buffers on skin permeation of Se-L-M were examined. Se-L-M is an amino acid containing selenium. According to the dissociation constant (pKa) values of Se-L-M (2.19 and 9.05)16, this compound is mainly in cationic, zwitterionic, and anionic forms at pH 4, 8, and 10.8, respectively. The solubility of Se-L-M in water is up to 1000 mg/mL, which can be associated with a risk of local toxicity if applied topically. The finite dose technique was applied in this study, although the maximal thermodynamic activity could not be obtained. All donor samples for testing the pH effect were prepared by dispersing 0.2% Se-L-M in buffer. Figure 1 shows the permeation profiles of Se-L-M across porcine skin and nude mouse skin as the means and standard deviations plotted against time. The flux value (μg·cm−2·h−1) is equal to the slope of the linear permeation profile and was calculated from the experimental curves shown in Figure 1. Table 1 summarizes the Se-L-M flux from various buffer solutions. A zero-order equation was suitable for use with the curves of most formulations, except the results of pH 8 buffer via nude mouse skin.
The pH of the vehicle had a significant effect on the transport of Se-L-M. As shown in Figure 1A, the permeability across porcine skin increased in the order of pH 8>pH 10.8>pH 4. The same trends were detected for both porcine and nude mouse skin (Figure 1A vs 1B). Based on the flux values shown in Table 1, the difference between pH 8 and 10.8 was not significant (P>0.05) according to a t-test in the case of porcine skin. For topical bioavailability purposes, the permeant retained in the strata of the skin should be included. Only considering the permeant flux reaching the receptor compartment may underestimate the true level of skin absorption. The skin deposition of Se-L-M by in vitro topical application is depicted in Table 1. The skin with no treatment (blank control) showed no selenium content above the detection limit of atomic absorption. A correlation was noted between porcine skin retention and the flux. A t-test revealed that there was no statistically significant difference (P>0.05) in the skin accumulation between pH 8 and 10.8 buffers in porcine skin. Se-L-M accumulation within nude mouse skin was greatest with the pH 8 buffer and least from the pH 4 buffer.
Table 2 summarizes the permeation data of Se-L-M from pH 8 buffer with 30% organic solvents of glycerol, PG, and PEG400. Porcine skin was used as the permeation barrier. The permeation of Se-L-M from the buffer containing the organic solvents was significantly lower (P<0.05) compared to the neat pH 8 buffer. The flux and skin reservoir of Se-L-M from pH 8 buffer were greater than those from the buffer with organic solvents by 2.5–5-fold. The general trend for the flux was PG>glycerol≥PEG400. There was no significant difference (P>0.05) among the skin deposition levels of the compound from the three vehicles.
The Se-L-M flux and skin deposition from pH 8 buffer with different doses of 0.05%–0.3% are respectively shown in Figure 2A and 2B. A linear correlation (r=0.9748) was apparent between the dose and flux across porcine skin. No significant difference (P>0.05) in the flux was observed between the doses of 0.2% and 0.3%. A linear relationship was not observed in nude mouse skin since a lower flux (P<0.05) was detected in the formulation with the 0.3% compound compared to that with 0.1% and 0.2%. As depicted in Figure 2B, the porcine skin reservoir generally increased with an increase in the Se-L-M dose except at 0.3%. A correlation of r=0.7858 was observed between the dose and porcine skin deposition. The same as the permeant flux via nude mouse skin, the skin deposition from the donor with 0.3% was relatively lower compared to that with 0.2% (P<0.05).
In vitro skin permeation of Se-L-M via various skin types
In order to elucidate the mechanisms involved in the skin permeation of Se-L-M, in vitro permeation experiments to examine the cumulative amount in the receptor were performed using various skin membranes. Although an examination of permeation across skin is less advantageous when targeting skin tissue, an understanding of the permeability is helpful in exploring the mechanisms or pathways of skin absorption. Figure 3 shows the cumulative amount–time profiles of Se-L-M from pH 4, 8, and 10.8 buffers via different skin types. Se-L-M diffusion across the cellulose membrane was determined to evaluate release rates from the buffers. The results indicated that the release of the permeant was faster than permeation across porcine skin. The release kinetics showed an initial burst (0–4 h), followed by a sustained burst (4–8 h), and a plateau (8–24 h). This trend and the level of release were similar for all buffers tested. Among the permeation curves, Se-L-M permeation across SC-stripped skin mostly approximated the data across the cellulose membrane, followed by delipidized skin and intact skin. According to the cumulative amount at 24 h (the end of the experiment), Se-L-M permeation across stripped skin was 158-, 1.7-, and 2.0-fold greater (P<0.05) than that across intact skin from pH 4, 8, and 10.8 buffers, respectively.
