Abstract
Magnetic microbubbles (MMBs) are microbubbles (MBs) coated with magnetic nanoparticles (NPs). MMBs not only maintain the acoustic properties of MBs, but also serve as an important contrast agent for magnetic resonance imaging. Such dual-modality functionality makes MMBs particularly useful for a wide range of biomedical applications, such as localized drug/gene delivery. This article reports the ability of MMBs to release their particle cargo on demand under stable oscillation. When stimulated by ultrasound at resonant frequencies, MMBs of 450 nm to 200 μm oscillate in volume and surface modes. Above an oscillation threshold, NPs are released from the MMB shell and can travel hundreds of micrometers from the surface of the bubble. The migration of NPs from MMBs can be described with a force balance model. With this technology, we deliver doxorubicin-containing poly(lactic-co-glycolic acid) particles across a physiological barrier both in vitro and in vivo, with a 18-fold and 5-fold increase in NP delivery to the heart tissue of zebrafish and tumor tissue of mouse, respectively. The penetration of released NPs in tissues is also improved. The ability to remotely control the release of NPs from MMBs suggests opportunities for targeted drug delivery through/into tissues that are not easily diffused through or penetrated.
Similar content being viewed by others
Introduction
Targeted drug delivery and controlled release is the ‘holy grail’ of nanomedicine. In this regard, one emerging strategy employs a localized stimulus to precisely deposit drug-containing nanoparticles (NPs) at the tissue/organ of interest. The deposited NPs then continuously release drug molecules in a localized and sustained manner. Current strategies trigger the release of NPs from carriers via enzymes,1 magnetic fields2 and shear stress.3 However, these methods are limited to specific organs/tissues, such as blocked blood vessels. A more versatile technology is desired that allows the targeted delivery of NPs to any organ/tissue while maintaining traceability using a non-invasive imaging modality.
The present paper reports a strategy toward this end. Magnetic microbubbles (MMBs), the combination of multi-modal contrast-enhanced imaging (both magnetic resonance imaging and ultrasound imaging) with targeted drug delivery (magnetic targeting) and controlled release (bubble cavitation) at any site of interest represents an emerging theranostic platform. However, the current formulations of MMBs, stabilized by a polymeric, lipid or silica shell, need a high acoustic energy field to trigger the release through bubble cavitation/collapse. This high energy and microstreaming may damage the surrounding tissues.4, 5, 6, 7 Our strategy involves stimulating stable oscillating MMBs at their resonant frequencies using ultrasound. MMBs are synthesized by coating a gas core with iron oxide NPs and drug-containing NPs. Magnetic NPs allow MMBs to be concentrated at the targeted organ/tissue via magnetic manipulation. Magnetic NPs can also be detected using magnetic resonance imaging. Furthermore, these MMBs retain the acoustic properties of microbubbles (MBs), making them responsive and detectable via common medical ultrasonic systems.
When stimulated at their resonant frequencies via ultrasound, MMBs of 450 nm to 200 μm oscillate in volume and surface modes. Above a stable oscillation threshold, NPs from the MMB shell are released and can travel hundreds of micrometers away from the surface of the bubble, which allows NPs to penetrate into tissue or across physiological barriers. This controlled and continuous detachment of NPs is accompanied by a concomitant size decrease in the MMBs that eventually ceases once all NPs have detached. More interestingly, this phenomenon is also observed for MMBs that are coated with functional NPs. As a proof of concept, we deliver doxorubicin-containing poly(lactic-co-glycolic acid) (PLGA) particles across a physiological barrier in both in vitro cell cultures and in vivo (zebra fish and mouse models). The ability to remotely control the release of NPs via the oscillation of stable MMBs poses opportunities for targeted drug delivery through/into tissues that are difficult to diffuse through or penetrate without damage to surrounding tissues by bubble cavitation.4, 5, 6, 7
Materials and methods
Cell culture
Colorectal cancer (RKO) cells were acquired from ATCC (Manassas, VA, USA). RKO cells were cultured in Dulbecco’s modified Eagle medium (DMEM) supplemented with 10% fetal bovine serum and 1% penicillin–streptomycin, at 37 °C with 5% CO2. Cells were passaged when they reached 80–90% confluence.
Synthesis of MMBs
Magnetic NPs (Fe3O4, approximately 50 nm, Sigma-Aldrich, St Louis, MO, USA) were first dispersed in deionized (DI) water to form a 2-mg ml−1 stock solution and subjected to ultrasound for 20 min before use. Next, a mixture containing 400 μl of a stock solution of Fe3O4 NPs, 150 μl of 10 mM sodium dodecyl sulfate (SDS) and 150 μl of DI water was agitated either by moderate shaking (~160 oscillations per minute) for 1 min or by homogenization for 0.5–5 min at various stirring speeds. After stirring, MMBs were left overnight before being rinsed with phosphate-buffered saline (PBS) three times before use. MMB diameters were manually measured from the images. Mean values and distributions were calculated using at least 500 MMBs per sample.
Synthesis of functional MMBs
Fluorescent MMBs
Approximately 150 μl of DI water was replaced with the same volume of a particular type of NP. For example, the mixture of SiO2 NPs (Hybrid Silica Technologies, Cambridge, MA, USA) containing MMBs consisted of 400 μl of stock solution of Fe3O4 NPs, 150 μl of 10 mM SDS and 150 μl of 2 mg ml−1 SiO2 NPs.
Dox-PLGA MMBs
Doxorubicin-PLGA particles were prepared using our previous protocol,8, 9 in which 10 mg of doxorubicin was mixed with 100 mg of PLGA. Dox-PLGA MMBs were prepared using the same recipe used for MMBs, in which only 150 μl of DI water was replaced with the same volume of doxorubicin-PLGA particles (10 mg ml−1). Dox-PLGA MMBs with a diameter of 100 μm (coated with 50 nm iron oxide NPs and 1 μm doxorubicin-PLGA particles) were used in the in vitro experiment. Dox-PLGA MMBs with a diameter of 5 μm (coated with 50 nm iron oxide NPs and 200 nm doxorubicin-PLGA particles) were used in the in vivo experiment (mouse tumor model). Through calculation, the loading mass of iron oxide NPs and doxorubicin was estimated as 1.67 × 10−13 g and 3.34 × 10−16 g per dox-PLGA MMBs, respectively.
