Abstract
OBJECTIVE: To examine body size and fat measurements of babies born in rural India and compare them with white Caucasian babies born in an industrialised country.
DESIGN: Community-based observational study in rural India, and comparison with data from an earlier study in the UK, measured using similar methods.
SUBJECTS: A total of 631 term babies born in six rural villages, near the city of Pune, Maharashtra, India, and 338 term babies born in the Princess Anne Hospital, Southampton, UK.
MEASUREMENTS: Maternal weight and height, and neonatal weight, length, head, mid-upper-arm and abdominal circumferences, subscapular and triceps skinfold thicknesses, and placental weight.
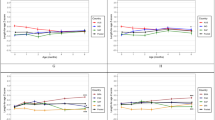
RESULTS: The Indian mothers were younger, lighter, shorter and had a lower mean body mass index (BMI) (mean age, weight, height and BMI: 21.4 y, 44.6 kg, 1.52 m, and 18.2 kg/m2) than Southampton mothers (26.8 y, 63.6 kg, 1.63 m and 23.4 kg/m2). They gave birth to lighter babies (mean birthweight: 2.7 kg compared with 3.5 kg). Compared to Southampton babies, the Indian babies were small in all body measurements, the smallest being abdominal circumference (s.d. score: −2.38; 95% CI: −2.48 to −2.29) and mid-arm circumference (s.d. score: −1.82; 95% CI: −1.89 to −1.75), while the most preserved measurement was the subscapular skinfold thickness (s.d. score: −0.53; 95% CI: −0.61 to −0.46). Skinfolds were relatively preserved in the lightest babies (below the 10th percentile of birthweight) in both populations.
CONCLUSIONS: Small Indian babies have small abdominal viscera and low muscle mass, but preserve body fat during their intrauterine development. This body composition may persist postnatally and predispose to an insulin-resistant state.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Ramachandran A, Snehalatha C, Latha E, Vijay V, Viswanathan M . Rising prevalence of NIDDM in an urban population in India. Diabetologia 1997; 40: 232–237.
Reddy KS . Cardiovascular diseases in India. World Health Stat Q 1993; 46: 101–107.
Gupta R, Gupta VP . Meta-analysis of coronary heart disease prevalence in India. Indian Heart J 1996; 48: 241–245.
Bulatao RA, Stephens PW . Global estimates and projections of mortality by cause, 1970–2015. Working Paper Series No.1007: Population and Human Resources Department, The World Bank: October 1992. Washington, DC.
Ramachandran A, Snehalatha C, Kapur A, Vijay V, Mohan V, Das AK, Rao PV, Yajnik CS, Prasanna Kumar KM, Nair JD, the Diabetes Epidemiology Study Group in India (DESI). High prevalence of diabetes and impaired glucose tolerance in India: National Urban Diabetes Survey. Diabetologia 2001; 44: 1094–1101.
King H, Aubert RE, Herman WH . Global burden of diabetes, 1995–2025; prevalence, numerical estimates and projections. Diabetes Care 1998; 21: 1414–1431.
McKeigue PM, Shah B, Marmot MG . Relation of central obesity and insulin resistance with high diabetes prevalence and cardiovascular risk in South Asians. Lancet 1991; 337: 382–386.
Yajnik CS, Naik SS, Bhat DS, Joshi VM, Shelgikar KM, Alberti KGMM, Hockaday TDR . The relationship between obesity, plasma immunoreactive insulin concentration and blood pressure in newly diagnosed Indian Type 2 diabetic patients. Diabetic Med 1993; 10: 146–151.
Shelgikar KM, Naik SS, Khopkar M, Bhat DS, Raut KN, Joglekar CV, Gerard ME, Yajnik CS . Circulating lipids and cardiovascular risk in newly diagnosed non-insulin-dependent diabetic subjects in India. Diabetic Med 1997; 14: 757–761.
Shelgikar KM, Hockaday TDR, Yajnik CS . Central rather than generalised obesity is related to hyperglycaemia in Asian Indian subjects. Diabetic Med 1991; 8: 712–717.
Chowdhury B, Helen Lantz, Lars Sjostrom . Computed tomography - determined body composition in relation to cardiovascular risk factors in Indian and matched Swedish males. Metabolism 1996; 45: 634–644
Banerji MA, Faridi N, Atluri R, Chaiken RL, Lebovitz HE . Body composition, visceral fat, leptin and insulin resistance in Asian Indian men. J Clin Endocrinol Metab 1999; 84: 137–144.