To further explore the permeation mechanisms, 3% oleic acid and α-terpineol in 25% ethanol/pH 7.4 buffer were used to pretreat porcine skin. Ethanol at 25% was used as the pretreatment medium for solubility considerations of oleic acid and α-terpineol. As shown in Figure 3B, pretreatment with 25% ethanol significantly reduced (P<0.05) Se-L-M permeation by 2-fold compared to intact skin. Treatment with oleic acid slightly but significantly increased (P<0.05) the cumulative amount over the 25% ethanol-treated group. On the other hand, pretreatment of the skin with α-terpineol did not further increase (P>0.05) permeation.
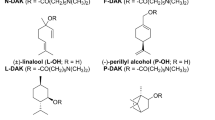
In vitro skin permeation of different selenium species
The skin delivery of other selenium species was also studied in the present work. These included Se-DL-M, selenium sulfide, and CdSe quantum dots. The flux and skin deposition of the selenium compounds are given in Table 3. The enantioselective transfer of selenomethionine via porcine skin was studied. Both the flux and skin deposition of Se-L-M increased more than those of Se-DL-M (P<0.05). From this, it is clear that the L form can pass more easily through the skin barrier than the DL form. This trend was especially significant with skin deposition since the L form showed 2-fold higher skin uptake than the DL form. Selenium sulfide could not pass across the skin into the receptor with a 24-h application. An in vitro uptake of 0.36 μg/g of selenium sulfide was found within the skin. The skin absorption of two types of quantum dots, CdSe and CdSe/ZnS, was tested. No selenium was detected in either the skin reservoir or receptor as shown in Table 3.
In vivo skin permeation of Se-L-M
Levels of Se-L-M in the skin were determined following a single application of pH 8 buffer to the dorsal surface of nude mice. In vivo percutaneous absorption was evaluated using nude mice because they are easy to handle. Table 4 shows the in vivo skin deposition of Se-L-M after topical delivery for 4 and 8 h. Skin uptake of the compound exhibited values of 7.8 and 7.2 μg/g, respectively. There was no significant difference (P>0.05) between the intradermal concentrations of Se-L-M at 4 and 8 h.
Bioengineering methods such as TEWL, pH, and colorimetry were conducted in vivo to evaluate the preliminary safety of Se-L-M on skin. pH 8 buffer containing 0.2% and 0.3% Se-L-M was applied to the dorsal skin of nude mice for 24 h. The total duration of application was 5 d. Values of TEWL, pH, and erythema (a*) were determined every day as shown in Figure 4. Compared to the control group (pH 8 buffer without Se-L-M), no enhancement of TEWL and pH values was observed after application of Se-L-M for 5 d (Figure 4A, 4B). The same result was detected for skin erythema after topical Se-L-M delivery (Figure 4C). This suggests tolerable changes in the skin with topically applied Se-L-M. No visible disruption of the skin was observed at any point during this study of nude mice receiving Se-L-M.
Possible skin irritation by Se-L-M after 5 d of exposure was histologically investigated as shown in Figure 5. Light microscopy indicated no observable damage to intact skin in the untreated group (Figure 5A). Histopathologic analysis of skin samples isolated from the area treated with 0.2% Se-L-M revealed some chronic inflammatory cells such as macrophages and lymphocytes in the dermis (Figure 5B). A partial loss of the SC was exhibited with this dose. When the dose was increased from 0.2% to 0.3%, less significant inflammation was seen in the dermis and subcutis (Figure 5C). Some disarray and disarrangement of the SC were observed. Histological changes to the skin due to treatment with Se-L-M were generally mild.