Scanning electron microscopy and energy dispersive spectroscopy
A drop of MMBs was placed on the silicon wafer and naturally dried, after which the MMBs were imaged using field emission scanning electron microscopy (SEM) (JEOL, Peabody, MA, USA) with energy dispersive spectroscopy (EDAX Inc., Mahwah, NJ, USA). The accelerating voltage was set at 5 kV. Element analysis was performed via energy dispersive spectroscopy analysis of at least three regions (~15 × 15 μm) per sample.
Measurement of MMB resonant frequencies
Polydimethylsiloxane microfluidic channels (1 cm × 1 mm × 0.2 mm) were fabricated on a glass slide. A piezo transducer was attached to the top of the glass slide adjacent to the microchannels, after which the acoustic pressure on the glass plate was measured.10 Next, MMBs were injected into the microfluidic channel using a syringe. Upon sweeping the ultrasonic frequency from 10 to 1000 kHz through a function generator, the resulting MMB oscillations were recorded using a high-speed camera (Photron SA1.1, Brookfield, CT, USA) at 100 000 frames per second. For driving frequencies equal to or larger than 100 kHz, the resonant frequencies were determined by video visualization of particle detachment and microstreaming flow. The time points at which resonance occurred were then correlated to the corresponding driving frequencies. For driving frequencies ranging from 10 to 100 kHz, the resonant frequencies were determined via the maximal change in bubble radius. The bubble radius was extracted from images taken with the high-speed camera at 100 000 frames per second. The bubble contours were then fitted to circles, and their radii were extracted.11
Controlled release of particles from oscillating MMBs
After MMBs with a diameter of 67 μm were injected into a microchannel, they were activated by a driving frequency at their resonant frequency (47 kHz). By adjusting the ultrasonic amplitude from 8 to 82 Vpp, the corresponding high-speed recordings were taken at 100 000 frames per second. To visualize the release of fluorescent SiO2 NPs, images were acquired using a CCD camera (Sensicam QE, Kelheim, Germany) in which the driving frequency was swept from 40 to 50 kHz for 100 ms with an amplitude of 80 Vpp.
Controlled dox-PLGA particle delivery from oscillating dox-PLGA MMBs in 2D
RKO cells were seeded in 6-well plates (0.2 × 106 cells per well) and cultured in DMEM supplemented with 10% fetal bovine serum and 1% penicillin–streptomycin. A piezo transducer was pre-attached to the bottom of the plate before seeding. After incubation at 37 °C with 5% CO2 for 24 h, 50 μl of dox-PLGA MMBs (100 μm in diameter) was added to the plate, and a magnet was placed under the plate to localize bubbles above the cells. After applying 10 cycles (1 s of exposure every 2 s) of 300 Vpp ultrasonic stimulation (sweeping from 40 to 400 kHz), the magnet was removed. Subsequently, the plate was transferred to an incubator. After incubation for 1 h, floating bubbles were removed and replenished with fresh DMEM, after which the cells were incubated for another 24 h before testing. Bright-field and fluorescent images were captured using an inverted microscope (Olympus, Tokyo, Japan), and the viability of RKO cells was determined by counting the cells still attached to the plate.
For confocal imaging, RKO cells were first washed with PBS three times. Then, cells were collected through trypsinization and resuspended in DMEM supplemented with 1 μg ml−1 Hoechst 33342 and 5 μg ml−1 Vybrant DiO membrane dye. The cell suspension was incubated on ice for 15 min before cells were collected, washed with PBS, and added to a cover slide pre-coated with fibronectin.9 After remaining in the cell incubator for 5 min, the cells were fixed and imaged using an Olympus FluoView FV1000 confocal microscope (Olympus).
Controlled release of dox-PLGA particles from oscillating dox-PLGA MMBs in 3D
RKO cells were stained with DiO following the protocol supplied by Life Technologies (Waltham, MA, USA). Briefly, RKO cells were resuspended in DMEM supplemented with 5 μg ml−1 DiO for 20 min at 37 °C and then washed with PBS twice. After centrifugation, the cell pellets were mixed with 6 ml of alginate acid solution (1% in PBS, pH 7.4) to form a cell suspension with a density of 2.0 × 106 cells per ml. Then, the mixtures were added to a Petri dish pre-attached with a piezo transducer. Gelation was carried out immediately by introducing 100 mM CaCl2 solution (in 10 mM HEPES buffer, pH 7.2) for 10 min, followed by washing with PBS three times and resting with DMEM at 37 °C with 5% CO2 for 24 h. Then, a magnet was placed below the Petri dish to localize dox-PLGA MMBs (50 μl of dox-PLGA MMBs with a diameter of 100 μm) on top of the hydrogel. Particle release was triggered by applying and sweeping an acoustic field from 40 to 400 kHz with an amplitude of 100 Vpp (1 s of exposure in every 10 s, total of 10 cycles), after which the magnet and dox-PLGA MMBs were removed. After washing with PBS three times, the hydrogel layer was imaged using confocal laser scanning microscopy (LSM 710, Carl Zeiss, Oberkochen, Germany). In parallel, free doxorubicin (5 μg ml−1), dox-PLGA particles (50 μg ml−1) and PBS buffer were added to the cell-alginate culture systems for 15 min each, and the resultant samples were processed using the same protocol applied to the samples treated with oscillating dox-PLGA MMBs.
Acoustic response of dox-PLGA MMBs used in in vivo experiment
We have measured the acoustic response of dox-PLGA MMBs used in in vivo experiments. To this end, the focused transducer (V302, Olympus), which is attached to a degassed-water-filled cone, irradiates a water droplet at its focus (the acoustic field generated by the focused transducer was characterized and summarized in Supplementary Figures S14a and b). A needle hydrophone (HNR1000, Onda, Sunnyvale, CA, USA) submerged in the drop records the driving acoustic field and the sound emitted from the bubbles. We compared the recordings from plain water droplets with droplets loaded with 5 μm dox-PLGA MMBs. The transducer is driven by an AC voltage of 698 kHz (near the MMBs’ resonant frequency), and the peak pressure increases linearly from 0 to 1.6 bar within 1 s. Short-time Fourier analyses (that is, spectrograms) reveal prominent subharmonic emissions only in MMB-loaded liquids. In general, the threshold for stable oscillation is identified with the onset of the subharmonic signal12 and is approximately 0.4 bar (see Supplementary Figure S15).
Zebrafish model
Larval zebrafish from the transgenic line Tg(fli1:EGFP) was used for the initial in vivo tests. In this transgenic line, the expression of green fluorescence protein (GFP) was driven via a fli1 promoter, which is expressed in endothelial cells, labeling all vascular structures. Larvae at 5–7 days post fertilization (dpf) were used in all experiments. All animal work received prior approval from the Animal Ethical Committee of the City University of Hong Kong and was in accordance with local animal care guidelines.
