Abstract
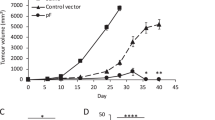
Modified vaccinia virus Ankara (MVA) has been used successfully to express various antigens for the development of vaccines. Here we show that MVA can also be used as an efficient vector for the transfer of suicide genes to cancer cells. We have generated a new and highly potent suicide gene, FCU1, which encodes a fusion protein derived from the yeast cytosine deaminase and uracil phosphoribosyltransferase genes. We now describe the therapeutic benefit of using MVA to deliver and express the FCU1 gene in cancer cells. MVA-mediated transfer of the FCU1 gene to various human tumor cells results in the production of a bifunctional intracellular enzyme, such that exposure to the prodrug 5-FC suppresses the growth of the tumor cells both in vitro and in vivo. Moreover, we report a more potent tumor growth delay at lower doses of 5-FC using MVA-FCU1 in comparison to adenovirus encoding FCU1. Prolonged therapeutic levels of cytotoxic 5-FU were detected in tumors in mice treated with both MVA-FCU1 and 5-FC while no detectable 5-FU was found in the circulation. This original combination between MVA and FCU1 represents a potentially safe and attractive therapeutic option to test in man.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Mullen CA, Kilstrup M, Blaese RM . Transfer of the bacterial gene for cytosine deaminase to mammalian cells confers lethal sensitivity to 5-fluorocytosine: a negative selection system. Proc Natl Acad Sci USA 1992; 89: 33–37.
Hirschowitz EA, Ohwada A, Pascal WR, Russi TJ, Crystal RG . In vivo adenovirus-mediated gene transfer of the Escherichia coli cytosine deaminase gene to human colon carcinoma-derived tumors induces chemosensitivity to 5-fluorocytosine. Hum Gene Ther 1995; 6: 1055–1063.
Kanai F, Lan KH, Shiratori Y, Tanaka T, Ohashi M, Okudaira T et al. In vivo gene therapy for alpha-fetoprotein-producing hepatocellular carcinoma by adenovirus-mediated transfer of cytosine deaminase gene. Cancer Res 1997; 57: 461–465.
Huber BE, Austin EA, Richards CA, Davis ST, Good SS . Metabolism of 5-fluorocytosine to 5-fluorouracil in human colorectal tumor cells transduced with the cytosine deaminase gene: significant antitumor effects when only a small percentage of tumor cells express cytosine deaminase. Proc Natl Acad Sci USA 1994; 91: 8302–8306.
Miller CR, Williams CR, Buchsbaum DJ, Gillespie GY . Intratumoral 5-fluorouracil produced by cytosine deaminase/5-fluorocytosine gene therapy is effective for experimental human glioblastomas. Cancer Res 2002; 62: 773–780.
Lee CH, Wu CL, Shiau AL . Hypoxia-induced cytosine deaminase gene expression for cancer therapy. Hum Gene Ther 2007; 18: 27–38.
Guffey MB, Parker JN, Luckett Jr WS, Gillespie GY, Meleth S, Whitley RJ et al. Engineered herpes simplex virus expressing bacterial cytosine deaminase for experimental therapy of brain tumors. Cancer Gene Ther 2007; 14: 45–56.
Erbs P, Exinger F, Jund R . Characterization of the Saccharomyces cerevisiae FCY1 gene encoding cytosine deaminase and its homologue FCA1 of Candida albicans. Curr Genet 1997; 31: 1–6.
Danielsen S, Kilstrup M, Barilla K, Jochimsen B, Neuhard J . Characterization of the Escherichia coli codBA operon encoding cytosine permease and cytosine deaminase. Mol Microbiol 1992; 6: 1335–1344.
Koechlin BA, Rubio F, Palmer S, Gabriel T, Duschinsky R . The metabolism of 5-fluorocytosine-2-14-C and of cytosine-14-C in the rat and the disposition of 5-fluorocytosine-2-14-C in man. Biochem Pharmacol 1966; 15: 435–446.
Andersen PS, Smith JM, Mygind B . Characterization of the upp gene encoding uracil phosphoribosyltransferase of Escherichia coli K12. Eur J Biochem 1992; 204: 51–56.
Kern L, de Montigny J, Jund R, Lacroute F . The FUR1 gene of Saccharomyces cerevisiae: cloning, structure and expression of wild-type and mutant alleles. Gene 1990; 88: 149–157.