Discussion
Cumulative and prolonged exposure to UVB is now known to induce deleterious reactions in human skin, including cutaneous aging, immunosuppression, photo-carcinogenesis, and various inflammatory skin disorders17. Supplying topical exogenous antioxidants to the skin can prevent or minimize UVB-induced damage18. Despite various reports linking many of the beneficial properties of selenium to its use, no comprehensive study has been conducted to investigate the skin absorptive ability of related compounds. Moreover, penetration of the skin still needs to be separately determined for each metal species because of the large diversity permeation characteristics of various metal via the skin15. The present results showed that Se-L-M exhibited considerable absorption into the skin, especially with pH 8 buffer. The preliminary safety of Se-L-M to the skin was also evaluated. The results showed negligible irritation of the skin after in vivo topical administration, suggesting its feasibility for dermal use.
Porcine skin was initially used as the permeation barrier in this study because of its similarity to human skin. The skin of rodents is most commonly used for in vitro and in vivo skin permeation studies. There are a number of hairless species (eg, nude mice and hairless rats) in which the absence of a hairy coat mimics human skin better than hairy skin19. Hence nude mice were also utilized as an animal model in this study. The experimental results showed similar flux values between nude mouse skin and porcine skin in our case. This suggests that nude mice can be a successful model for evaluating the skin permeation of selenium compounds. Se-L-M in the buffers with higher pH values was found to penetrate more easily into and through the skin. The accumulation of a compound within the skin reflects the skin deposition after topical application. On the other hand, the concentration of a compound received in the Franz cell predicts the amount distributed to plasma or other organs in an in vivo status20. Both parameters were meaningful for Se-L-M. This selenium compound can prevent or treat UVB-related disorders in skin. The essential uptake for systemic levels of selenium in daily life was also achieved by a transdermal route.
Skin absorption of a permeant is determined by its physicochemical characteristics, in particular, its Mw and lipophilicity, which play major roles in the skin permeation process. Finnin and Morgan21 indicated that molecules with a Mw of <500 Da can penetrate across the skin because of their small molecular volumes. Se-L-M fits this criterion (Mw 196.1 Da). Poor absorption is more likely when the octanol/water partition coefficient (logP) is >5 or <-117. Se-L-M showed a logP of -3.0122, which does not fulfill the criterion. This can explain the extremely low permeation of Se-L-M from pH 4 buffer. However, Se-L-M still demonstrated a considerable penetration in pH 8 and 10.8 buffers. Se-L-M is predominantly in a zwitterion form in pH 8 buffer, which is beneficial due to its lipophilicity. The neutral form of a compound always shows higher skin partitioning compared to the ionic form because of the lipophilic characteristics of the SC23, 24. The present findings suggest that the corresponding anions at pH 10.8 also showed high skin permeation. Increased pH can ionize a greater part of the intercellular fatty acids, changing the phase behavior and packing of the barrier lipid mixture25. The SC may be much more permeable to molecules in an alkaline vehicle15. This effect was not observed below pH 9 since the evidence indicates buffers at pH<9 did not compromise the barrier function26.
A direct correlation between the skin deposition and flux was achieved for all Se-L-M formulations tested. The higher skin reservoir of the compound may result in high release into the receptor compartment because of the rapid diffusion due to the concentration gradient24. However, differences in skin deposition among formulations were smaller compared to those of flux values. For example, pH 8 buffer exhibited a 9-fold increase in skin deposition over pH 4 buffer, whereas a 127-fold increase was detected for the flux. The electrophilic nature of many metals determines their protein reactivity, which can result in depot formation in the SC15, 27. Se-L-M was found to replace methionine when incorporated into proteins16, resulting in an abundance in the skin reservoir. A previous study28 suggested that protection from UVB-radiation-induced human skin cell death can be obtained with concentrations of as low as 10 nmol/L with Se-L-M. This value can be calculated as 0.002 ng/g, a level that simulates skin deposition. Se-L-M showed skin deposition which was much greater than the minimum concentration for inducing protection efficiency.
The incorporation of an organic solvent such as glycerol, PG, or PEG400 in pH 8 buffer significantly reduced the permeation of Se-L-M. The addition of an organic solvent may have reduced the polarity of the aqueous vehicle as the solvent is relatively lipophilic. The decreased polarity with organic solvent incorporation in the vehicle hinders the partitioning of the permeant into the SC29, 30. Another explanation may be the higher viscosity of these solvents relative to the aqueous solution, making it difficult for the permeant to diffuse within the oil system. The data clearly showed an increased flux with PG compared to glycerol and PEG400. The permeation process is generally referred to as the drag-effect and may explain the effect of PG31, 32. Such data may indicate a polar route of delivery for Se-L-M.
