Abstract
Aim:
To evaluate single-dose and multiple-dose pharmacokinetics of cytotoxic T-lymphocyte-associated antigen 4 fusion protein (CTLA4Ig) in healthy volunteers and patients with rheumatoid arthritis (RA).
Methods:
The clinical trials included two phase I open studies: study 1 was an open-label dose-escalation study in 27 healthy volunteers and study 2 was a single-group, open-label study in patients with rheumatoid arthritis. In study 2, 9 patients were arranged to receive 10 mg/kg of CTLA4Ig at 0, 2, 4, 8, 12, and 16 weeks. The concentration-time data obtained by a validated ELISA method were subjected to non-compartmental pharmacokinetic analysis by DAS 2.1 software.
Results:
In study 1, serum CTLA4Ig concentrations climbed rapidly to the peak and declined slowly with a t1/2 of 15.1±2.6 d, 14.2±2.3 d, and 11.8±1.2 d after a single infusion of 1, 10, and 20 mg/kg, respectively. Cmax and AUC0–∞ increased proportionally with the dose. In study 2, the steady-state condition for CTLA4Ig following multiple doses of 10 mg/kg appeared to be attained at the fourth dose (d 56), with peak and trough concentrations of 239.8±45.3 mg/L and 20.5±7.9 mg/L, respectively. After multiple infusions, serum concentrations dropped slowly and the terminal half-life was 12.6±4.7 d.
Conclusion:
Intravenous infusion of CTLA4Ig was well tolerated in healthy volunteers and patients with rheumatoid arthritis. CTLA4Ig exhibited linear pharmacokinetics over the dose range of 1 to 20 mg/kg in healthy volunteers. The pharmacokinetics in RA patients appeared to be similar to that in healthy volunteers. No system accumulation appeared upon repeated infusions of 10 mg/kg every 4 weeks.
Similar content being viewed by others

Introduction
Rheumatoid arthritis (RA) is a chronic, inflammatory, destructive, autoimmune disease of the synovial joints that leads to severe, chronic functional disability and consequent reduction in quality of life1, 2.
Activated T cells are thought to underlie the pathogenic immune response in RA3. T-cells can proliferate, produce pro-inflammatory cytokines such as tumor necrosis factor α (TNFα) and interleukin-1, and activate other cells of the immune system, as well as connective-tissue cells in the joint, which produce metalloproteinases such as matrix metalloproteinase-3 (MMP-3) and inflammatory mediators with subsequent bone and cartilage degradation3, 4. Hence, the inhibition of T-cell activation would be predicted to diminish macrophage activation, pro-inflammatory cytokine production and autoantibody production, thus becoming a new approach to the treatment of rheumatoid arthritis.
Human cytotoxic T-lymphocyte-associated antigen 4 (CTLA4) is a naturally occurring negative regulator, which can block the co-stimulatory signal pathway of B7/CD28 during T cell activation5, 6, 7. CTLA4 is a trans-membrane protein only expressed on the surface of activated T cells. It binds CD80/86 with higher avidity than CD28 but does not transduce activation signals. CTLA4Ig is a fully human soluble fusion protein that consists of the extracellular domain of CTLA4 genetically linked to the modified Fc (hinge, CH2 and CH3 domains) portion of human immunoglobulin G1 (IgG1). Like CTLA4, it competes with CD28 for CD80 and CD86 binding and thereby can be used to selectively inhibit T-cell activation8, 9, 10. CTLA4Ig is constructed based on DNA-recombination technology, produced as a secreted protein in large scale culture of Chinese hamster ovary cell line and purified and formulated as a pharmaceutical-grade product. The apparent molecular weight of this fusion protein is 92 kilodaltons. Preclinical studies demonstrated the in vitro and in vivo efficacy of CTLA4Ig on many autoimmune diseases and allograft rejection models.
