Abstract
Aim:
To investigate the synergism of low-doses of amlodipine and irbesartan on reduction of blood pressure variability (BPV), amelioration of baroreflex sensitivity (BRS) and organ protection in spontaneously hypertensive rats (SHR).
Methods:
The rats were administered amlodipine (1 mg·kg−1·d−1) alone, irbesartan (10 mg·kg−1·d−1) alone, or the combination of the two drugs for 4 months. The drugs were mixed into the rat chow. Blood pressure (BP) was continuously monitored in conscious animals. After the determination of BRS, the rats were killed for morphological evaluation of organ damages.
Results:
The combination of low-dose irbesartan and amlodipine had statistically significant synergism on reduction of BP and BPV, amelioration of BRS and organ protection in SHR. Multiple regression analysis showed that the decrease in left ventricular hypertrophy was associated with the decrease in systolic BPV (r=0.665, P<0.01); the decrease in aortic hypertrophy was associated with the increase in BRS (r=0.656, P<0.01); and the amelioration in renal lesion was associated with the increase in BRS (r=0.763, P<0.01) and the decrease in systolic BPV (r=0.706, P<0.01).
Conclusion:
Long-term treatment with a combination of low-doses of amlodipine and irbesartan showed significant synergism on reduction of BP and BPV, restoration of BRS and organ protection in SHR. Besides BP reduction, the enhancement of BRS and reduction of BPV might contribute to the organ protection.
Similar content being viewed by others
Introduction
It is well known that blood pressure (BP) level is an important determinant for the end-organ damage in hypertensive patients or hypertensive animals. However, BP level is certainly not the unique determinant for end-organ damage. Recently, it has been proposed that blood pressure variability (BPV) and baroreflex sensitivity (BRS) may be two important factors determining organ damage in hypertension1, 2, 3, 4, 5, 6. This implies that antihypertensive treatment should aim at not only reducing BP values but also reducing BPV and enhancing BRS.
The importance of a combination therapy has been well recognized in the treatment of hypertension7, 8. To better control BP is the main objective of the combination therapy. Generally speaking, a combination of two drugs belonging to different classes may possess a synergism on BP reduction. However, limited imformation is available about whether such a combination possesses a synergism on BPV reduction, BRS restoration and organ protection. Irbesartan, an angiotensin II receptor blocker, and amlodipine, a dihydropyridine calcium antagonist, are two widely used drugs in the treatment of hypertension. They belong to two different classes of antihypertensives and the mechanisms of action are quite different for these two drugs. Therefore, the present work was designed to investigate the possible synergism of irbesartan and amlodipine on BP and BPV reduction, BRS restoration and organ protection in spontaneously hypertensive rats (SHR).
Materials and methods
Animals and chemicals
Male SHRs with an age of 18 weeks were provided by the animal center of Second Military Medical University. The rats were housed with controlled temperature (22–24 °C) and lighting (8:00–20:00 light, 20:00–8:00 dark) and with free access to food and tap water. All the animals used in this work received humane care in compliance with institutional animal care guidelines. Antihypertensive drugs used in this study are as follows: amlodipine (Nanjing Pharmaceutical Co Ltd, Nanjing, China) and irbesartan (Jiangsu Hengrui Pharmaceutical Co Ltd, Lianyungang, China).
Drug administration
Studies were performed in four groups of SHR. Irbesartan, amlodipine or combination of these two drugs were mixed in the rat chow. The consumption of rat chow containing drugs was determined previously. The content of drugs in the rat chow was calculated according to the chow consumption, and the ingested doses of drugs were approximately 10 mg·kg−1·d−1 for irbesartan, 1 mg·kg−1·d−1 for amlodipine and 1+10 mg·kg−1·d−1 for the combination of these two drugs. The control SHR group received the same diet without the drugs. We used relatively low doses of drugs to avoid a very remarkable normalization of BP in the treatment, which would make it much difficult to distinguish the contribution of blood pressure variability and baroreflex sensitivity to organ protection from that of blood pressure. After 4 months of drug administration, BP was recorded during 24 h, and then BPV was calculated and BRS was determined in conscious freely moving rats. Histopathological examinations were performed after BP recording and BRS studies.