It can be seen that the permeation of Se-L-M was not commensurate with the applied concentration. A 0.3% dose did not further increase the flux or skin deposition via porcine skin compared to a lower dose (0.2%). This can be interpreted as a saturation of the skin reservoir by the selenium compound. A dose of 0.3% Se-L-M even showed reduced permeation via nude mouse skin. This phenomenon is commonly observed with the skin delivery of metals. This is due to the buildup of a secondary diffusion barrier as a consequence of metals forming stable bonds with proteins of the skin15. In this way, a depot accumulates in the SC retarding further penetration in inverse proportion to the metal concentration. This effect may have been more pronounced for nude mouse skin than porcine skin.
With respect to drug permeation via the skin from the vehicle, a permeant should first diffuse out of the vehicle onto the skin surface. The release rate of Se-L-M across the cellulose membrane was significantly higher than that across porcine skin. This indicates that the skin exerted a significant barrier function against the transport of Se-L-M. The release profiles from various buffer systems approximated each other. Since a large discrepancy of skin penetration existed among the various buffers, the partitioning or permeation process via skin but not the release process was the rate-limiting step for Se-L-M. Tape stripping is a simple standard technique for evaluating the function of the SC in percutaneous absorption studies33. Se-L-M in pH 4 buffer showed the highest enhancement of skin permeation across SC-stripped skin compared to the other buffer systems, suggesting that diffusion through the SC layer was important for permeation in a cationic form. Se-L-M permeation across stripped skin did not achieve the level of release across the cellulose membrane by the end of the experiment (24 h). This suggests that permeation was hindered by the SC, and the viable epidermis/dermis beneath the SC may have contributed to the aqueous resistance to its diffusion. The epidermal-dermal tight junction is an example of an important barrier for some materials34. This phenomenon was not observed for Se-L-M at pH 8 and 10.8 since the cumulative Se-L-M amount via stripped skin approximated the release amount at the end of the experiment.
Permeation through corneocytes (a transcellular pathway) and permeation through the lipid bilayers surrounding the corneocytes (an intercellular pathway) contribute to the routes of drug permeation across the SC. Delipidation greatly increased the skin permeation of Se-L-M at pH 4 compared to intact skin. This suggests that the intercellular lipid bilayers were the main barrier blocking the transit of Se-L-M in an acidic environment. The penetration rates of this compound via delipidized skin and intact skin were comparable in neutral and alkaline environments (pH 8 and 10.8). This indicates that the presence of lipid bilayers did not greatly influence the penetration of this selenium compound at these pH values. Intracellular or transappendageal routes may be pathways for Se-L-M delivery at pH 8 and 10.8. This result is in accordance with permeation from PG-containing vehicles. The penetration pathways of Se-L-M in pH 8 buffer were further investigated using ethanol, oleic acid, and α-terpineol as pretreatment media for the skin. Pretreatment with 25% ethanol resulted in a retardation of Se-L-M permeation. Changes in the skin's structure induced by ethanol reduced the delivery of some drugs24, 35. Protein denaturation in the SC may have been involved in this reduction. This result verified that the hydrophilic pathways through corneocytes can play an important role in the skin delivery of Se-L-M.
Oleic acid and α-terpineol were used as permeation enhancers for dermal/transdermal drug delivery. Oleic acid acts on the lipidic tail portion of intercellular lipid bilayers, while α-terpineol is known to act on the lipid polar heads of ceramides36. Oleic acid produced enhancement of the skin permeation of Se-L-M compared to the 25% ethanol-treated group. This suggests that the alkyl chain of the lipids could act as a barrier hindering permeation. It also confirms that the intracellular route may be essential for Se-L-M, since oleic acid can disrupt corneocytes37. Pretreatment with α-terpineol did not enhance the activity of Se-L-M permeation. This may indicate that hydrogen bonds between ceramides are not important for Se-L-M penetration across the SC.