NP release in zebrafish
MMBs coated with fluorescent silica NPs (approximately 200 nm in diameter) with a mean diameter of 5 μm were used in the zebrafish study. Fluorescent silica NP-coated MMBs were microinjected into the tissue near the heart of a larva from the fli1 transgenic line (5–7 dpf), and vascular structures were visualized via GFP fluorescence. Ultrasound stimulation (1 MHz, <0.5 bar) was applied for 2 min to trigger the release of NPs from MMBs. To characterize the release profile, confocal fluorescence images were taken before and after ultrasound treatment. For NP release in brain tissue, the MMBs were microinjected into the brain ventricles of a larva from the fli1 transgenic line (5–7 dpf), and the associated tissue was examined using confocal microscopy (SP8, Leica, Wetzlar, Germany) before and after ultrasound treatment (1 MHz, <0.5 bar).
Mouse model
All procedures involving animals were approved by the Institutional Animal Care and Utilization Committee (IACUC) at Nanyang Technological University. Male NOD SCID (non-obese diabetic severe combined immunodeficient) mice (6–8 weeks old) were obtained from In Vivos Pte Ltd (Singapore, Singapore). Cultured RKO cancer cells (3 × 106 cells in 100 μl of serum-free DMEM per injection) were injected subcutaneously into both flanks of the mice. Each tumor xenograft formation was monitored every 3 days until it reached 100 mm3 in volume. Then, the mice were randomly separated into three groups for different treatments, as described below.
NP release in the mouse tumor model
MMBs coated with dox-PLGA NPs (approximately 200 nm in diameter) with a mean diameter of 5 μm were used in the mice study. The mice underwent three different treatments and were grouped accordingly. (1) 100 μl of dox-PLGA MMBs (approximately 1 mg of iron oxide and 0.002 mg of doxorubicin) was injected into mice via the tail vein, after which a disk-shaped (2 cm in diameter) magnet was attached to one tumor xenograft for 30 min, during which the mouse was anesthetized by isoflurane; at the same time, the tumor on the other side of the same mouse did not undergo any magnetic treatment. Next, the mice were treated with ultrasonic irradiation (0.5–2 MHz linear sweep, peak pressure of 2.5 bar at 1 MHz, 0.5 s irradiation period every 2 s) via a focused transducer (point focus transducer, V302, Olympus, coupled by a clone filled with degassed water) that scanned across the top of each tumor (both flanks) for 2 min. (2) The same dose of dox-PLGA MMBs used in (1) was injected in the same manner, followed by magnet application to one tumor xenograft as in (1); however, no ultrasonic trigger was applied to group (2). (3) One hundred microliters of PBS was injected via the tail vein, and neither magnetic attraction nor ultrasonic trigger was applied.
After the above treatments, all mice were killed for tumor harvesting. The tumor tissue was imaged using an IVIS Spectrum CT (PerkinElmer, Waltham, MA, USA) immediately after harvesting, after which the tumors were stored in 10% formalin or −80 °C for histology or element analysis, respectively.
Histology and element analysis
Fixed tumor samples first underwent gradient dehydration using a series of ethanol solutions (30, 50, 60, 70, 80, 90 and 100%, v/v). Then, they were washed and made transparent in xylene. After embedding in paraffin, each sample was cut into 10 μm sections using a rotary microtome (Leica RM 2265), after which each sample was affixed to microscopy slides. Slides containing tissue sections were sequentially immersed in xylene to dissolve excess paraffin and then rehydrated via immersion in decreasing concentrations of ethanol followed by 100% water. Next, the slides were immersed in a freshly prepared solution containing equal parts of 20% HCl and 10% potassium ferrocyanide for 20 min at room temperature. After rinsing in DI water, Prussian-blue-stained slides were immersed in a solution of nuclear fast red for 5 min followed by a water rinse. Slides were dehydrated again, cleared in xylene, coverslipped with mounting medium and allowed to dry overnight.
The freshly harvested tumors were digested in acid (HNO3:HCl, 1:3, v/v) at 60 °C overnight. The resultant solution was analyzed by ICP-MS (inductively coupled plasma mass spectrometry) (Elan-DRCe, Waltham, MA, USA) for iron quantification.
Results and Discussion
Preparation of MMBs
Few reports have been published regarding the synthesis of MMBs, which are stabilized by a polymeric,13, 14, 15, 16 lipid17, 18 or silica19 shell, and the incorporation of magnetic and therapeutic NPs. In these published studies, the shells of MMBs are normally intact, which hinders MB oscillation at low-amplitude driving forces.20 As a result, the release of particle cargo relies on the abrupt collapse and accompanying shell disruption of each MB under high-amplitude driving forces of 3–10 bars.16, 18, 19 Such rapid and asymmetrical collapse (that is, cavitation) results in high shear flows, microjets and microstreaming21 that damage surrounding tissues, such as the endothelium.4, 5, 6, 7 Furthermore, the synchronous burst release of drugs could exceed toxic limits, limiting the clinical application of these MMBs.
The MMBs used in the present study contain gas cores and shells of magnetic NPs (Figure 1a). They were prepared by emulsifying a solution containing anionic surfactants (that is, SDS) and cationic magnetic NPs (that is, 50 nm poly(vinylpyrrolidone)-coated iron oxide (Fe3O4) NPs). SEM revealed that magnetic NPs assembled on each MMB surface and formed a dense shell (Figure 1b). This magnetic shell allowed the MMB to respond to magnetic manipulation (Figures 1g and h) and stabilized the MMB against dissolution in five different buffers for at least 10 days (Supplementary Figures S1a and b). When stored in water, the MMBs remained intact for 1 year (Supplementary Figure S1c). The interaction of magnetic NPs and surfactant (that is, SDS) increases the viscoelasticity of the interface and reduces the surface tension.22 The size of MMBs can be controlled by manipulating the concentrations of magnetic NPs or via stirring speed and time. For example, MMB sizes fell between 100 and 200 μm when they were synthesized using moderate shaking (~160 oscillations per minute) for 1 min (Figure 1c). Using a homogenizer with stirring speeds of approximately 20 000 r.p.m. decreased MMB sizes to approximately 2 μm (Supplementary Figure S2). When the speed (that is, 8000 r.p.m. via a homogenizer) and the magnetic NP concentration (2 mg ml−1) were fixed, a longer emulsification time could also reduce MMB sizes from 10 to 5 μm (Figure 1i and Supplementary Figure S3). If the synthesis was performed at a reduced pressure (0.1 atm), then MMB sizes could be reduced further to approximately 450 nm. Using a higher concentration of magnetic NPs during preparation increased the MMB sizes (Figure 1i) due to the thickening of their shells. The thickness of NP shell also varies with the size of MMB. For example, shell thickness was around 1 μm for MMB with diameter of 100 μm while 200 nm shell was found for MMB with diameter of 5 μm (data not shown).