Our previous in vitro study has indicated that CTLA4Ig can inhibit T cell proliferation and induce T cell anergy by blocking the B7/CD28 co-stimulatory pathway11. In a mouse allergic contact dermatitis model, CTLA4Ig-treated mice displayed 2,4-dinitro-1-fluorobenzene (DNFB)-specific tolerance, but exhibited a vigorous immune response to FITC upon re-sensitization 14 d after the first challenge. Adoptive transfer of lymphocytes from CTLA4Ig-treated mice could induce inhibition of the contact hypersensitivity response in recipient mice12. We also conducted an in vivo study to evaluate the pharmacokinetics, tissue distribution and excretion of CTLA4Ig in Wistar rats after intravenous injection13. Our data showed that after a single injection with doses of 10, 30, and 100 mg/kg, the drug level reached the climax immediately after the injection ended, and the peak concentration (Cmax) was 0.232±0.019 mg/L, 0.698±0.060 mg/L, and 2.32±0.16 mg/L, respectively. The drug concentration dropped quickly, with a half-life (t1/2) of 41±1 h, 47±2 h, and 54±2 h.
In the present clinical pharmacokinetic trial, we attempt to determine the serum concentration of CTLA4Ig and reveal the pharmacokinetic profile of the protein in healthy volunteers and RA patients, which would provide some theoretical guidance for upcoming clinical trials.
Materials and methods
Drug
The CTLA4Ig formulation was manufactured by the Shanghai Center for Cell Engineering and Antibody. It is a soluble fusion protein that consists of the extracellular domain of human CTLA4 linked to the modified Fc (hinge, CH2, and CH3 domains) portion of human immunoglobulin G1 (IgG1). It is produced by recombinant DNA technology with the CHO cell expression system. The apparent molecular weight is 92 kilodaltons. The CTLA4Ig formulation is provided as a sterile, white, preservative-free, lyophilized powder for parenteral administration. Following reconstitution with 1 mL of sterile water, the solution is clear and colorless to pale yellow with a pH of 7.4. Each single-use vial contains 20 mg CTLA4Ig, 40 mg mannitol, 10 mg sucrose and 1.2 mg Tris (hydroxymethyl) aminomethane.
Study design and subjects
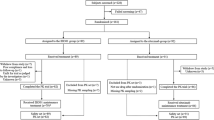
This study was designed as a single-center, open-label clinical trial to investigate the tolerability and pharmacokinetics of the test drug. The whole study was carried out in compliance with the ethics principles of the Declaration of Helsinki and Good Clinical Practice (GCP) guidelines. The study protocol was approved by the ethics committee of Xijing Hospital of the Fourth Military Medical University. All subjects signed the informed consent forms before participation. The study consisted of two parts: Study 1 was an open-label dose escalation study in healthy volunteers. Twenty-seven subjects were assigned randomly into three groups of 9. Every subject was randomly arranged to receive intravenous infusion of 1, 10, and 20 mg/kg. The medication was administered over 60 min. To be included in the study, all volunteers had to be between the ages of 18 and 45; if female, they must have a negative pregnancy test 24 h before study medication administration; have weight within normal limits; have clinical laboratory values within the normal limits 7 d before administration; and have an electrocardiogram and chest X-ray within normal limits. If the subject had one of the following characteristics, he or she would be excluded from participation: presence of pregnancy or lactation; history of hypersensitivity to drug or food; an active infection (like cold or fever); having received any investigational drug within 3 month before medication administration; or history of smoking, alcoholism or illicit drug abuse for at least one year prior to study medication administration.