Both inorganic and organic forms of selenium are commonly used for therapeutic and diagnostic purposes. The experimental results indicated that molecular stereochemical complexity can predominate the skin delivery of compounds. The in vitro skin permeation experiments demonstrated that the diffusion of the L and DL forms via porcine skin was stereoselective, with the L form showing higher permeation. This indicates that the SC contributed to the barrier function against percutaneous absorption of the D form. Since intracellular pathways were the predominant route for selenomethionine delivery, corneocytes may produce qualitative evidence of stereoselective interaction. This chiral interaction can cause differences in diffusion rates via the skin. Se-L-M may favor this interaction compared to the D form. According to previous studies involving the skin delivery of enantiomers38, 39, 40, the L form (or S form) of ketorolac, ketoprofen, and selegiline also exhibited greater skin absorption than the D form (or R form).
Topical preparations containing selenium sulfide are frequently used to manage tinea versicolor, seborrheic dermatitis, and dandruff41, 42. It is commonly incorporated into shampoo for treating dandruff. Our results showed that the skin was virtually impermeable to selenium sulfide. Only a very low amount of selenium sulfide was retained in the skin reservoir. This is accordance with a previous study which found that selenium sulfide in shampoo is not absorbed by the skin43.
Quantum dot nanoparticles have received attention due to their fluorescent characteristics and potential use in medical applications34, 44. Because the skin is the main target tissue for nanoparticle exposure, assessment of the skin penetration of quantum dots has attracted a great deal of attention. A recent development is utilization of selenium as a material for quantum dot preparations. The core of quantum dots consists of cadmium and selenium (CdSe), sometimes with a shell of ZnS to make them biologically compatible. Whether the quantum dots can permeate the skin is controversial. Recent investigations reported that skin penetration by quantum dots did not occur in intact mouse skin45, was minimal in a murine model46, and was detected in the lower SC layer of a human skin equivalent47. In our case, neither CdSe nor CdSe/ZnS quantum dots were absorbed by porcine skin. No or only negligible amounts in the receptor and skin reservoir were detected by analyzing selenium. This suggests that the shell of quantum dots was not damaged, and the CdSe core did not leach out. Penetration of quantum dots into the epidermal layers can result in a localized skin response, such as inflammation or cytotoxicity26. Cadmium and selenium are two components of the core that are known to be toxic to cells34. Our results indicated that quantum dots with a diameter of 6 nm may be safe for topical administration to skin tissue.
The electrophilic nature of many metals determines their protein interactions, which can result in depot formation in the skin. The in vivo skin uptake of Se-L-M was hence determined. The level of the in vivo skin reservoir was less than that in an in vitro condition. This was due to the significant diffusion and distribution of permeants from the skin to the systemic circulation or other tissues after in vivo topical administration, thus reducing the skin accumulation in an in vivo status. No significant difference in Se-L-M skin levels was observed between 4 and 8 h of administration. This can be explained by saturation of the skin reservoir. Another reason for the lower uptake of in vivo permeation was the shorter exposure time during the in vivo experiment compared to the in vitro experiment (24 h).
In addition to the efficiency of diffusion into the skin, the skin tolerance is another concern for topical delivery systems. Selenium should be used with caution as a topically applied reagent since it may increase the risk of nonmelanoma skin cancer in excessive doses48. TEWL was utilized to assess the degree of SC disruption, and a good correlation between the chemical damage to the skin barrier and TEWL increment was demonstrated49. By evaluating established endpoints of skin irritation, the present work found that the topical application of Se-L-M for up to 5 d did not cause TEWL enhancement. Although Se-L-M caused some abrasion or disarray of the SC according to a histopathological examination, the barrier function of the SC did not fail. It was shown that the complete removal of lipids from the SC led to a 100-fold increase in water permeability50. Healthy skin has a slightly acidic pH, and the acidity of the skin maintains antimicrobial activity18. Disturbing this naturally acidic mantle may cause skin diseases. On the other hand, the a*-coordinate of colorimetry correlates well with inflammatory interactions of the skin, especially viable skin24. Se-L-M delivered by a topical route may be safe for both skin acidity and viable skin. Although inflammation occurred by monitoring skin slices, this irritation was not significant. An interesting result was that the inflammation induced by the 0.3% dose was less than that with 0.2%. This may have been due to a secondary barrier of the skin formed by the metals as cited above.
