Abstract
OBJECTIVE: Single-slice magnetic resonance imaging (MRI) and computed tomography (CT) are finding increasing use as methods to estimate visceral fat content in human studies. To assess the validity of this approach, we have compared single- and multi-slice MRI methods for the measurement of intra-abdominal adipose tissue content.
MEASUREMENTS: Multi-slice whole-body MR images and single-slices at the level of L2–L3 and L4–L5 were obtained from 59 healthy female volunteers chosen to cover a wide range of body size, and from 17 healthy female volunteers before and after a 6-month exercise intervention.
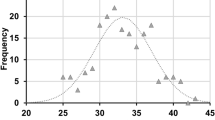
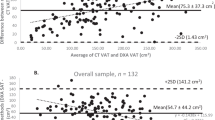
RESULTS: Taking the group as a whole, significant correlation between multi-slice and single-slices was observed (L2–L3: r=0.56; P<0.01; L4–L5: r=0.76; P<0.01). However, the ranking of subjects according to their intra-abdominal fat content was significantly altered by the choice of MRI strategy, especially using L2–L3 methodology. Whole-body (−23.8±20.0%; P<0.01) and single-slice (L2–L3: −31.03±35.0%; P<0.01; L4–L5: −22.1±37.24%; p<0.05) MRI methods also detected a significant decrease in intra-abdominal fat following the exercise protocol, although the latter techniques gave rise to increased spreading of the data from the mean. These results suggest that the use of single-slice imaging techniques can lead to inconsistencies in the estimation of intra-abdominal fat content, which in turn can have significant effects on data interpretation.
CONCLUSION: Single-slice MRI appears to be suitable for assessing changes in intra-abdominal fat content in interventional studies, especially in large cohort of subjects, where each subject can serve as its own control. However, for accurate determination of an individual's intra-abdominal fat content, and intersubject comparison, only multi-slice imaging will give precise results.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Fogelholm M, van Marken Lichtenbelt W . Comparison of body composition methods: a literature analysis. Eur J Clin Nutr 1997; 51: 495–503.
Deurenberg P, Yap M . The assessment of obesity: methods for measuring body fat and global prevalence of obesity. Baillieres Best Pract Res Clin Endocrinol Metab 1999;13: 1–11.
Smith SR, Zachwieja JJ . Visceral adipose tissue: a critical review of intervention strategies. Int J Obes Relat Metab Disord 1999; 23: 329–335.
Abate N, Garg A . Heterogeneity in adipose tissue metabolism: causes, implications and management of regional adiposity. Prog Lipid Res 1995; 34: 53–70.
Fowler PA, Fuller MF, Glasbey CA, Cameron GG, Foster MA . Validation of the in vivo measurement of adipose tissue by magnetic resonance imaging of lean and obese pigs. Am J Clin Nutr 1992; 56: 7–13.
Ross R, Leger L, Guardo R, De Guise J, Pike BG . Adipose tissue volume measured by magnetic resonance imaging and computerized tomography in rats. J Appl Physiol 1991; 70: 2164–2172.
Abate N, Burns D, Peshock RM, Garg A, Grundy SM . Estimation of adipose tissue mass by magnetic resonance imaging: validation against dissection in human cadavers. J Lipid Res 1994; 35: 1490–1496.
Fowler PA, Fuller MF, Glasbey CA, Foster MA, Cameron GG, McNeill G, Maughan RJ . Total and subcutaneous adipose tissue in women: the measurement of distribution and accurate prediction of quantity by using magnetic resonance imaging. Am J Clin Nutr 1991; 54: 18–25.
Ross R, Shaw KD, Martel Y, de Guise J, Avruch L . Adipose tissue distribution measured by magnetic resonance imaging in obese women. Am J Clin Nutr 1993; 57: 470–475.
Sohlstrom A, Wahlund LO, Forsum E . Adipose tissue distribution as assessed by magnetic resonance imaging and total body fat by magnetic resonance imaging, underwater weighing, and body-water dilution in healthy women. Am J Clin Nutr 1993; 58: 830–838.
Thomas EL, Saeed N, Hajnal JV, Brynes A, Goldstone AP, Frost G, Bell JD . Magnetic resonance imaging of total body fat. J Appl Physiol 1998; 85: 1778–1785.
Bonora E, Micciolo R, Ghiatas AA, Lancaster JL, Alyassin A, Muggeo M, DeFronzo RA . Is it possible to derive a reliable estimate of human visceral and subcutaneous abdominal adipose tissue from simple anthropometric measurements? Metabolism 1995; 44: 1617–1625.