BP measurement
Systolic BP (SBP), diastolic BP (DBP) and heart period (HP) of rats were continuously recorded using a previously described technique9, 10. Briefly, rats were anesthetized with a combination of ketamine (40 mg/kg) and diazepam (6 mg/kg). A floating polyethylene catheter was inserted into the lower abdominal aorta via the left femoral artery for BP measurement, and another catheter was placed into the left femoral vein for intravenous injection. The catheters were exteriorized through the interscapular skin. After a 3-d recovery period, the animals were placed for BP recording in individual cylindrical cages containing food and water. The aortic catheter was connected to a BP transducer via a rotating swivel that allowed the animals to move freely in the cage. The hemodynamic recording system used in the present work is MPA-HBBS blood pressure and heart rate analysis system (Model: MPA-HBBS. Shanghai Alcott Biotech Co, LTD, Shanghai, China). The transducer is ALC-AP12 blood pressure sensor (Model: ALC-AP12. Shanghai Alcott Biotech Co, Ltd, Shanghai, China). After about 14-h habituation, the BP signal was digitized by a microcomputer. SBP, DBP and HP values from every heartbeat were determined on line. The mean values and standard deviation of these parameters (including all beats) during a period of 24 h were calculated. The standard deviation was defined as the quantitative parameter of BPV, ie systolic BPV (SBPV), diastolic BPV (DBPV), and HP variability (HPV).
BRS measurement
To determine the function of arterial baroreflex in conscious rats, the methods widely used are derived from that of Smyth firstly applied for humans11. The principle of this method is to measure the prolongation of HP in response to an elevation of BP. With some modifications, this method was used in conscious rats12, 13. A bolus injection of phenylephrine was used to induce an elevation of BP. The dose of phenylephrine was adjusted to raise SBP between 20 and 40 mmHg. HP was plotted against SBP for linear regression analysis and the slope of SBP-HP was expressed as BRS (ms/mmHg).
Morphological examination
The animal was weighed and killed by decapitation. The thoracic and peritoneal cavities were immediately opened. The right kidney, aorta and heart were excised and rinsed in cold physiological saline. The right kidney was blotted, and weighed. The left ventricle was isolated, blotted, and weighed. At the same time, the aorta was cleaned of adhering fat and connective tissue. Just below the branch of the left subclavicular artery, a 30-mm-long segment of thoracic aorta was harvested, blotted, and weighed. Ratios of left ventricular weight to body weight (LVW/BW), and aortic weight to the length of aorta (AW/length) were calculated14. Histopathological observation was also carried out with our conventional method15. Briefly, immediately after gross detection, all samples of left ventricles in 2- to 3-mm-thick slices, aortae and kidney were immersed in formalin solution for more than 1 week, dehydrated in ethanol, cleared in dimethylbenzene and embedded in paraffin. Then 5-μm-thick sections were prepared and stained with hematoxylin and eosin for light microscopic evaluation.
Glomerulosclerosis score
For the semiquantitative evaluation of glomerular damage, the glomerulosclerosis score (GSS) was defined as previously described16. On the light microscopic specimens, approximately 50 glomeruli from the outer cortex and the same number of glomeruli from the inner cortex for each kidney were graded according to the degree of sclerosis: 0, if no mesangial expansion; 1, if mild mesangial expansion (less than 30% of a glomerular area); 2, if moderate mesangial expansion (30%–60% of a glomerular area); 3, if marked mesangial expansion (more than 60% of a glomerular area); and 4, if the sclerosis was global. This was performed by one observer in a blind fashion using coded slides. A weighted composite sclerosis score was then calculated for each kidney according to the following formula: glomerulosclerosis score=[1×(number of grade 1 glomeruli)+2×(number of grade 2 glomeruli) +3×(number of grade 3 glomeruli)+4×(number of grade 4 glomeruli)]×100/(number of glomeruli observed).
Probability sum test
To determine whether the combination was synergistic, we tried to use the probability sum test. This came from classic probability analysis and it was proposed for evaluating the synergism of the combination of 2 drugs (q test)13, 17, 18. In the present work, we used the following criteria. Compared with the mean values of control rats, treated rats with a decrease in BP (SBP or DBP) ≥20 mmHg were defined as responders according to clinical experiences. For other parameters, treated rats with a decrease or increase ≥20% of the mean values of the control group were defined as responders. The formula is as follows: q=PA+B/(PA+PB–PA×PB). Here, A and B indicate drug A and drug B; P (probability) is the percentage of responders in each group. PA+B is real percentage of responder and (PA+PB–PA×PB) is expected response rate. (PA+PB) indicates the sum of the probabilities when drug A and drug B were used alone. (PA×PB) is the probability of rats responding to both drugs when they were used alone, ie, assuming the two drugs act independently. When q<0.85, the combination is antagonistic; when q>1.15, it is synergistic; and when q between 0.85 and 1.15, it is additive.