Conclusions
As demonstrated in this study, Se-L-M was readily absorbed by the skin in both the in vitro and in vivo experiments. Se-L-M in a zwitterion form revealed higher permeation compared to the other forms. A linear correlation was observed between the flux and skin deposition. The DL form of selenomethionine showed less skin absorption than did the L form, indicating a stereoselective character of this compound. Other selenium compounds including selenium sulfide and CdSe quantum dot nanoparticles exhibited no or only negligible skin delivery. Intracellular but not intercellular pathways were an important route for Se-L-M penetration via the SC. Summarizing the results of the present work, it was concluded that it may be suitable to develop dermal preparations of Se-L-M to protect against the harmful effects of UV. A preliminary safety examination of the skin indicated acceptable skin tolerance to Se-L-M. The established profiles of Se-L-M skin absorption will be helpful in developing topical products of this compound. More in vivo and clinical information on the efficacy and safety of the percutaneous absorption of Se-L-M is required to assess future practicability.
Author contribution
Jia-you FANG and Saleh A AL-SUWAYEH designed research; Chih-hung LIN, Chia-lang FANG, and Shih-yun YANG performed research; Chih-hung LIN analyzed data; and Jia-you FANG and Saleh A AL-SUWAYEH wrote the paper.
References
Cross CE, van der Vliet A, Louie S, Thiele JJ, Halliwell B . Oxidative stress and antioxidants at biosurfaces: plants, skin, and respiratory tract surfaces. Environ Health Perspect 1998; 106: 1241–51.
Aziz MH, Reagan-Shaw S, Wu J, Longley BJ, Ahmad N . Chemoprevention of skin cancer by grape constituent resveratrol: relevance to human disease? FASEB J 2005; 19: 1193–5.
Richelle M, Sabatier M, Steiling H, Williamson G . Skin bioavailability of dietary vitamin E, carotenoids, polyphenols, vitamin C, zinc, and selenium. Br J Nutr 2006; 96: 227–38.
Nelson PS, Montgomery B . Unconventional therapy for prostate cancer: good, bad or questionable? Nat Rev Cancer 2003; 3: 845–58.
Wan XS, Ware JH, Zhou Z, Dohahue JJ, Guan J, Kennedy AR . Protection against radiation-induced oxidative stress in cultured human epithelial cells by treatment with antioxidant agents. Int J Radiat Oncol Biol Phys 2006; 64: 1475–81.
Clark LC, Graham GF, Crounse RG, Grimson R, Hulka B, Shy CM . Plasma selenium and skin neoplasms: a case control study. Nutr Cancer 1984; 6: 13–21.
Burke KE, Burford RG, Combs GF, French IW, Skeffington DR . The effect of topical L-selenomethionine on minimal erythema dose of ultraviolet irradiation in humans. Photodermatol Photoimmunol Photomed 1992; 9: 52–7.
McKenzie RC, Beckett GJ, McLean S, Arthur JR, Macve JC, Nicol F, et al. Differential effects of doses and forms of dietary selenium on immune cell numbers in the skin of ultraviolet-irradiated and unirradiated mice. Biol Trace Elem Res 2008; 125: 255–67.
Payette MJ, Whalen J, Grant-Kels JM . Nutrition and nonmelanoma skin cancers. Clin Dermatol 2010; 28: 650–62.
Ryan-Harshman M, Aldoori W . The relevance of selenium to immunity, cancer, and infectious/inflammatory diseases. Can J Diet Pract Res 2005; 66: 98–102.
Xiong S, Markesbery WR, Shao C, Lovell MA . Seleno-L-methionine protects against -amyloid and iron/hydrogen peroxide-mediated neuron death. Antioxid Redox Signal 2007; 9: 457–67.
Vinceti M, Wei ET, Malagoli C, Bergomi M, Vivoli G . Adverse health effects of selenium in humans. Rev Environ Health 2001; 16: 233–51.
Heard CM, Johnson S, Moss G, Thomas CP . In vitro transdermal delivery of caffeine, theobromine, theophylline and catechin from extract of Guarana, Paullinia Cupana. Int J Pharm 2006; 317: 26–31.
Hung CF, Lin YK, Zhang LW, Chang CH, Fang JY . Topical delivery of silymarin constituents via the skin route. Acta Pharmacol Sin 2010; 31: 118–26.