Kanai F, Kawakami T, Hamada H, Sadata A, Yoshida Y, Tanaka T et al. Adenovirus-mediated transduction of Escherichia coli uracil phosphoribosyltransferase gene sensitizes cancer cells to low concentrations of 5-fluorouracil. Cancer Res 1998; 58: 1946–1951.
Erbs P, Regulier E, Kintz J, Leroy P, Poitevin Y, Exinger F et al. In vivo cancer gene therapy by adenovirus-mediated transfer of a bifunctional yeast cytosine deaminase/uracil phosphoribosyltransferase fusion gene. Cancer Res 2000; 60: 3813–3822.
Trinh QT, Austin EA, Murray DM, Knick VC, Huber BE . Enzyme/prodrug gene therapy: comparison of cytosine deaminase/5-fluorocytosine versus thymidine kinase/ganciclovir enzyme/prodrug systems in a human colorectal carcinoma cell line. Cancer Res 1995; 55: 4808–4812.
Mesnil M, Piccoli C, Tiraby G, Willecke K, Yamasaki H . Bystander killing of cancer cells by herpes simplex virus thymidine kinase gene is mediated by connexins. Proc Natl Acad Sci USA 1996; 93: 1831–1835.
Matono S, Tanaka T, Sueyoshi S, Yamana H, Fujita H, Shirouzu K . Bystander effect in suicide gene therapy is directly proportional to the degree of gap junctional intercellular communication in esophageal cancer. Int J Oncol 2003; 23: 1309–1315.
Mayr A, Stickl H, Muller HK, Danner K, Singer H . The smallpox vaccination strain MVA: marker, genetic structure, experience gained with the parenteral vaccination and behavior in organisms with a debilitated defence mechanism (author's translation). Zentralbl Bakteriol [B] 1978; 167: 375–390 (in German).
Stickl H, Hochstein-Mintzel V, Mayr A, Huber HC, Schafer H, Holzner A . MVA vaccination against smallpox: clinical tests with an attenuated live vaccinia virus strain (MVA) (author's translation). Dtsch Med Wochenschr 1974; 99: 2386–2392 (in German).
Sutter G, Moss B . Nonreplicating vaccinia vector efficiently expresses recombinant genes. Proc Natl Acad Sci USA 1992; 89: 10847–10851.
Chakrabarti S, Sisler JR, Moss B . Compact, synthetic, vaccinia virus early/late promoter for protein expression. Biotechniques 1997; 23: 1094–1097.
Puhlmann M, Gnant M, Brown CK, Alexander HR, Bartlett DL . Thymidine kinase-deleted vaccinia virus expressing purine nucleoside phosphorylase as a vector for tumor-directed gene therapy. Hum Gene Ther 1999; 10: 649–657.
Cochran MA, Puckett C, Moss B . In vitro mutagenesis of the promoter region of vaccinia virus gene: evidence for tandem early and late regulatory signals. J Virol 1985; 54: 30–37.
Rosel JL, Earl PL, Weir JP, Moss B . Conserved TAAATG sequence at the transcriptional and translational initiation sites of vaccinia virus late genes deduced by structural and functional analysis of the HindIII H genome fragment. J Virol 1986; 60: 436–439.
Falkner F, Moss B . Escherichia coli gpt gene provides dominant selection for vaccinia virus open reading frame expression vectors. J Virol 1988; 62: 1849–1854.
Spehner D, Drillien R, Proamer F, Houssais-Pecheur C, Zanta MA, Geist M et al. Enveloped virus is the major virus form produced during productive infection with the modified vaccinia virus Ankara strain. Virology 2000; 273: 9–15.
Ramirez JC, Gherardi MM, Esteban M . Biology of attenuated modified vaccinia virus Ankara recombinant vector in mice: virus fate and activation of B- and T-cell immune responses in comparison with the Western Reserve strain and advantages as a vaccine. J Virol 2000; 74: 923–933.
Stittelaar KJ, Kuiken T, de Swart RL, van Amerongen G, Vos HW, Niesters HG et al. Safety of modified vaccinia virus Ankara (MVA) in immune-suppressed macaques. Vaccine 2001; 19: 3700–3709.
Sutter G, Staib C . Vaccinia vectors as candidate vaccines: the development of modified vaccinia virus Ankara for antigen delivery. Curr Drug Targets Infect Disord 2003; 3: 263–271.
Taylor J, Weinberg R, Tartaglia J, Richardson C, Alkhatib G, Briedis D et al. Nonreplicating viral vectors as potential vaccines: recombinant canarypox virus expressing measles virus fusion (F) and hemagglutinin (HA) glycoproteins. Virology 1992; 187: 321–328.