Statistical analysis
Data are expressed as mean±SEM. Comparisons among groups were made by ANOVA followed by Duncan test. The relationships between hemodynamic parameters and organ damage parameters were analyzed by classic univariate correlation analysis. Stepwise multiple-regression analysis was performed to study the independent effect of hemodynamic parameters on organ damage. F to enter and F to remove were set to P<0.05 and P>0.10, respectively. P<0.05 was considered statistically significant. Statistical analysis was performed by using software SPSS 11.0.0.
Results
Effects on BP, BPV, and BRS in SHR
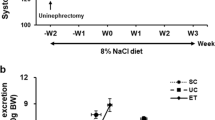
Both long-term amlodipine (1 mg·kg−1·d−1) and irbesartan (10 mg·kg−1·d−1) had no obvious effect on BP level, whereas combination of these two drugs significantly decreased SBP and DBP values in SHR. Amlodipine did not significantly affect the BPV and BRS values, but both irbesartan and the combination marketly decreased SBPV (−21%, P<0.01; −34%, P<0.01, respectively), DBPV (−24%, P<0.05; and −36%, P<0.01, respectively) and obviously enhanced BRS (+77%, P<0.05; and +155%, P<0.05, respectively) in SHR. The extents of BPV reduction and BRS amelioration in combination-treated rats were significantly greater than those in irbesartan-treated rats. No obvious change was found in HP and HPV in any treatment group (Table 1, Figure 1).
Effects on organ damages in SHR
Among organ damage parameters studied, some representative parameters are shown in Figure 2. They are LVW/BW (reflecting left ventricular hypertrophy), AW/length (reflecting aortic hypertrophy) and GSS (reflecting renal damage). It was found that long-term treatment with irbesartan, which had no effect on SBP and DBP levels, significantly decreased LVW/BW (−9.8%, P<0.05), AW/length (−13%, P<0.01) and GSS (−17%, P<0.01) in SHR. No significant decrease in all the three organ damage parameters was found in amlodipine-treated rats. Treatment with the combination significantly decreased all the three organ damage parameters, and the extents of decrease in AW/length (−24%, P<0.01) and GSS (−30%, P<0.01) were greater than those in irbesartan-treated rats.
Effects of long-term treatment with irbesartan, amlodipine alone and in combination on pathological changes in ventricles, aortae, and kidneys in spontaneously hypertensive rats. SHR, spontaneously hypertensive rats (n=11); Irb, irbesartan-treated rats (n=8); Aml, amlodipine-treated rats (n=9); Irb+Aml, combination-treated rats (n=9); LVW, left ventricular weight; BW, body weight; AW, aortic weight; GSS, glomerulosclerosis score. bP<0.05, cP<0.01 vs SHR; eP<0.05, fP<0.01 vs Irb.
Synergism of irbesartan and amlodipine in SHR
Table 2 showed the result of the probability sum test in data from SHR treated with irbesartan, amlodipine and the combination. All q values were larger than 1.15. It was found that the combination of irbesartan and amlodipine possesses a significant synergism on BP and BPV reduction, BRS amelioration and organ protection in SHR.
Relationships between BP, BPV, BRS, and organ damages in SHR
When all the SHRs employed in the present study were pooled as a whole (n=37) for linear regression analysis, relationships between BP, BPV, BRS and organ damages are shown in Table 3. It was found that LVW/BW, AW/length and GSS were all negatively related to BRS and positively related to SBP, SBPV and DBPV, but not to DBP. Both HP and HPV were not correlated with all the three organ damage parameters (data not shown). Some examples for important correlations are shown in Figure 3.
As aforementioned, irbesartan produced organ protective action independent of its BP-lowering effect. To elucidate the role of BPV and BRS in the protection, the relationships between BP, BPV, BRS and organ damages were also analyzed in irbesartan-treated and untreated rats (Table 4). Considering the limited number (n=8) of irbesartan-treated rats would reduced the validity of linear regression analysis, irbesartan-treated rats and control SHRs were pooled as a whole. It was found that both AW/length and GSS were markedly correlated with BRS, and all the three pathological parameters were significantly related to SBPV, but not to SBP or DBP level.