Hostynek JJ . Factors determining percutaneous metal absorption. Food Chem Toxicol 2003; 41: 327–45.
Read JF, Wyand AEH . The kinetics and mechanism of the oxidation of seleno-DL-methionine by potassium ferrate. Transition Met Chem 1998; 23: 755–62.
Marti-Mestres G, Mestres JP, Bres J, Martin S, Ramos J, Vian L . The in vitro” percutaneous penetration of three antioxidant compounds. Int J Pharm 2007; 331: 139–44.
Zhai H, Behnam S, Villarama CD, Arens-Corell M, Choi MJ, Maibach HI . Evaluation of the antioxidant capacity and preventive effects of a topical emulsion and its vehicle control on the skin response to UV exposure. Skin Pharmacol Physiol 2005; 18: 288–93.
Godin B, Touitou E . Transdermal skin delivery: predictions for humans from in vivo, ex vivo and animal models. Adv Drug Deliv Rev 2007; 59: 1152–61.
Pan TL, Wang PW, Al-Suwayeh SA, Chen CC, Fang JY . Skin toxicology of lead species evaluated by their permeability and proteomic profiles: a comparison of organic and inorganic lead. Toxicol Lett 2010; 197: 19–28.
Finnin BC, Morgan TM . Transdermal penetration enhancers: applications, limitations, and potential. J Pharm Sci 1999; 88: 955–8.
Meylan WM, Howard PH . Atom/fragment contribution method for estimating octanol-water partition coefficients. J Pharm Sci 1995; 84: 83–92.
Saija A, Tomaino A, Trombetta D, De Pasquale A, Uccella N, Barbuzzi T, et al. In vitro and in vivo evaluation of caffeic and ferulic acids as topical photoprotective agents. Int J Pharm 2000; 199: 39–47.
Zhang LW, Al-Suwayeh SA, Hsieh PW, Fang JY . A comparison of skin delivery of ferulic acid and its derivatives: evaluation of their efficacy and safety. Int J Pharm 2010; 399: 44–51.
Vvrová K, Lorencová K, Klimentová J, Novotný J, Holý A, Hrabálek A . Transdermal and dermal delivery of adefovir: effects of pH and permeation enhancers. Eur J Pharm Biopharm 2008; 69: 597–604.
Ryman-Rasmussen JP, Riviere JE, Monteiro-Riviere NA . Penetration of intact skin by quantum dots with diverse physicochemical properties. Toxicol Sci 2006; 91: 159–65.
Van Lierde V, Chry CC, Roche N, Monstrey S, Moens L, Vanhaecke F . In vitro permeation of chromium species through porcine and human skin as determined by capillary electrophoresis-inductively coupled plasma-sector field mass spectrometry. Anal Bioanal Chem 2006; 384: 378–84.
Rafferty TS, McKenzie RC, Hunter JAA, Howie AF, Arthur JR, Nicol F, et al. Differential expression of selenoproteins by human skin cells and protection by selenium from UVB-radiation-induced cell death. Biochem J 1998; 332: 231–6.
Nicolazzo JA, Morgan TM, Reed BL, Finnin BC . Synergistic enhancement of testosterone transdermal delivery. J Control Release 2005; 103: 577–85.
Huang ZR, Hung CF, Lin YK, Fang JY . In vitro and in vivo evaluation of topical delivery and potential dermal use of soy isoflavones genistein and daidzein. Int J Pharm 2008; 364: 36–44.
Bowen JL, Heard CM . Film drying and complexation effects in the simultaneous skin permeation of ketoprofen and propylene glycol from simple gel formulations. Int J Pharm 2006; 307: 251–7.
Nicoli S, Bunge AL, Delgado-Charro MB, Guy RH . Dermatopharmacokinetics: factors influencing drug clearance from the stratum corneum. Pharm Res 2009; 26: 865–71.
Lademann J, Ilgevicius A, Zurbau O, Liess HD, Schanzer S, Weigmann HJ, et al. Penetration studies of topically applied substances: optical determination of the amount of stratum corneum removed by tape stripping. J Biomed Opt 2006; 11: 054026.
Zhang LW, Monteiro-Riviere NA . Assessment of quantum dot penetration into intact, tape-stripped, abraded and flexed rat skin. Skin Pharmacol Physiol 2008; 21: 166–80.