Tartaglia J, Perkus ME, Taylor J, Norton EK, Audonnet JC, Cox WI et al. NYVAC: a highly attenuated strain of vaccinia virus. Virology 1992; 188: 217–232.
Pederson LC, Buchsbaum DJ, Vickers SM, Kancharla SR, Mayo MS, Curiel DT et al. Molecular chemotherapy combined with radiation therapy enhances killing of cholangiocarcinoma cells in vitro and in vivo. Cancer Res 1997; 57: 4325–4332.
Lambin P, Nuyts S, Landuyt W, Theys J, De Bruijn E, Anne J et al. The potential therapeutic gain of radiation-associated gene therapy with the suicide gene cytosine deaminase. Int J Radiat Biol 2000; 76: 285–293.
Kievit E, Bershad E, Ng E, Sethna P, Dev I, Lawrence TS et al. Superiority of yeast over bacterial cytosine deaminase for enzyme/prodrug gene therapy in colon cancer xenografts. Cancer Res 1999; 59: 1417–1421.
Hamstra DA, Rice DJ, Fahmy S, Ross BD, Rehemtulla A . Enzyme/prodrug therapy for head and neck cancer using a catalytically superior cytosine deaminase. Hum Gene Ther 1999; 10: 1993–2003.
Hamstra DA, Lee KC, Tychewicz JM, Schepkin VD, Moffat BA, Chen M et al. The use of 19F spectroscopy and diffusion-weighted MRI to evaluate differences in gene-dependent enzyme prodrug therapies. Mol Ther 2004; 10: 916–928.
Wolf W, Presant CA, Servis KL, el-Tahtawy A, Albright MJ, Barker PB et al. Tumor trapping of 5-fluorouracil: in vivo 19F NMR spectroscopic pharmacokinetics in tumor-bearing humans and rabbits. Proc Natl Acad Sci USA 1990; 87: 492–496.
Presant CA, Wolf W, Waluch V, Wiseman C, Kennedy P, Blayney D et al. Association of intratumoral pharmacokinetics of fluorouracil with clinical response. Lancet 1994; 343: 1184–1187.
Presant CA, Jacobson J, Wolf W, Waluch V, Weitz IC, Macdonald JS . Does leucovorin alter the intratumoral pharmacokinetics of 5-fluorouracil (5-FU)? A Southwest Oncology Group study. Invest New Drugs 2002; 20: 369–376.
Edwards Jr JE, Bodey GP, Bowden RA, Buchner T, de Pauw BE, Filler SG et al. International conference for the development of a consensus on the management and prevention of severe candidal infections. Clin Infect Dis 1997; 25: 43–59.
Kievit E, Nyati MK, Ng E, Stegman LD, Parsels J, Ross BD et al. Yeast cytosine deaminase improves radiosensitization and bystander effect by 5-fluorocytosine of human colorectal cancer xenografts. Cancer Res 2000; 60: 6649–6655.
Kambara H, Tamiya T, Ono Y, Ohtsuka S, Terada K, Adachi Y et al. Combined radiation and gene therapy for brain tumors with adenovirus-mediated transfer of cytosine deaminase and uracil phosphoribosyltransferase genes. Cancer Gene Ther 2002; 9: 840–845.
Acknowledgements
We thank R Wittek (University of Lausanne, Switzerland) for providing the synthetic vaccinia p11K7.5 promoter. We thank Y Schlesinger and D Villeval for their technical assistance. We would like to acknowledge the help and scientific criticisms of B. Acres during the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Erbs, P., Findeli, A., Kintz, J. et al. Modified vaccinia virus Ankara as a vector for suicide gene therapy. Cancer Gene Ther 15, 18–28 (2008). https://doi.org/10.1038/sj.cgt.7701098
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cgt.7701098
Keywords
This article is cited by
-
Safety, biodistribution and viral shedding of oncolytic vaccinia virus TG6002 administered intravenously in healthy beagle dogs
Scientific Reports (2021)
-
Polymeric Cups for Cavitation-mediated Delivery of Oncolytic Vaccinia Virus
Molecular Therapy (2016)
-
Enhanced tumor therapy using vaccinia virus strain GLV-1h68 in combination with a β-galactosidase-activatable prodrug seco-analog of duocarmycin SA
Cancer Gene Therapy (2011)
-
Targeted delivery of a suicide gene to human colorectal tumors by a conditionally replicating vaccinia virus
Gene Therapy (2008)