Furthermore, when all the SHRs employed in the present study were pooled as a whole, the relative dependencies of organ damage on hemodynamic parameters were assessed by stepwise multiple-regression analysis. LVW/BW was independently associated with higher SBPV (β=0.657, P<0.01; where β is the standardized partial regressive coefficient). AW/length was independently associated with higher SBPV (β=0.422, P<0.05) and lower BRS (β=−0.371, P<0.05). Glomerulosclerosis score was independently associated with lower BRS (β=−0.525, P<0.01) and higher SBPV (β=0.354, P<0.05).
Discussion
The present work clearly demonstrated the synergism of low-dose irbesartan and amlodipine in reducing BP and BPV, restoring BRS and protecting end organs in SHRs.
It was found that both amlodipine (1 mg·kg−1·d−1) and irbesartan (10 mg·kg−1·d−1) had no obvious effect on BP level, whereas combination of these two drugs significantly decreased SBP and DBP values in SHR. A synergistic effect on SBP and DBP reduction was found in combination therapy (q=1.5 for both SBP and DBP). This synergistic effect would reduce the dose of each drug required in the treatment of hypertension and then could minimize the clinical and metabolic side effects of each individual component in larger dosage when used alone. It has been proposed that dihydropyridines have a natriuretic effect, which is expected to render blood pressure maintenance more angiotensin II-dependent19, 20. This may account for the synergistic effect of amlodipine and irbesartan on BP reduction. In addition, the response of the sympathetic nervous system to the vasodilation induced by dihydropyridines is buffered by concomitant blockade of the renin-angiotensin system, which may contribute to enhancement of the BP reduction as well as to prevention of the reflex increase in heart rate and the palpitations possibly occurring during calcium channel blockade 19, 21.
Clinical observations suggested that BPV was related to organ damages in hypertensive patients1, 22, 23, 24. In animal studies, it has been reported that the organ damages induced by sinoaortic denervation were related to the high BPV but not to BP level25, 26. Accordingly, it seems very important to emphasize the role of BPV in antihypertensive therapy6. However, little information is available about how to better control BPV in the treatment of hypertension. In the present work, chronic treatment with combination of low-dose irbesartan and amlodipine markedly decreased BPV in SHR and an obvious synergism on BPV reduction was found in combination therapy. These results suggested that combination therapy might be more effective in control of BPV than monotherapy.
Arterial baroreflex dysfunction is another feature of hypertension. It has been well recognized that BRS is impaired in hypertensive humans and animals4, 5, 27. It should be noted that baroreflex sensitivity as measured in the present work provides rather limited insight into baroreflex vascular regulation. However, baroreflex sensitivity measured with this technique may mainly reflect the vagal component of baroreflex and is important in the pathology of cardiovascular diseases28, 29, 30. Our previous study proposed that BRS was one of the independent variables related to end-organ damage score in hypertension31. In the present work, long-term treatment with combination of low-dose irbesartan and amlodipine markedly enhanced BRS in SHR, and an obvious synergism on BRS restoration was found in combination therapy. In hypertension, the impairment of baroreflex is mainly the result of elevated BP level32, 33, 34. Therefore, BRS will be enhanced when BP level is lowered by an antihypertensive drug. However, the present work showed that the enhancement of BRS was not attributable to the normalization of BP level in irbesartan-treated rats. It has been reported that endogenous angiotensin II acted at AT1 receptors in the nucleus of the solitary tract (NTS) to attenuate the arterial baroreflex (ABR) function in SHRs and WKY rats, and that microinjection of CV-11974 (AT1 receptors antagonist) in the NTS enhanced the ABR function in SHRs and WKY rats without altering the prevailing level of blood pressure at the same time32. Accordingly, irbesartan, an AT1 receptor antagonist, may act at AT1 receptors in the NTS level to enhance the ABR function in SHRs.
The present work demonstrated that long-term treatment with the combination of irbesartan and amlodipine possessed the obvious effects on organ protection in SHR, and an obvious synergism on organ protection was found in combination therapy. It was found that LVW/BW, AW/length, and GSS were all positively related to SBP, SBPV, and DBPV, and negatively related to BRS in treated and untreated SHRs. In multiple-regression analysis, decrease in left ventricular hypertrophy was most closely associated with the decrease in SBPV, the decrease in aortic hypertrophy was most closely associated with the increase in BRS and the decrease in SBPV, and amelioration in renal lesion was most closely associated with the increase in BRS and the decrease in SBPV. These results suggest that the decrease in BP and BPV and the enhancement of baroreflex function may co-contribute to the organ protective action of drugs in SHR. But, it should be noted that, from a statistical point of view, the aforementioned results of multiple-regression analysis did not necessarily prove that reducing BPV and improving BRS may lead to a higher organ protection.