Study 2 was a single-group, multi-dose, open-label study in patients with rheumatoid arthritis. Nine patients were recruited and received 10 mg/kg of CTLA4Ig in a 60-min intravenous infusion at 0, 2, 4, 8, 12, and 16 weeks. Patients eligible for the study were 18−65 years old and had active rheumatoid arthritis with at least 3 swollen joints and 3 tender joints. The joint function should be grade II or grade III. Use of oral corticosteroids (no more than 10 mg prednisone or its equivalent per day) was allowed if the dose had been stable for at least one week. The background dose of disease-modifying anti-rheumatic drugs (DMARDs) should remain stable for 4 weeks and nonsteroidal antiinflammatory drugs (NSAIDs) for one week. Patients who had one of the following situations were excluded: alanine aminotransferase or total bilirubin level twice the upper limit of normal range or creatinine level 1.25 times higher than the upper limit of normal. Patients were excluded if they had severe concomitant disease or complications in kidneys, heart, lung and blood or had a malignant tumor or family history of cancer. Female patients were excluded if they were pregnant or lactating.
Patients were asked to complete the screening test 7 d before administration of the study medication. Screening tests included medical history inquiries, physical examinations, vital signs and laboratory tests including hematology, serum chemistry test and urine analysis. Consumption of alcoholic beverages and medications was discontinued 7 d before the study and was not allowed during the study. After the subject was verified to be in good health and the informed consent form was obtained, the volunteer received a single dose of CTLA4Ig. In study 1, laboratory examinations were performed 1, 14, 28, 56, and 84 d after medication administration, and physical examinations including vital signs were also conducted. In study 2, laboratory tests were performed immediately before every medication administration. A final physical examination and laboratory test were performed at the end of the study. Adverse events (AEs) were monitored during the treatment and follow-up period. All adverse events were summarized and any relation to the test drug was reported.
Sample collection for pharmacokinetics
In study 1, blood samples for drug concentration detection were drawn from the radial vein before administration, 30 min after the infusion began, and 0, 2, 4, 12, and 24 h after the infusion ended. Blood samples were also drawn 2, 3, 7, 14, 28, 42, 56, 70, and 84 d after the infusion ended. In study 2, blood samples for drug concentration detection were obtained from the radial vein before and immediately after every infusion. Other blood samples were collected at 2, 4, 12, 24 h and 2, 3, 7, 14, 28, 42, 56, 70, and 84 d after the last infusion.
For each sample, serum was harvested by means of centrifugation from about 3 mL whole blood and stored for analysis at −20 °C.
Enzyme-linked immunosorbent assay for CTLA4Ig concentration
Serum concentration of CTLA4Ig was determined by enzyme-linked immunosorbent assay (ELISA). The coating antibody (BD Bioscience, Cat No 58.233.08) was a mouse anti-human CTLA4 monoclonal antibody. The detection antibody (BD Bioscience, Cat No 58.233.02) was a biotinylated mouse anti-human CTLA4 monoclonal antibody. The streptavidin-HRP conjugate (Cat No 41.000.09) was purchased from BD Bioscience. The CTLA4Ig standard was provided by Shanghai Key Lab of Cell Engineering and Shanghai National Engineering Research Center for Antibody Medicine. All serum samples were diluted at most 10 fold with dilution buffer (0.5% bovine serum albumin, 0.1% Tween 20 in phosphate solution) and run in duplicate. A serial standard solution was prepared with 10% blank human serum in dilution buffer.
CTLA4Ig assay procedure was performed as follows: plates were coated with the coating antibody (2 mg/L) at 100 μL/well, incubated for 18 h at 2–8 °C, and then aspirated. Plates were blocked for 2 h at room temperature by the addition of 300 μL/well of blocking solution (0.5% BSA in phosphate solution). After being washed four times with Tris-buffered saline with 0.1% Tween 20, diluted standards (500−2 μg/L) were added at 100 μL/well, followed by the addition of 50 μL/well of detection antibody and incubation for 2 h at room temperature with continuous shaking. After being washed four times, 100 μL/well of streptavidin-HRP (375 mg/L, diluted 1:5000 before use) was added and incubated for 30 min at room temperature with continuous shaking. After being washed four times, 100 μL/well of Chromogen TMB (A/B 1:1) was added and incubated for 30 min at room temperature with continuous shaking, avoiding light. Then 100 μL/well of stop solution (2 mol/L sulfuric acid) was added. The optical density was measured at 450 nm (reference wavelength 650 nm). The standard curve was fitted using the four-parameter logistic equation:

Y represents the absorbance at 450 nm; X represents the concentration of CTLA4Ig; A1 represents the maximal absorbance; A2 represents the minimal absorbance; X0 represents half of the maximal effective concentration and P represents the slope of the log-log curve.