Seidell JC, Bakker CJ, van der Kooy K . Imaging techniques for measuring adipose-tissue distribution—a comparison between computed tomography and 1.5-T magnetic resonance. Am J Clin Nutr 1990; 51: 953–957.
Gronemeyer SA, Steen RG, Kauffman WM, Reddick WE, Glass JO . Fast adipose tissue (FAT) assessment by MRI. Magn Reson Imaging 2000; 18: 815–818.
Abate N, Garg A, Peshock RM, Stray-Gundersen J, Adams-Huet B, Grundy SM . Relationship of generalized and regional adiposity to insulin sensitivity in men with NIDDM. Diabetes 1996; 45: 1684–1693.
Treuth MS, Hunter GR, Kekes-Szabo T, Weinsier RL, Goran MI, Berland L . Reduction in intra-abdominal adipose tissue after strength training in older women. J Appl Physiol 1995; 78: 1425–1431.
Gray DS, Fujioka K, Colletti PM, Kim H, Devine W, Cuyegkeng T, Pappas T . Magnetic-resonance imaging used for determining fat distribution in obesity and diabetes. Am J Clin Nutr 1991; 54: 623–627.
Marks SJ, Chin S, Strauss BJ . The metabolic effects of preferential reduction of visceral adipose tissue in abdominally obese men. Int J Obes Relat Metab Disord 1998; 22: 893–898.
Ronnemaa T, Koskenvuo M, Marniemi J, Koivunen T, Sajantila A, Rissanen A, Kaitsaari M, Bouchard C, Kaprio J . Glucose metabolism in identical twins discordant for obesity. The critical role of visceral fat. J Clin Endocrinol Metab 1997; 82: 383–387.
Ross R, Leger L, Morris D, de Guise J, Guardo R . Quantification of adipose tissue by MRI: relationship with anthropometric variables. J Appl Physiol 1992; 72: 787–795.
Kvist H, Chowdhury B, Grangard U, Tylen U, Sjostrom L . Total and visceral adipose-tissue volumes derived from measurements with computed tomography in adult men and women: predictive equations. Am J Clin Nutr 1988; 48: 1351–1361.
Abate N, Garg A, Coleman R, Grundy SM, Peshock RM . Prediction of total subcutaneous abdominal, intraperitoneal, and retroperitoneal adipose tissue masses in men by a single axial magnetic resonance imaging slice. Am J Clin Nutr 1997; 65: 403–408.
Thomas EL, Brynes AE, McCarthy J, Goldstone AP, Hajnal JV, Saeed N, Frost G, Bell JD . Preferential loss of visceral fat following aerobic exercise, measured by magnetic resonance imaging. Lipids 2000; 35: 769–776.
Prentice AM, Jebb SA . Beyond body mass index. Obes Rev 2001; 2: 141–147.
Raji A, Seely EW, Arky RA, Simonson DC . Body fat distribution and insulin resistance in healthy Asian Indians and Caucasians. J Clin Endocrinol Metab 2001; 86: 5366–5371.
Greenfield JR, Samaras K, Chisholm DJ, Campbell LV . Regional intra-subject variability in abdominal adiposity limits usefulness of computer tomography. Obes Res 2002; 10: 260–265.
Acknowledgements
Financial support from the Medical Research Council and Marconi Medical Systems is gratefully acknowledged. We thank Serena Counsell and Tracey Harrington for their help and Dr Kish Bhakoo for his useful discussions regarding this work. Finally, we thank all of the volunteers who took part in this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Thomas, E., Bell, J. Influence of undersampling on magnetic resonance imaging measurements of intra-abdominal adipose tissue. Int J Obes 27, 211–218 (2003). https://doi.org/10.1038/sj.ijo.802229
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.802229
Keywords
This article is cited by
-
CT analysis of thoracolumbar body composition for estimating whole-body composition
Insights into Imaging (2023)
-
Fully automated CT-based adiposity assessment: comparison of the L1 and L3 vertebral levels for opportunistic prediction
Abdominal Radiology (2022)
-
Body composition and its association with fatigue in the first 2 years after colorectal cancer diagnosis
Journal of Cancer Survivorship (2021)
-
Comparison of single-slice CT and DXA-derived measures of central adiposity in South African women
European Journal of Clinical Nutrition (2020)
-
Abdominal subcutaneous fat quantification in obese patients from limited field-of-view MRI data
Scientific Reports (2020)