Chandalia M, Abate N, Garg A, Stray-Gundersen J, Grundy SM . Relationship between generalized and upper body obesity to insulin resistance in Asian Indian men. J Clin Endocrinol Metab 1999; 84: 2329–2335
Vaz M, Ukyab TT, Padmavathi R, Kuriyan R, Muthayya S, Diffey B, Kurpad AV . Body fat topography in Indian and Tibetan males of low and normal body mass index. Indian J Physiol Pharmacol 1999; 43: 179–185.
Neel JV . Diabetes mellitus: a ‘thrifty’ genotype rendered detrimental by ‘progress’? Am J Hum Genet 1962; 14: 353–362.
Hales CN, Barker DJP . Type 2 (non-insulin-dependent) diabetes mellitus: the thrifty phenotype hypothesis. Diabetologia 1992; 35: 595–601.
Barker DJP . Mothers, babies and health in later life. Churchill Livingstone: London, 1998.
Gopalan C . Low birth weight: significance and implications. In: Sachdev HPS, Chaudhury P, (eds). Nutrition in children; developing country concerns. Imprint: New Delhi, 1994.
Rao S, Yajnik CS, Kanade A, Fall CHD, Margetts BM, Jackson AA, Shier R, Joshi S, Rege S, Lubree H, Desai B . Intake of micronutrient-rich foods in rural Indian mothers is associated with the size of their babies at birth: Pune Maternal Nutrition Study. J Nutr 2001; 131: 1217–1224.
Kinare AS, Natekar AS, Chinchwadkar MC, Yajnik CS, Coyaji KJ, Fall CHD, Howe DT . Low midpregnancy placental volume in rural Indian women: a cause for low birth weight? Am J Obstet Gynaecol 2000; 182: 443–448.
Dewar AL . The ponderal index of the newborn infant. Dissertation for 4th year medical student research project. Department of Reproduction, University of Southampton, May 1987.
Mohan M, Shiv Prasad SR, Chellani HK, Kapani V . Intrauterine growth curves in North Indian babies: weight, length, head cir-cumference and ponderal index. Indian Pediatr 1990; 27: 43–51.
Power C . National trends in birth weight: implications for future adult disease. BMJ 1994; 308: 1270–1271.
Bonellie SR, Raab GM . Why are babies getting heavier? Comparison of Scottish births from 1980 to 1992. BMJ 1997; 35: 1205
Apte SV, Iyengar L . Composition of the human fetus. Br J Nutr 1972; 27: 305–317.
Widdowson E . Immediate and long-term consequences of being large or small at birth: a comparative approach. In: Elliot K, Knight J (eds). Size at birth. Ciba Foundation No. 27; Elsevier: Holland; 1974.
Hediger ML, Overpeck MD, Kuczmarski RJ, McGlynn A, Maurer KR, Davis WW . Muscularity and fatness of infants and young children born small or large for gestational age. Pediatrics 1998; 102: 1–6.
Loos RJF, Beunen G, Fagard R, Derom C, Vlietinck R . Birth weight and body composition in young adult men—a prospective twin study. Int J Obes Relat Metab Disord 2001; 25: 1537–1545
Humphreys MD, Holzheimer DJ . Differing influences on Aboriginal and non-Aboriginal neonatal phenotypes: a prospective study. Med J Aust 2001; 21: 503–506.
Flynn M, Goldberg G, Prentice A, Cole T . Aetiology of obesity III: critical periods for the development of obesity. In: Obesity, the report of the British Nutrition Foundation Task Force, Chapter 7. Blackwell Science: UK; 1999, pp 45–59.
Fall CHD, Yajnik CS, Rao S, Coyaji KJ . The effects of maternal body composition before pregnancy on fetal growth; The Pune Maternal Nutrition Study. In: Shaughn O'Brien PM, Wheeler T, Barker DJP (eds). Fetal programming influences on development and disease in later life, Chapter 21, RCOG: London; 1999, pp 231–245.
Auwerx J . PPARγ-the ultimate thrifty gene. Diabetologia 1999; 42: 1033–1049.
Luan J, Brownw P, Harding AH, Halsall D, O'Rahilly S, Chaterjee VK, Wareham NJ . Evidence for gene-nutrient interaction at the PPARγ locus. Diabetes 2001; 50: 686–689.
Hardy SB . Mother nature. Vintage: London, UK; 2000.
Silverman BL, Metzger BE, Cho NH, Loeb CA . Impaired glucose tolerance in adolescent offspring of diabetic mothers. Relationship to fetal hyperinsulinism. Diabetes Care 1995; 18: 611–617.