Data analysis
The individual PK parameters were calculated by DAS 2.1 software (Wannan Medical College, Wuhu, China) using non-compartment methods of analysis. Elimination half-life (t1/2), elimination rate constant (Ke), mean retention time (MRT), clearance rate (Cl) and apparent volumes of distribution (Vss) were obtained through this software. The area under the concentration-time curve (AUCs) was calculated using the trapezoidal method. Maximal serum concentration (Cmax) and time to reach peak concentration (Tmax) of CTLA4Ig were defined as observed. Serum drug level below the level of quantification (<20 μg/L) was deemed equal to zero for this calculation.
Statistical analysis
Statistical analysis was performed with SPSS 13.0 software for Windows operation system (SPSS Inc, Chicago, IL, USA). All grouped data were expressed as means±SD. For data among at least three groups, analysis of variance (ANOVA) was applied to test differences of data on normal distribution, and the Kruskal-Wallis test (K-W H test) was used when the data were not normally distributed. For a difference between two groups, the t-test was employed when the data were of normal distribution and variance was homogenous; otherwise, the Wilcoxon test was used. A P value <0.05 was considered statistically significant.
Results
Demographics
In study 1, among the 27 healthy volunteers recruited, there were no significant differences among the three groups with regard to age, sex, height, weight, and body mass index (BMI, Table 1). All subjects completed the study. The ranges of body mass index for the 1 mg/kg, 10 mg/kg and 20 mg/kg dose groups were 22.1−24.0 kg·m−2, 19.8−23.7 kg·m−2 and 20.3−23.7 kg·m−2, respectively.
In study 2, 9 patients with rheumatoid arthritis were assigned to receive 6 doses of CTLA4Ig. The patients included 2 male and 7 female participants who were 61±12 years old, weighed 55±9 kg, and had a height of 163±6 cm and a BMI of 17.9−22.9 kg·m−2. All patients had active disease at baseline, as evidenced by high mean counts of tender and swollen joints, C-reactive protein level and erythrocyte sedimentation rate. Eight patients completed the study and one discontinued follow-up one day after the sixth dose.
Safety
Intravenous infusion of CTLA4Ig was well tolerated in healthy adult volunteers and patients with rheumatoid arthritis. In study 1, no serious clinical or laboratory events were observed during the course of the study. In study 2, seven adverse events were reported, all of which were grade one (mild) in severity. The adverse events included face flushing, cough, upper respiratory tract infection, dizziness, vertigo, blurred vision and mouth dryness.
Validation of the ELISA method for CTLA4Ig determination in human serum A specificity test of the assay has demonstrated that 20% human serum would not interfere with CTLA4Ig quantification. Proteins such as human immunoglobulin, TNFRIg fusion protein and anti-CD20 monoclonal antibody did not interfere with the determination of CTLA4Ig concentration in serum. The recovery rates of blank serum fortified with 125 μg/L, 31.2 μg/L, and 7.8 μg/L CTLA4Ig were 100.7%±8.0%, 102.7%±4.7%, and 106.2%±9.3%, respectively. The coefficient of variations (CV%) of the intra-assay precision and inter-assay precision were no more than 6.8% and 9.3%, respectively. The range of serum concentration quantification was 7.8 to 125 μg/L. Limitation of quantification (LOQ) of the assay was demonstrated to be 4 μg/L if the serum sample was diluted to a minimal ratio of 1:5. The stability of CTLA4Ig in serum was tested for up to 26 h at 2−8 °C and one year at −80 °C.