In addition, the present work showed that irbesartan produced organ protective action independent of its BP-lowering effect. It has been reported that candesartan (an AT1 bloker) was effective in protection against hypertensive organ damage even at dose having no effect on BP, and the blockade of rennin-angiotensin system (RAS) was one of the major mechanisms35, 36, 37. The present work showed that both AW/length and GSS were markedly correlated with BRS, and all the three pathological parameters were significantly related to SBPV, but not to SBP or DBP level in the irbesartan-treated and untreated rats. Therefore, in addition to known mechanisms for RAS antagonists, the present work might show another two possible mechanisms for this BP-independent organ protection of irbesartan: reduction of BPV and enhancement of BRS.
In conclusion, long-term treatment with a combination of amlodipine and irbesartan possessed an obvious synergism in BP and BPV reduction, BRS restoration and organ protection in SHR. Besides BP reduction, the enhancement of BRS and reduction of BPV might importantly contribute to this organ protection.
Author contribution
Wen SHANG, Ping HAN, Cheng-bing YANG, Xiao-wen GU, Wei ZHANG, Li-ping XU, and Shou-ting FU performed research and analyzed data; Ding-feng SU designed research; He-hui XIE designed research, analyzed data, and wrote the paper.
References
Kikuya M, Hozawa A, Ohokubo T, Tsuji I, Michimata M, Matsubara M, et al. Prognostic significance of blood pressure and heart rate variabilities: the Ohasama study. Hypertension 2000; 36: 901–6.
Parati G, Mancia G . Blood pressure variability as a risk factor. Blood Press Monit 2001; 6: 341–7.
Su DF, Miao CY . Reduction of blood pressure variability: a new strategy for the treatment of hypertension. Trends Pharmacol Sci 2005; 26: 388–90.
Su DF, Miao CY . Functional studies of arterial baroreflex function in conscious rats. Acta Pharmacol Sin 2002; 23: 673–9.
Sleight P . The importance of autonomic nervous system in health and disease. Aust N Z J Med 1997; 27: 467–73.
Liu JG, Xu LP, Chu ZX, Miao CY, Su DF . Contribution of blood pressure variability to the effect of nitrendipine on end-organ damage in spontaneously hypertensive rats. J Hypertens 2003; 21: 1961–7.
Gupta AK, Arshad S, Poulter NR . Compliance, safety, and effectiveness of fixed-dose combinations of antihypertensive agents: a meta-analysis. Hypertension 2010; 55: 399–407.
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL Jr, et al. Seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Hypertension 2003; 42: 1206–52.
Xie HH, Miao CY, Liu JG, Su DF . Effects of long-term treatment with candesartan on organ damages in sinoaortic denervated rats. J Cardiovasc Pharmacol 2003; 41: 325–31.
Norman RA Jr, Coleman TG, Dent AC . Continuous monitoring of arterial pressure indicates sinoaortic denervated rats are not hypertensive. Hypertension 1981; 3: 119–25.
Smyth HS, Sleight P, Pickering GW . Reflex regulation of arterial pressure during sleep in man: a quantitative method of assessing baroreflex sensitivity. Circ Res 1969; 24: 109–21.
Su DF, Chen L, Kong XB, Cheng Y . Determination of arterial baroreflex-blood pressure control in conscious rats. Acta Pharmacol Sin 2002; 23: 103–9.
Xie HH, Miao CY, Jiang YY, Su DF . Synergism of atenolol and nitrendipine on hemodynamic amelioration and organ protection in hypertensive rats. J Hypertens 2005; 23: 193–201.
Hayakawa H, Raij L . The link among nitric oxide synthase activity, endothelial function, and aortic and ventricular hypertrophy in hypertension. Hypertension 1997; 29: 235–41.
Miao CY, Tao X, Gong K, Zhang SH, Chu ZX, Su DF . Aterial remodeling in chronic sinoaortic-denervated rats. J Cardiovasc Pharmacol 2001; 37: 6–15.
Kimula K, Tojo A, Matsuoka H, Sugimoto T . Renel arteriolar diameters in spontaneously hypertensive rats: Vascular cast study. Hypertension 1991; 18: 101–10.
Jin ZJ . About the evaluation of drug combination. Acta Pharmacol Sin 2004; 25: 146–7.
Su DF, Xu LP, Miao CY, Xie HH, Shen FM, Jiang YY . Two useful methods for evaluating antihypertensive drugs in conscious freely moving rats. Acta Pharmacol Sin 2004; 25: 148–51.