Metzger BE, Silverman BL, Freinkel N, Dooley SL, Ogata ES, Green OC . Amniotic fluid insulin concentration as a predictor of obesity. Arch Dis Childhood 1990; 65: 1050–1052.
Bavdekar A, Yajnik CS, Fall CHD, Bapat S, Pandit AN, Deshpande V, Bhave S, Kellingray SD, Joglekar C . The insulin resistance syndrome (IRS) in eight-year-old Indian children: small at birth, big at 8 years or both? Diabetes 2000; 48: 2422–2429.
Fall CHD, Stein CE, Kumaran K, Cox V, Osmond C, Barker DJP, Hales CN . Size at birth, maternal weight, and type 2 diabetes in South India. Diabetic Med 1998; 15: 220–227.
Bjorntorp P . Adipose tissue distribution and function. Int J Obes Relat Metab Disord 1991; 15: 67–81.
Mohamed-Ali V, Goodrick S, Rawesh A, Miles JM, Katz D, Yudkin JS, Coppack SW . Human subcutaneous adipose tissue secretes interleukin-6 but not tumour necrosis factor-α in vivo. J Clin Endocrinol Metab 1997; 82: 4196–4200
Hotamisligil GS, Spiegelman BM . Tumour necrosis factor-α: a key component of the obesity-diabetes link. Diabetes 1994; 43: 1271–1278.
Yajnik CS, Sardesai BS, Bhat DS, Naik SS, Raut KN, Shelgikar KM, Orskov H, Alberti KGMM, Hockaday TDR . The ketosis- resistance in fibro-calculous pancreatic diabetes. 2. Hepatic ketogenesis after oral medium chain triglycerides. Metabolism 1997; 46: 1–4.
Kulkarni RN, Kurpad AV, Shetty PS . Reduced postexercise recovery oxygen consumptions: an adaptive response in chronic energy deficiency?. Metabolism 1993; 42: 544–547.
Kulkarni RN, Shetty PS . Net mechanical efficiency during stepping in chronically energy-deficient human subjects. Ann Hum Biol. 1992; 19: 421–425.
Hattersley A, Beards F, Ballantyne et al. Mutations in the glucokinase gene in the fetus result in reduced birthweight. Nat Gene 1998; 19: 268–270.
Klebanoff MA, Mednick BR, Schulsinger C, Secher NJ, Shiono PH . Father's effect on infant birth weight. Am J Obstet Gynecol 1998; 178: 1022–1026.
Acknowledgements
We are grateful to the community, in particular the pregnant women and their families, for taking part in this study. We would also like to thank Dr Mrs Banoo Coyaji, Director of the KEM Hospital, Pune, and initiator 25 years ago of the rural primary healthcare programme in the study area. We acknowledge the major contributions made to the study by Dr Arun Kinare, Dr Monesh Shah, Dr Asit Natekar, Dr Manoj Chinchwadkar, Dr Binu John, Dr Anuja Bisht, Dr Mahananda Bhavikatti, Dr Asawari Kanade, Mrs Punam Gupta, Mrs Parveen Bharucha, Miss Vanessa Cox and Dr Barrie Margetts. We also thank Mr Tim Wheeler, Reader in Obstetrics and Gynaecology, Princess Anne Hospital, Southampton, UK, for the Southampton data. The study was funded by the Wellcome Trust, London, UK, the Medical Research Council, UK and SNEHA, India.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yajnik, C., Fall, C., Coyaji, K. et al. Neonatal anthropometry: the thin–fat Indian baby. The Pune Maternal Nutrition Study. Int J Obes 27, 173–180 (2003). https://doi.org/10.1038/sj.ijo.802219
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ijo.802219
Keywords
This article is cited by
-
Neonatal adiposity is associated with microRNAs in adipocyte-derived extracellular vesicles in maternal and cord blood, a discovery analysis
International Journal of Obesity (2024)
-
Body composition from birth to 2 years
European Journal of Clinical Nutrition (2023)
-
Can the triglyceride-glucose index predict insulin resistance in LGA newborns?
Journal of Perinatology (2023)
-
Association between maternal hyperglycemia in pregnancy and offspring anthropometry in early childhood: the pandora wave 1 study
International Journal of Obesity (2023)
-
Gestational age specific anthropometric postnatal percentile charts for neonates born at tertiary hospital in Eastern Nepal
BMC Pediatrics (2022)