Single-dose pharmacokinetics of CTLA4Ig in healthy volunteers The mean (±SD) serum concentration-time curves of CTLA4Ig following a dose of 1 mg/kg, 10 mg/kg, and 20 mg/kg are shown in Figure 1. The pharmacokinetic parameters are summarized in Table 2.
In study 1, following a single intravenous dose of 1, 10, and 20 mg/kg in healthy adult subjects, serum CTLA4Ig levels increased sharply and reached the peak soon after the infusion ended, with the maximum serum concentration (Cmax) and AUC0–Z increasing proportionally to the dose. The drug declined slowly with the mean (±SD) terminal half-life (t1/2) of 11.8–15.1 d. The system clearance and distribution volumes were similar among the three single-dose groups. The mean system clearance (Cl) and distribution volume (Vss) ranged from 0.0058 to 0.0067 L·d−1·kg−1 and 0.114 to 0.138 L·kg−1, respectively, with no significant difference among these groups (P>0.05, ANOVA). The Vss value, after a single infusion of three escalating doses over 60 min in healthy volunteers, approximated plasma volume (0.04–0.07 L·kg−1)15, indicating that CTLA4Ig was confined primarily to the vascular system and was not significantly distributed in the extravascular spaces.
Following iv infusion, CTLA4Ig exhibited linear pharmacokinetics over the dose range (1–20 mg/kg) in healthy volunteers. As dose levels increased at a ratio of 1:10:20, the Cmax and AUC0–∞ increased at a ratio of 1:10:23 and 1:9:17, respectively. These ratios indicated that both Cmax and AUC0–∞ were approximately proportional to dosage.
Multiple-dose pharmacokinetics of CTLA4Ig in patients with rheumatoid arthritis The mean (±SD) serum concentration-time profiles of CTLA4Ig following multiple intravenous infusions with a dose of 10 mg/kg are shown in Figure 2. The pharmacokinetic parameters are summarized in Table 3 and Table 4.
Following multiple intravenous infusions (on d 0, 14, and 28 and approximately every 4 weeks thereafter), steady-state conditions for CTLA4Ig, at a dose of 10 mg/kg, appeared to be reached after the fourth dose (d 56) in active rheumatoid arthritis subjects. The mean (±SD) Cmax and Cmin concentrations at steady-state were 239.8±45.3 mg/L and 20.5±7.9 mg/L, and the average concentration was 65.4±25.3 mg/L. The mean (±SD) AUC from 0 to 28 d after the last dose (AUCss) was 1830±708 mg·d·L−1, and the degree of fluctuation (DF) was 369%±100%.
After multiple intravenous infusions of CTLA4Ig at a dose of 10 mg/kg, the mean (±SD) terminal half-life was 12.6±4.7 d, ranging from 4.35 d to 20.9 d. The mean (±SD) system clearance (Cl) was 0.0050±0.0023 L·d−1·kg−1. The mean (±SD) distribution volume (Vss) was 0.074±0.031 L·kg−1.
A comparison of mean Cmin value at 56, 84, and 112 d suggested that no systemic accumulation would appear upon repeated treatments with 10 mg/kg every four weeks in RA patients. The mean (±SD) trough concentrations at 56, 84, and 112 d were 21.7±8.1 mg/L, 20.7±8.2 mg/L, and 19.1±9.0 mg/L (P>0.05, ANOVA), respectively. No significant difference was observed among these values.
After the last infusion of CTLA4Ig at a dose of 10 mg/kg in RA patients, the Vss value approximated the plasma volume, indicating that CTLA4Ig was confined primarily to the vascular system and was not significantly distributed in the extravascular spaces.
The pharmacokinetics of RA patients and healthy volunteers appeared comparable (Table 5). Compared with a single infusion with a dose of 10 mg/kg in healthy volunteers, no significant difference was observed in the terminal half-life (t1/2) and systemic clearance (Cl) after multiple infusions in RA patients (P>0.05, Student's t-test). But the peak concentration (Cmax) after the last dose in RA patients was slightly higher than that of healthy volunteers after a single dose of 10 mg/kg (P<0.05, Student's t-test).