Characterization of magnetic microbubbles (MMBs). (a) Schematic of an MMB composed of an air core (blue) and a shell of Fe3O4 nanoparticles (NPs) (50 nm, brown). (b) Scanning electron microscopy (SEM) image of an MMB shell. (c) Dark-field image of MMBs. (d) Schematic of fluorescent MMBs composed of an air core (blue) and a shell of Fe3O4 NPs (50 nm, brown) and SiO2 NPs (500 nm, yellow). (e) SEM image of the shell of a fluorescent MMB. (f) Fluorescence image of fluorescent MMBs. (g) MMBs float on the top of the water surface and (h) are attracted by a magnet. (i) Mean diameters of MMBs prepared with different concentrations of Fe3O4/SiO2 NPs and different homogenization times (speed: 8000 r.p.m.).
That the resulting MMBs are stable is evidenced by the presence of magnetic NPs. Subsequently, functional MMBs (Figure 1d) were constructed by replacing magnetic NPs with a mixture of magnetic NPs and other types of functional molecules encapsulated by cationic NPs. For example, fluorescent MMBs were obtained by mixing 500 nm fluorescent silica (SiO2) NPs (encapsulating tetramethyl rhodamine) with 50 nm Fe3O4 NPs during preparation (Figures 1e and f). As shown in Figure 1e, SiO2 NPs were embedded within the Fe3O4 NPs. Similar to the previously synthesized MMBs, the sizes of fluorescent MMBs could be controlled by manipulating either the concentrations of NPs or the stirring speed and time. For example, with fixed NP concentrations (2 mg ml−1 Fe3O4 NPs and 0.2 mg ml−1 SiO2 NPs) and stirring speed (8000 r.p.m.), the sizes of fluorescent MMBs could be decreased from 15 to 5 μm by increasing the homogenization time from 1 to 5 min (Figure 1i and Supplementary Figure S4). Elemental analysis showed that regardless of the stirring speed and time, the ratio of silicon to iron in fluorescent MMBs was between 0.009 and 0.031, comparable to the seeding ratio of silicon to iron (that is, 0.027) (Supplementary Table S1). Thus, the ratio of the two types of NPs on fluorescent MMBs was determined by the seeding ratio of those NPs.
Particle detachment via stable bubble oscillation
Once the synthesized MMBs were exposed to a sufficiently strong resonant ultrasound field, they began to oscillate in a spherical mode (that is, changing radius) near their resonant frequencies.11 High-order shape oscillation modes (that is, shape changes) were observed under increasing driving pressure. If the driving pressure was sufficiently high, then some NPs were released and traveled away from the bubble, similar to the lipid shedding observed from oscillating MBs;23 in other words, the NPs were transported by the flow field generated by the oscillating bubble.
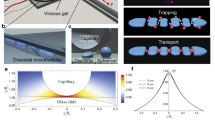
To facilitate quantitative measurements of this process, we confined the motion of MMBs susceptible to buoyancy and acoustic forces.24 This was achieved by floating the MMBs in a microfluidic channel with a width of 1 mm and a height of 0.2 mm. The channel was made using standard soft lithography and was bonded to a glass substrate. The acoustic field was generated via a piezoelectric transducer glued to the substrate (Figure 2a).25 Bright-field images and fluorescence images were captured using an attached high-speed camera and CCD camera, respectively.
Controlled particle release from magnetic microbubbles (MMBs). (a) Schematic of the apparatus used to investigate MMB oscillation and particle release from a single oscillating MMB. (b) Plot of MMB resonant frequency vs radius. (c) Fluorescence images of a fluorescent MMB undergoing volume-mode oscillation and fluorescent SiO2 particles ejected at different times (scale bar: 50 μm). (d) Plot of the distance of released NPs from the fluorescent MMB center vs time. (e) Simulation of particle velocity vs distance to the MMB center for particles with different diameters.
To determine the resonant frequencies of MMBs, we swept the driving frequencies along a certain range at a low amplifier setting. For driving frequencies equal to or larger than 100 kHz, the resonant frequency was determined by visualization of particle detachment and microstreaming flow via video. For driving frequencies ranging from 10 to 100 kHz, the resonant frequency was determined by observing the continuous changes in bubble radii, which were extracted from images taken with the high-speed camera.11 For example, in Supplementary Information Video 1, the resonant frequency of a 45-μm (radius) MMB was determined to be 60 kHz (Supplementary Figure S5).
An examination of MMBs with radii ranging from 6.5 to 65 μm (Figure 2b) illustrated that small MMBs (radii <25 μm) showed characteristic responses similar to MBs lacking NP coatings, whose resonant frequencies are inversely proportional to their radii (Minnaert frequency).26 Owing to the introduction of a shell elastic parameter and the shell friction factor of the NP shell, which ultimately increase the associated resonant frequencies,27 the MMB resonant frequencies measured during these experiments are slightly larger than those obtained for MBs without NP coatings. We note that theoretically the mass loading from our NP shell is negligible.28 Previous work also found that NP shell does not modify the acoustic properties of MMBs.29 However, the resonant frequencies of MMBs with larger radii (>35 μm) stabilized at approximately 50 kHz. Of these, most were smaller than the Minnaert frequency and may have been caused by confinement in the microfluidic channel (Figure 2b).
Next, we exposed a single MMB to an acoustic field at its resonant frequency and increased the acoustic pressure steadily. The bubble’s response switched from a radial volume mode to the shape model oscillation (Supplementary Figure S6). At sufficiently low amplitudes (volume mode), the NPs continuously detached from the MB’s surface, traveling away radially from the bubble (Supplementary Information Video 2). Pronounced shedding of NPs was observed once the shape mode oscillations set in (Supplementary Information Videos 3 and 4). Here, the detached NPs followed radial flow lines known as microstreaming and detached as aggregates. Once the majority of the NPs were removed from the bubble surface, the bubble shrank and dissolved (in the absence of driving).