Wang JJ, Sung KC, Huang JF, Yeh CH, Fang JY . Ester prodrugs of morphine improve transdermal drug delivery: a mechanistic study. J Pharm Pharmacol 2007; 59: 917–25.
Panchagnula R, Desu H, Jain A, Khandavilli S . Effect of lipid bilayer alteration on transdermal delivery of a high-molecular-weight and lipophilic drug: studies with paclitaxel. J Pharm Sci 2004; 93: 2177–83.
Touitou E, Godin B, Karl Y, Bujanover S, Becker Y . Oleic acid, a skin penetration enhancer, affects Langerhans cells and corneocytes. J Control Release 2002; 80: 1–7.
Roy SD, Chatterjee DJ, Manoukian E, Divor A . Permeability of pure enantiomers of ketorolac through human cadaver skin. J Pharm Sci 1995; 84: 987–90.
Panus PC, Ferslew KE, Tober-Meyer B, Kao RL . Ketoprofen tissue permeation in swine following cathodic iontophoresis. Phys Ther 1999; 79: 40–9.
Fang JY, Hung CF, Chi CH, Chen CC . Transdermal permeation of selegiline from hydrogel-membrane drug delivery systems. Int J Pharm 2009; 380: 33–9.
Burke KE, Clive J, Combs GF, Nakamura RM . Effects of topical L-selenomethionine with topical and oral vitamin E on pigmentation and skin cancer induced by ultraviolet irradiation in Skh:2 hairless mice. J Am Acad Dermatol 2003; 49: 458–72.
Kakourou T, Uksal U . Guidelines for the management of tinea capitis in children. Pediatr Dermatol 2010; 27: 226–8.
Cummins LM, Kimuka ET . Safety evaluation of selenium sulfide shampoo in seborrheic dermatitis. Toxicol Appl Pharmacol 1971; 20: 89–96.
Frasco M, Chaniotakis N . Bioconjugated quantum dots as fluorescent probes for bioanalytical applications. Anal Bioanal Chem 2010; 396: 229–40.
Gopee NV, Roberts DW, Webb P, Cozart CR, Siitonen PH, Latendresse JR, et al. Quantitative determination of skin penetration of PEG-coated CdSe quantum dots in dermabraded but not intact SKH-1 hairless mouse skin. Toxicol Sci 2009; 111: 37–48.
Mortensen LJ, Oberdorster G, Pentland AP, Delouise LA . In vivo skin penetration of quantum dot nanoparticles in the murine model: the effect of UVR. Nano Lett 2008; 8: 2779–87.
Jeong SH, Kim JH, Yi SM, Lee JP, Kim JH, Sohn KH, et al. Assessment of penetration of quantum dots through in vitro and in vivo human skin using the human skin equivalent model and the tape stripping method. Biochem Biophys Res Commun 2010; 394: 612–5.
Duffield-Lillico AJ, Slate EH, Reid ME, Turnbull BW, Wilkins PA, Combs GF, et al. Selenium supplementation and secondary prevention of nonmelanoma skin cancer in a randomized trial. J Natl Cancer Inst 2003; 95: 1477–81.
Fang JY, Tsai TH, Lin YY, Wong WW, Wang MN, Huang JF . Transdermal delivery of tea catechins and theophylline enhanced by terpenes: a mechanistic study. Biol Pharm Bull 2007; 30: 343–9.
Serup J, Agner T . Colorimetric quantification of erythema -— a comparison of two colorimeters (Lange Micro Color and Minolta Chroma Meter CR-200) with a clinical scoring scheme and laser-Doppler flowmetry. Clin Exp Dermatol 1990; 15: 267–72.
Acknowledgements
We thank the financial support from Chang Gung Memorial Hospital, Kweishan, Taoyuan, Taiwan, China (CMRPD170162).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Lin, Ch., Fang, Cl., Al-suwayeh, S. et al. In vitro and in vivo percutaneous absorption of seleno-L-methionine, an antioxidant agent, and other selenium species. Acta Pharmacol Sin 32, 1181–1190 (2011). https://doi.org/10.1038/aps.2011.89
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2011.89
Keywords
This article is cited by
-
Optimization of Selenium Inclusion Level in the Larval Diet of Labeo rohita
Biological Trace Element Research (2023)