Pharmacodynamic markers affected by CTLA4Ig in RA patients Serum levels of biomarkers [interleukin-6 (IL-6), TNFα and MMP-3] before and after multiple treatment with CTLA4Ig in patients with rheumatoid arthritis are shown in Figure 3.
Pro-inflammatory cytokines like TNFα, MMP-3, and IL-6 are key substances in the initiation and continuation of rheumatoid inflammation4. In study 2, 9 patients with active rheumatoid arthritis received CTLA4Ig treatment with doses of 10 mg/kg at 0, 2, 4, 8, 12, and 16 weeks, and serum samples were obtained at 0, 8, 16, and 28 weeks. Serum IL-6, TNFα and MMP3 levels were determined by ELISA analysis.
Compared with the baseline level, serum IL-6, TNFα and MMP3 levels at 8, 16, and 28 weeks were much lower after multiple treatments with CTLA4Ig. The level of IL-6, TNFα and MMP3 before the treatment was 30.2±9.6 ng/L, 45.0±10.5 ng/L, and 58.4±12.5 μg/L, respectively, and was significantly higher than the level at 16 weeks after treatment (P<0.05, Student's t-test). The levels of IL-6, TNFα, and MMP3 at 16 weeks were 17.3±3.3 ng/L, 23.8±3.0 ng/L, and 30.6±3.4 μg/L, respectively.
Discussion
CTLA4Ig, which is manufactured by the Shanghai Center for Cell Engineering and Antibody, is a recombinant soluble fusion protein that consists of the extracellular domain of human CTLA4 linked to the modified Fc (hinge, CH2 and CH3 domains) portion of human immunoglobulin G1 (IgG1). In this phase I clinical trial, our aim was to investigate the safety and pharmacokinetics of CTLA4Ig in healthy volunteers and patients with rheumatoid arthritis. All subjects tolerated the CTLA4Ig treatment well. Seven adverse events were observed in the multiple-dose study, including facial flushing, coughing, upper respiratory tract infection, dizziness, vertigo, blurred vision and mouth dryness. All adverse events were mild, and the RA patients did not discontinue CTLA4Ig treatment. With the exception of the upper respiratory tract infection, the adverse events disappeared without any treatment.
It has been demonstrated by in vitro data that CTLA4Ig can inhibit T cell proliferation and inhibit T cell activity in vitro by blocking the B7/ CD28 co-stimulatory pathway11, 14. In human mixed-lymphocyte response (MLR) assays, concentrations above 3−12 mg/L of the fusion protein could effectively inhibit T-cell proliferation. The data obtained from study 2 indicated that during the dosing interval, serum concentrations of CTLA4Ig were primarily above the lowest efficacy level (3 mg/L), offering a pharmacologically relevant level for treatment of RA.
Following intravenous administration, CTLA4Ig exhibited a linear pharmacokinetic profile over the dose range of 1 to 20 mg/kg in healthy volunteers because the Cmax and AUC0–∞ increased proportionally to the dose. Following a single intravenous dose of 1, 10, and 20 mg/kg, the serum CTLA4-Ig level increased rapidly and reached a peak soon after the infusion ended. No significant difference was found in the half-life with increasing doses of CTLA4Ig. However, the results in non-clinical pharmacokinetics seemed quite different12. The pharmacokinetics in Wistar rats after single intravenous (iv) injection were demonstrated to be dose-dependent but not dose-proportional over the dose range of 10−100 mg/kg. CTLA4Ig decreased more quickly in rats than in humans with half-lives (t1/2) of 41±1 h, 47±2 h, and 54±2 h. It is not surprising that the dynamics of CTLA4Ig differed in rats, because it is a fully human protein. This human protein consisting of the modified Fc portion of human immunoglobulin G1 (IgG1) will elicit anti-human immune responses when administered to rats. The development of anti-CTLA4Ig antibodies accelerates the elimination of CTLA4Ig in rats. Therefore, non-human primates are more appropriate models for predicting pharmacokinetic profiles of CTLA4Ig and providing a dosing regimen for clinical trials. In fact, we also conducted an in vivo study in rhesus monkeys to evaluate the pharmacokinetics, tissue distribution and excretion of CTLA4Ig at intravenous doses of 2, 20, and 50 mg/kg (data not shown) and obtained valuable information for this clinical trial.