Particle transport under oscillatory flow
The NP shedding phenomenon enables MMBs to be used as controlled-release carriers, as we demonstrate using MMBs coated with fluorescent particles. A continuous efflux of fluorescent SiO2 NPs was observed at a low driving pressure (Figures 2c and d). At high driving pressure, we observed strong expulsion of fluorescent NPs and the formation of a toroidal vortex (Supplementary Figure S7), within which the NPs spread as far as 400 μm. The fluorescent MMBs dissolved once acoustic driving was switched off.
For practical reasons, it is important to understand the effects of outer parameters, such as driving amplitude and particle size, on the resulting trajectory of the particles. Thus, we used a force balance model to calculate the motion of the particles during release.30 The balanced forces are liquid and particle inertia and a Stokes drag force, as follows:

where ρl and ρp are the water and particle densities, respectively, ul and up are the liquid and particle velocities, respectively, d is the particle diameter, R is the MMB radius, r is the distance to the center of the MMB, dR/dt is the velocity of the bubble surface during the oscillation and CA=0.5 is the added mass coefficient for a spherical particle. We account for confinement by modeling the liquid velocity to decrease according to 1/r. At low driving forces, we assume harmonic oscillation of the bubble radius. In the simulation, the radius of oscillating MMB is R=R0(1+ɛcos(ωt)), where R0 is the radius of the MMB at rest, ɛ=10% is the oscillation amplitude and ω is the angular driving frequency.
The simulation provided plots of particle velocity vs position (distance to the MMB center) for different particle sizes (Figure 2e) and showed that smaller particles tend to move away from the MMB at slower speeds. This model was compared with the recorded trajectory of a 1.4-μm fluorescent particle released from a 65-μm fluorescent MMB (Figure 2c). Experimentally, we exposed the fluorescent MMB to moderate acoustic driving so that it oscillated in the volume mode. Then, we depicted the displacement of the particles from the oscillating bubble against the time exposed to the acoustic field (Figure 2d), which allowed us to derive the velocity of the fluorescent particles vs the distance to the bubble center. As shown in Figure 2e, the experimentally obtained velocity as a function of distance corresponds well with the simulation.
Drug delivery to in vitro cell cultures
As discussed above, to date, the exploration of MMBs for localized drug delivery has relied on the abrupt disruption/collapse of MBs, which generates high shear flows, microjets and microstreaming21 that detach drugs from MB surfaces and drive them toward the intended targets.13, 27, 31, 32, 33 However, the resultant rapid collapse of bubbles (that is, cavitation) may also damage surrounding tissues, such as the endothelium.4, 5, 6, 7 In addition, the synchronous burst release of drugs could exceed toxic limits.
The controlled and moderate release obtained using the present MMB approach may provide a solution to these challenges, given that the detachment and subsequent migration of NPs are not accompanied by microjets resulting from cavitation bubbles. As a proof of concept, we prepared a type of functional MMBs with 50 nm Fe3O4 NPs and 2 μm PLGA particles containing the chemotherapeutic drug doxorubicin (dox-PLGA MMBs). SEM images revealed that the PLGA particles were coated with Fe3O4 NPs and packed together to form a shell (Supplementary Figure S8). To facilitate the visualization of the release of PLGA particles using a fluorescent microscope, the size of dox-PLGA MMBs was maintained at approximately 100 μm.
Next, after using a magnet to localize them on the bottom of the Petri dish, the stability of dox-PLGA MMBs under oscillation was examined in the cell medium. As expected, dox-PLGA MMBs first ejected particles with an MMB collapse ratio of only 8.5% when the MMBs were driven at their resonance frequencies using moderate amplitudes (Supplementary Figure S9). When colorectal cancer cells (that is, RKO cells) were subsequently cultured on the Petri dish, they were labeled with the detached dox-PLGA particles from inside the cellular cytoplasm (Figures 3a and b), which significantly decreased the viability of cancer cells at 24 h post experiment (Figure 3c). This cytotoxicity was clearly caused by the dox-PLGA particles, as the viabilities of cancer cells were only slightly decreased when dox-PLGA-free MMBs were used. More excitingly, when ultrasound was not applied during the experiment, the detachment of dox-PLGA particles from MBs was negligible and demonstrated no influence on cell viability (Figure 3c and Supplementary Figure S10).
Controlled particle release from dox-PLGA magnetic microbubbles (MMBs) to cancer cells in 2D and 3D cultures. (a) Bright-field (top) and fluorescence (bottom) images of RKO cells untreated (left) and treated with oscillating dox-PLGA MMBs (right), followed by 24 h of incubation. Scale bar: 100 μm. (b) Confocal scanning microscopy of RKO cells treated with oscillating dox-PLGA MMBs, in which Hoechst 33342 stains the nuclei, DiO stains the membrane, and the red color represents dox-PLGA particles. Scale bar: 10 μm. (c) Viability of RKO cancer cells treated with different methods after 24 h of incubation. (d) Schematic of the controlled release of dox-PLGA particles from dox-PLGA MMBs. The particles released were able to penetrate into the alginate hydrogel and target the RKO cells. (e) Confocal scanning microscopy and (f) 3D projection of the RKO cells in the hydrogel after treatment with oscillating dox-PLGA MMBs. (g) RKO cells in the hydrogel before any treatment. (h) RKO cells in the hydrogel treated with free doxorubicin for 15 min. (i) RKO cells in the hydrogel treated with dox-PLGA particles for 15 min. The green color corresponds to DiO staining of the membrane, and the red color represents dox-PLGA particles.
We next examined the penetration of controlled-release NPs into a hydrogel. RKO cells were cultured within an approximately 3-mm-thick alginate hydrogel. Subsequently, dox-PLGA MMBs were magnetically localized on the hydrogel before introducing ultrasound at the resonant frequency of dox-PLGA MMBs to induce oscillation (Figure 3d). Within 1 min, dox-PLGA particles were found inside the hydrogel layer, and some particles even entered the cellular cytoplasm of cells within the hydrogel (Figures 3e and f). In comparison, neither free doxorubicin nor dox-PLGA particles (equivalent concentration of doxorubicin) were able to penetrate the hydrogel layer and label the RKO cells during the same incubation time (Figures 3g–i). Previous studies have shown that only 10.52% of added doxorubicin (10 μg ml−1) penetrated into the alginate hydrogel and labeled the cells after at least 2 h.34, 35 Minimal penetration was found at 0.5 and 1 h. The penetration of DiO-loaded lipid NPs was even limited and only 3.41% of added NPs penetrated into the hydrogel after 2 h. Clearly, the technology developed here allows faster and deeper penetration of dox-PLGA particles into the hydrogel.