Waeber B, Ruilope LM . Amlodipine and valsartan as components of a rational and effective fixed-dose combination. Vasc Health Risk Manag 2009; 5: 165–74.
Luft FC, Aronoff GR, Sloan RS, Fineberg NS, Weinberger MH . Calcium channel blockade with nitrendipine. Effects on sodium homeostasis, the renin-angiotensin system, and the sympathetic nervous system in humans. Hypertension 1985; 7: 438–42.
Gennari C, Nami R, Pavese G, Gragnani S, Bianchini C, Buracchi P . Calcium-channel blockade (nitrendipine) in combination with ACE inhibition (captopril) in the treatment of mild to moderate hypertension. Cardiovasc Drugs Ther 1989; 3: 319–25.
Parati G, Pomidossi G, Albini F, Malaspina D, Mancia G . Relationship of 24-hour blood pressure mean and variability to severity of target organ damage in hypertension. J Hypertens 1987; 5: 93–8.
Mancia G, Omboni S, Parati G . The importance of blood pressure variability in hypertension. Blood Press Monit 2000; 5: S9–S15.
Sander D, Kukla C, Klingelhofer J, Winbeck K, Conrad B . Relationship between circadian blood pressure patterns and progression of early carotid atherosclerosis: A 3-year follow-up study. Circulation 2000; 102: 1536–41.
Miao CY, Su DF . The importance of blood pressure variability in rat aortic and left ventricular hypertrophy by sinoaortic denervation. J Hypertens 2002; 20: 1865–72.
Parati G, Lantelme P . Blood pressure variability, target organ damage and cardiovascular events. J Hypertens 2002; 20: 1725–9.
Bristow JD, Honour AJ, Pickering GW, Sleight P, Smyth HS . Diminished baroreflex sensitivity in high blood pressure. Circulation 1969; 39: 48–54.
La Rovere MT, Bigger JT Jr, Marcus FI, Mortara A, Schwartz PJ . Baroreflex sensitivity and heart-rate variability in prediction of total cardiac mortality after myocardial infarction. ATRAMI (Autonomic Tone and Reflexes After Myocardial Infarction) Investigators. Lancet 1998; 351: 478–84.
Mortara A, La Rovere MT, Pinna GD, Prpa A, Maestri R, Febo O, et al. Arterial baroreflex modulation of heart rate in chronic heart failure: clinical and hemodynamic correlates and prognostic implications. Circulation 1997; 96: 3450–8.
Cai GJ, Miao CY, Xie HH, Lu LH, Su DF . Arterial baroreflex dysfunction promotes atherosclerosis in rats. Atherosclerosis 2005; 183: 41–7.
Shan ZZ, Dai SM, Su DF . Relationship between baroreceptor reflex function and end-organ damage in spontaneously hypertensive rats. Am J Physiol 1999; 277: H1200–6.
Parmer RJ, Cervenka JH, Stone RA . Baroreflex sensitivity and heredity in essential hypertension. Circulation 1992; 85: 497–503.
Parmer RJ, Cervenka JH, Stone RA, O'Connor DT . Autonomic function in hypertension: Are there racial difference? Circulation 1990; 81: 1305–11.
Brown AM . Receptors under pressure. An update on baroreceptors. Circ Res 1980; 46: 1–10.
Matsumura K, Averill DB, Ferrario CM . Angiotensin II acts at AT1 receptors in the nucleus of the solitary tract to attenuate the baroreceptor reflex. Am J Physiol 1998; 275: R1611–9.
Nishikawa K . Angiotensin AT1 receptor antagonism and protection against cardiovascular end-organ damage. J Human Hypertens 1998; 12: 301–9.
Murayama S, Hirano T, Sakaue T, Okada K, Ikejiri R, Adachi M . Low-dose candesartan cilexetil prevents early kidney damage in type 2 diabetic patients with mildly elevated blood pressure. Hypertens Res 2003; 26: 453–8.
Acknowledgements
This work was supported by the National Science and Technology Major Project (2009ZX09303-002) and the National Natural Science Foundation of China (No 30971158).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Shang, W., Han, P., Yang, Cb. et al. Synergism of irbesartan and amlodipine on hemodynamic amelioration and organ protection in spontaneously hypertensive rats. Acta Pharmacol Sin 32, 1109–1115 (2011). https://doi.org/10.1038/aps.2011.88
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2011.88