Following multiple intravenous infusions at doses of 10 mg/kg (on d 0, 14, and 28 and approximately every 4 weeks thereafter), the steady-state condition for CTLA4Ig appeared to be reached after the fourth dose (d 56) in active rheumatoid arthritis subjects. The degree of fluctuation (DF) seemed wider than anticipated because the administration route was intravenous infusion without any absorption and the administration interval was almost twice the half-life (12.6 d).
Human in vivo data suggested that in rheumatoid arthritis patients there is an overproduction of several key pro-inflammatory cytokines (TNFα and IL-6) and effector molecules, such as MMP-34. To assess the inhibition effect of the medication, serum TNFα, IL-6, and MMP-3 levels were monitored during treatment with CTLA4Ig in RA patients. Data showed that serum IL-6, TNFα, and MMP-3 levels declined 40%–60% after multiple-dose treatment with CTLA4Ig, which is consistent with the remission response of RA patients.
To evaluate the response of RA patients to medication, an American College of Rheumatology (ACR) score was obtained for efficacy evaluation before and after treatment. Four of eight patients reached the ACR20 level at 16 weeks (the sixth infusion). However, due to the small number of subjects and lack of a placebo control, a conclusion could not be made regarding the efficacy of CTLA4Ig on rheumatoid arthritis.
In summary, our study has demonstrated that CTLA4Ig treatment was well tolerated and exhibited linear pharmacokinetics over the dose range (1–20 mg/kg) in healthy volunteers. Following multiple infusions of 10 mg/kg, patients were generally safe. The serum concentration of CTLA4Ig reached steady state after the fourth dose. It was primarily above the lowest efficacy level (3 mg/L) during the dose interval. Therefore, we recommend that intravenous infusion of CTLA4Ig be used in the future treatment of RA at a dose of 10 mg/kg at 0, 2, and 4 weeks and every 4 weeks thereafter. However, further evaluation of the safety and efficacy with placebo control and more subjects should be investigated in the ongoing pivotal phase II/III clinical trials.
Author contribution
Ying MA, Hao WANG, Ai-dong WEN and Ya-jun GUO designed research; Ying MA, Bi-rong LIN, Bei LIN, Sheng HOU, Wei-zhu QIAN, Min TAN, Jian MA and Fei HAO performed research; Hao WANG contributed new analytical tools and reagents; Jing LI analyzed data; Ying MA, Bi-rong LIN, Jing LI, Bo-hua LI and Ya-jun GUO wrote the paper.
References
Genovese MC, Becker JC, Schiff M, Luggen M, Sherrer Y, Kremer J, et al. Abatacept for rheumatoid arthritis refractory to tumor necrosis factor alpha inhibition. N Engl J Med 2005; 353: 1114–23.
Judith RA, Mark GL, Cynthia AG, Brian VJ, Michael TG, Bernard SG, et al. CTLA4Ig-mediated blockade of T-cell costimulation in patients with psoriasis vulgaris. J Clin Invest 1999; 103: 1243–52.
Kremer JM, Westhovens R, Leon M, Eduardo DG, Rieke A, Serge S, et al. Treatment of rheumatoid arthritis by selective inhibition of T-cell activation with fusion protein CTLA4Ig. N Engl J Med 2003; 349: 1907–15.
Choy EH, Panayi GS . Cytokine pathways and joint inflammation in rheumatoid arthritis. N Engl J Med 2001; 344: 907–16.
John JE, Timothy JS, James PA . CTLA-4 overexpression inhibits T cell responses through a CD28-B7-dependent mechanism. J Immunol 2006; 177: 1052–61.