Drug delivery in in vivo models
To investigate whether the aforementioned abilities of controlled-release NPs were applicable to in vivo systems and to assess the stability and safety of circulating MMBs through the blood, we injected MMBs into two animal models and examined NP release and penetration achieved by ultrasound irradiation. MMBs with a mean diameter of 5 μm (comparable to clinically used MBs, for example, Optison (Little Chalfont, UK), which have a mean diameter of 3.0–4.5 μm) and a stable oscillation threshold of 0.4 bar (see Materials and methods for details) were prepared for this purpose.
The controlled release of fluorescent NPs in vivo was first tested in a zebrafish model (Figures 4a and b), in which the vascular system was genetically labeled with GFP. Fluorescent silica NP (red)-coated MMBs were injected into the tissue near the heart (Figure 4c). After applying an acoustic field (1 MHz, <0.5 bar for 2 min), released fluorescent NPs traveled away from the injection site and entered the heart tissue (outlined with white lines in Figure 4d). This penetration of fluorescent NPs caused an 18-fold increase (over the original intensity) in the fluorescence signal obtained for the associated heart region (Figure 4e).
Controlled fluorescent nanoparticle release from magnetic microbubbles (MMBs) in zebrafish. (a) Representative bright-field image of a zebrafish larva (5 dpf). (b) Confocal microscopy images of a larva from the Fli1 transgenic line injected with fluorescent silica NP-coated MMBs into tissue near the heart. (c) Enlarged views of associated heart regions (boxed in b) showing the delivery of NPs into the heart before (top) and after (bottom) the ultrasound trigger. The vascular structures are genetically labeled with GFP (green) and fluorescent silica NPs are red. (d) Fluorescent signals from NPs near or within the associated heart region (outlined with white lines). (e) Quantitative assessment of fluorescent signal changes as a result of ultrasound-stimulated delivery from NP-loaded MBs. Error bars indicate standard deviation (n=5). Scale bar: 200 μm (a, b) and 25 μm (c, d).
In another experiment, MMBs were injected into zebrafish brain ventricles, and ultrasound was applied (Supplementary Figure S11a). The results obtained were similar to those described immediately above. Specifically, the NPs released via ultrasound treatment penetrated the cerebral cortex at up to 25 μm away from the injection site (Supplementary Figures S11d and e). This result compliments the changes in fluorescence signals observed in the z-direction, which was initially confined to a flat cavity in the brain (Supplementary Figures S11b and c). Under control conditions, that is, without the ultrasound trigger, the majority of the NPs remained in close proximity to the injection site (exhibiting a diffusion distance of approximately 2 μm in the z-direction).
Finally, we examined a mouse tumor model. Briefly, RKO cancer cells were xenografted on both flanks of an immunodeficient mouse model (NOD SCID). Dox-PLGA MMBs (approximately 5 μm in diameter) were injected into each mouse via its tail veins, and a magnet was placed on only one of two tumor xenografts on the same mouse for 30 min (Figure 5a and Supplementary Figure S12a). Within the experimental time frame (2–4 h), no mouse (out of 17 mice in total) showed any observable abnormality after injection of the MBs. After ultrasound irradiation was applied to both xenografts for 2 min (Supplementary Figure S12b), the mice were killed, and tumors were harvested for further analysis.
Controlled nanoparticle release from magnetic microbubbles (MMBs) in a mouse cancer model. (a) Schematic of the experiment performed on the mouse cancer model. Dox-PLGA MMBs (approximately 5 μm in diameter) were injected into each mouse through the tail vein. Subsequently, a magnet was applied for 30 min to one of the two tumor xenografts, followed by 2 min of ultrasound treatment for both tumors. (b) Representative bright-field (i) and fluorescence (ii) images of a harvested tumor (left: without magnetic attraction; right: with magnetic attraction). The color scale represents radiant efficiency (min=1.29 × 107, max=2.47 × 108). Scale bars represent 1 cm. (iii) Fluorescence intensity (fold change) was calculated using the fluorescence intensity ratio between the tumor with (box chart) and without (red dashed line) magnet application on the same mouse (N=5). (c) Representative histological images of tumors treated with dox-PLGA MMBs, a magnet and ultrasound stimulation (i), tumors treated only with dox-PLGA MMBs and a magnet (ii), tumors treated only with dox-PLGA MMBs and ultrasound stimulation (iii) and tumors treated only with PBS (iv). Iron was stained with Prussian blue, and cells were counterstained with nuclear fast red. Black arrows indicate tumor blood vessels. Scale bars represent 100 μm. (d) Iron concentrations in tumors were quantified using ICP-MS. Black dots represent the group treated with dox-PLGA MMBs, a magnet and ultrasound stimulation (N=5); red cycles represent the group treated with dox-PLGA MMBs and a magnet (N=5); green triangles represent the group treated with dox-PLGA MMBs and ultrasound stimulation (N=5); blue open squares represent the group treated with dox-PLGA MMBs only (N=4); cyan squares represent the group treated with PBS only (N=3). Statistical significance was determined by calculating the P-value using the Student’s t-test (two-tailed distribution and two-sample unequal variance).
To semi-quantitatively evaluate the efficacy of doxorubicin delivery using this technology, two tumors from the same mice were imaged, and their fluorescence was quantified (Figure 5b). The tumor volume from the mice was similar despite they exhibit different structures. As shown in Figure 5biii, the tumor with magnetic enrichment showed a fluorescence intensity that was approximately 1.6-fold higher than the other tumor from the same mice, suggesting that magnetic attraction results in higher doxorubicin delivery efficacy.
To examine whether released NPs could penetrate tumor tissue from the vasculature, tumor sections were stained with Prussian blue, showing iron oxide NPs in blue, and were counterstained with nuclear fast red (pink). In the group treated with dox-PLGA MMBs, a magnet and ultrasound stimulation (Figure 5ci), the iron oxide NPs were observed to penetrate and spread within the tumor tissue surrounding the tumor blood vessels. Depending on the histological observation, this penetration could extend for several hundred micrometers. In contrast, when no ultrasound was applied (such that treatment was only with dox-PLGA MMBs and a magnet), a much lower tissue density of iron oxide NPs was observed, and this was mainly entrapped within associated blood vessels (Figure 5cii). The other groups were either treated with dox-PLGA MMBs and ultrasound (no magnet, Figure 5ciii) or treated only with dox-PLGA MMBs (no magnet and no ultrasound, Supplementary Figure S13), neither of which resulted in detectable iron oxide NPs in the tumor tissue; these results were similar to those observed for the buffer control group (treated with buffer only, Figure 5civ).