Todd DJ, Costenbader KH, Weinblatt ME . Abatacept in the treatment of rheumatoid arthritis. Int J Clin Pract 2007; 61: 494–500.
Grennan DM . Re: An association between the CTLA4 exon 1 polymorphism and early rheumatoid arthritis with autoimmune endocrinopathies, by Vaidya et al. Rheumatology (Oxford) 2002; 41: 180–3.
Knoerzer DB, Karr RW, Schwartz BD, Mengle LJ . Collagen-induced arthritis in the BB rat. Prevention of disease by treatment with CTLA-4-Ig. J Clin Invest 1995; 96: 987–93.
Moreland LW, Alten R, Van den Bosch F, Appelboom T, Leon M, Emery P, et al. Costimulatory blockade in patients with rheumatoid arthritis: a pilot, dose-finding, double-blind, placebo-controlled clinical trial evaluating CTLA-4Ig and LEA29Y eighty-five days after the first infusion. Arthritis Rheum 2002; 46: 1470–9.
Kremer JM, Dougados M, Emery P, Durez P, Sibilia J, Shergy W, et al. Treatment of rheumatoid arthritis with the selective costimulation modulator abatacept: twelve-month results of a phase IIb, double-blind, randomized, placebo-controlled trial. Arthritis Rheum 2005; 52: 2263–71.
Zhou Q, Qian WZ, Kou G, Wang H, Liu YJ, Li XD, et al. Effect of CTLA4Ig fusion protein on human T lymphocytes. Chin Pharmacol Bull 2002; 18: 165–8.
Zhou Q, Kou G, Qian WZ, Wang H, Liu YJ, Wang, XY, et al. Treatment of murine allergic contact dermatitis with CTLA4-Ig. Chin J Dermatol 2002; 35: 256–9.
Li ZG, Li J, Wen N, Tang Y, Yuan L, Wang XL, et al. Pharmacokinetic study of I125-CTLA4Ig: absorption, distribution and excretion after a single intravenous administration to rat. Chin J Pharm Anal 2007; 27: 949–53.
Nadler S, Townsend R, Mikesell, G. Abatacept (CTLA4-IG; BMS-188667) significantly inhibits T-cell proliferation in vitro at clinically relevant concentrations. Ann Rheum Dis 2004; 63 Suppl 1: 142.
Wei SL, Zhang Q . Biopharmaceuticals and pharmacokinetics. 2nd ed. Beijing: Peking University Medical Press; 2004.
Acknowledgements
This project was supported by the National Natural Science Foundation of China, Shanghai Commission of Science & Technology, Ministry of Science and Technology of China (973 & 863 Program Projects), and Shanghai Pudong Commission of Science & Technology.
Author information
Authors and Affiliations
Corresponding authors
Rights and permissions
About this article
Cite this article
Ma, Y., Lin, Br., Lin, B. et al. Pharmacokinetics of CTLA4Ig fusion protein in healthy volunteers and patients with rheumatoid arthritis. Acta Pharmacol Sin 30, 364–371 (2009). https://doi.org/10.1038/aps.2009.13
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/aps.2009.13
Keywords
This article is cited by
-
Implantable niche with local immunosuppression for islet allotransplantation achieves type 1 diabetes reversal in rats
Nature Communications (2022)
-
Body mass index and clinical response to intravenous or subcutaneous abatacept in patients with rheumatoid arthritis
Clinical Rheumatology (2017)
-
CTLA4-Ig in B7-1-positive diabetic and non-diabetic kidney disease
Diabetologia (2016)
-
Generation and Preclinical Characterization of a Fc-optimized GITR-Ig Fusion Protein for Induction of NK Cell Reactivity Against Leukemia
Molecular Therapy (2013)
-
Modeling pharmacokinetics/pharmacodynamics of abatacept and disease progression in collagen-induced arthritic rats: a population approach
Journal of Pharmacokinetics and Pharmacodynamics (2013)