The histological results were further confirmed by quantifying the iron concentration in the tumor tissue using ICP-MS. As shown in Figure 5d, the tumor group treated with MMBs, a magnet and ultrasound stimulation possessed the highest mean iron concentration (40.7±18.0 μg per gram of wet tissue for which the significance was P<0.05) compared with the other groups. Groups that did not receive magnet treatment (17.8±9.0), ultrasound treatment (8.3±5.7) or either treatment (7.8±8.6) displayed iron concentrations that were highly similar to those obtained for the buffer control group (12.0±3.8). Thus, once the dox-PLGA MMBs are enriched at tumor-blood-vessel sites using magnetic attraction, the associated NPs (both magnetic and dox-PLGA NPs) are released at the blood-vessel site and penetrate into the surrounding tissue only when ultrasound is applied immediately. Without the ultrasound trigger, the majority of the dox-PLGA MMBs is flushed away via blood flow once the magnet is removed, resulting in the inability of NPs to reach the tumor tissue. We observed no evidence of an enhanced permeability and retention effect (entrapped by the tumor) on the MMBs due to their micrometer size (approximately 5 μm). In this drug delivery system, the use of magnetic NPs is necessary for enrichment at the tumor site.
Conclusion
This report presents a new property of MMBs, wherein NPs can be continuously ejected from a stably oscillating MMB shell, preventing bubble disruption and/or other adverse cavitation effects. This property is robust for all types of MMBs, such that non-magnetic, functional NPs in the MMB shell experience the same transport process. MMB size and composition can be controlled via ambient pressure, particle concentration and stirring speed during preparation. Thus, MMB size distribution can be tailored for medical applications. The detachment and migration of NPs from their associated MMBs are dependent on the bubble’s resonant frequency and pressure amplitude. The experimentally determined migration velocities for NPs in the flow field of an oscillating bubble are in agreement with those calculated using a simple model. Animal experiments demonstrated the stable and safe use of MMBs in tissues and blood circulation as well as the feasibility of NP release from MMBs in vivo. This technology may provide a strategy for drug delivery into and through tissues that free drugs or NPs have difficulty in diffusion through or penetration.
References
Wong, C., Stylianopoulos, T., Cui, J., Martin, J., Chauhan, V. P., Jiang, W., Popovic, Z., Jain, R. K., Bawendi, M. G. & Fukumura, D. Multistage nanoparticle delivery system for deep penetration into tumor tissue. Proc. Natl. Acad. Sci. USA 108, 2426–2431 (2011).
Chorny, M., Fishbein, I., Yellen, B. B., Alferiev, I. S., Bakay, M., Ganta, S., Adamo, R., Amiji, M., Friedman, G. & Levy, R. J. Targeting stents with local delivery of paclitaxel-loaded magnetic nanoparticles using uniform fields. Proc. Natl. Acad. Sci. USA 107, 8346–8351 (2010).
Korin, N., Kanapathipillai, M., Matthews, B. D., Crescente, M., Brill, A., Mammoto, T., Ghosh, K., Jurek, S., Bencherif, S. A., Bhatta, D., Coskun, A. U., Feldman, C. L., Wagner, D. D. & Ingber, D. E. Shear-activated nanotherapeutics for drug targeting to obstructed blood vessels. Science 337, 738–742 (2012).
Ay, T., Havaux, X., Van Camp, G., Campanelli, B., Gisellu, G., Pasquet, A., Denef, J. F., Melin, J. A. & Vanoverschelde, J. L. Destruction of contrast microbubbles by ultrasound: effects on myocardial function, coronary perfusion pressure, and microvascular integrity. Circulation 104, 461–466 (2001).
Kobayashi, N., Yasu, T., Yamada, S., Kudo, N., Kuroki, M., Kawakami, M., Miyatake, K. & Saito, M. Endothelial cell injury in venule and capillary induced by contrast ultrasonography. Ultrasound Med. Biol. 28, 949–956 (2002).
Prentice, P., Cuschierp, A., Dholakia, K., Prausnitz, M. & Campbell, P. Membrane disruption by optically controlled microbubble cavitation. Nat. Phys. 1, 107–110 (2005).
Yoshida, K., Nakatani, S., Tsukamoto, A., Ushida, T. & Watanabe, Y. Effects of collapsing bubble in ultrasonic field on soft material. Jpn. J. Appl. Phys. 47, 4200–4204 (2008).
Xu, C., Miranda-Nieves, D., Ankrum, J. A., Matthiesen, M. E., Phillips, J. A., Roes, I., Wojtkiewicz, G. R., Juneja, V., Kultima, J. R., Zhao, W., Vemula, P. K., Lin, C. P., Nahrendorf, M. & Karp, J. M. Tracking mesenchymal stem cells with iron oxide nanoparticle loaded poly(lactide-co-glycolide) microparticles. Nano Lett. 12, 4131–4139 (2012).
Ankrum, J. A., Miranda, O. R., Ng, K. S., Sarkar, D., Xu, C. & Karp, J. M. Engineering cells with intracellular agent–loaded microparticles to control cell phenotype. Nat. Protoc. 9, 233–245 (2014).
Tandiono, T., Siak-Wei Ow, D., Driessen, L., Sze-Hui Chin, C., Klaseboer, E., Choo, A. B., Ohl, S. W. & Ohl, C. D. Sonolysis of Escherichia coli and Pichia pastoris in microfluidics. Lab Chip 12, 780–786 (2012).
Zhao, X., Quinto-Su, P. & Ohl, C.-D. Dynamics of magnetic bubbles in acoustic and magnetic fields. Phys. Rev. Lett. 102, 024501 (2009).
Kenneth, B. B. & Christy, K. H. Gauging the likelihood of stable cavitation from ultrasound contrast agents. Phys. Med. Biol. 58, 127 (2013).
Yang, F., Li, Y. X., Chen, Z. P., Zhang, Y., Wu, J. R. & Gu, N. Superparamagnetic iron oxide nanoparticle-embedded encapsulated microbubbles as dual contrast agents of magnetic resonance and ultrasound imaging. Biomaterials 30, 3882–3890 (2009).
Yang, F., Zhang, M. A., He, W., Chen, P., Cai, X. W., Yang, L., Gu, N. & Wu, J. Controlled release of Fe3O4 nanoparticles in encapsulated microbubbles to tumor cells via sonoporation and associated cellular bioeffects. Small 7, 902–910 (2011).
Cai, X. W., Yang, F. & Gu, N. Applications of magnetic microbubbles for theranostics. Theranostics 2, 103–112 (2012).
Niu, C., Wang, Z., Lu, G., Krupka, T. M., Sun, Y., You, Y., Song, W., Ran, H., Li, P. & Zheng, Y. Doxorubicin loaded superparamagnetic PLGA-iron oxide multifunctional microbubbles for dual-mode US/MR imaging and therapy of metastasis in lymph nodes. Biomaterials 34, 2307–2317 (2013).
Vlaskou, D., Mykhaylyk, O., Krötz, F., Hellwig, N., Renner, R., Schillinger, U., Gleich, B., Heidsieck, A., Schmitz, G., Hensel, K. & Plank, C. Magnetic and acoustically active lipospheres for magnetically targeted nucleic acid delivery. Adv. Funct. Mater. 20, 3881–3894 (2010).
Fan, C.-H., Ting, C.-Y., Lin, H.-J., Wang, C.-H., Liu, H.-L., Yen, T.-C. & Yeh, C. K. SPIO-conjugated, doxorubicin-loaded microbubbles for concurrent MRI and focused-ultrasound enhanced brain-tumor drug delivery. Biomaterials 34, 3706–3715 (2013).
Huang, H.-Y., Liu, H.-L., Hsu, P.-H., Chiang, C.-S., Tsai, C.-H., Chi, H.-S., Chen, S. Y. & Chen, Y. Y. A multitheragnostic nanobubble system to induce blood–brain barrier disruption with magnetically guided focused ultrasound. Adv. Mater. 27, 655–661 (2015).
Hernot, S. & Klibanov, A. L. Microbubbles in ultrasound-triggered drug and gene delivery. Adv. Drug Deliv. Rev. 60, 1153–1166 (2008).
Marmottant, P. & Hilgenfeldt, S. Controlled vesicle deformation and lysis by single oscillating bubbles. Nature 423, 153–156 (2003).
Degen, P., Wieland, D. C. F., Leick, S., Paulus, M., Rehage, H. & Tolan, M. Effect of magnetic nanoparticles on the surface rheology of surfactant films at the water surface. Soft Matter 7, 7655–7662 (2011).
Luan, Y., Lajoinie, G., Gelderblom, E., Skachkov, I., van der Steen, A. F. W., Vos, H. J., Versluis, M. & De Jong, N. Lipid shedding from single oscillating microbubbles. Ultrasound Med. Biol. 40, 1834–1846 (2014).
Werner, L. & Thomas, K. Physics of bubble oscillations. Rep. Prog. Phys. 73, 106501 (2010).
Tandiono, Ohl, S.-W., Ow, D. S. W., Klaseboer, E., Wong, V. V., Dumke, R. & Ohl, C. D. Sonochemistry and sonoluminescence in microfluidics. Proc. Natl. Acad. Sci. USA 108, 5996–5998 (2011).
Minnaert, M. On musical air bubbles and the sounds of running water. Philos. Mag. 16, 235–248 (1933).
Wu, J. & Nyborg, W. L. Ultrasound, cavitation bubbles and their interaction with cells. Adv. Drug Deliv. Rev. 60, 1103–1116 (2008).
Spencer, S. J. Mathematical models for the acoustic response of a solids-loaded encapsulated bubble. J. Acoust. Soc. Am. 137, 2623–2641 (2015).
Sciallero, C. & Trucco, A. Ultrasound assessment of polymer-shelled magnetic microbubbles used as dual contrast agents. J. Acoust. Soc. Am. 133, EL478–EL484 (2013).
Gonzalez-Avila, S. R., Huang, X. H., Quinto-Su, P. A., Wu, T. & Ohl, C. D. Motion of micrometer sized spherical particles exposed to a transient radial flow: attraction, repulsion, and rotation. Phys. Rev. Lett. 107, 074503 (2011).
Mura, S., Nicolas, J. & Couvreur, P. Stimuli-responsive nanocarriers for drug delivery. Nat. Mater. 12, 991–1003 (2013).
Mannell, H., Pircher, J., Rathel, T., Schilberg, K., Zimmermann, K., Pfeifer, A., Mykhaylyk, O., Gleich, B., Pohl, U. & Krötz, F. Targeted endothelial gene delivery by ultrasonic destruction of magnetic microbubbles carrying lentiviral vectors. Pharm. Res. 29, 1282–1294 (2012).
Mannell, H., Pircher, J., Fochler, F., Stampnik, Y., Rathel, T., Gleich, B., Plank, C., Mykhaylyk, O., Dahmani, C., Wörnle, M., Ribeiro, A., Pohl, U. & Krötz, F. Site directed vascular gene delivery in vivo by ultrasonic destruction of magnetic nanoparticle coated microbubbles. Nanomed.-Nanotechnol. Biol. Med. 8, 1309–1318 (2012).
Godugu, C., Patel, A. R., Desai, U., Andey, T., Sams, A. & Singh, M. AlgiMatrix based 3D cell culture system as an in-vitro tumor model for anticancer studies. PLoS ONE 8, e53708 (2013).
Ong, S.-M., Zhao, Z., Arooz, T., Zhao, D., Zhang, S., Du, T., Wasser, M., van Noort, D. & Yu, H. Engineering a scaffold-free 3D tumor model for in vitro drug penetration studies. Biomaterials 31, 1180–1190 (2010).
Acknowledgements
This work was partially supported by NTU-NU Institute of Nanomedicine (M4081502.F40 to XCJ).
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the NPG Asia Materials website
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Gao, Y., Chan, C., Gu, Q. et al. Controlled nanoparticle release from stable magnetic microbubble oscillations. NPG Asia Mater 8, e260 (2016). https://doi.org/10.1038/am.2016.37
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/am.2016.37
This article is cited by
-
Ultrasound and nanomaterial: an efficient pair to fight cancer
Journal of Nanobiotechnology (2022)
-
Targeted drug delivery of magnetic microbubble for abdominal aortic aneurysm: an in silico study
Biomechanics and Modeling in Mechanobiology (2022)
-
Interior non-uniformity of acoustically excited oscillating gas bubbles
Journal of Hydrodynamics (2019)
-
Dynamic capillary assembly of colloids at interfaces with 10,000g accelerations
Nature Communications (2018)