Abstract
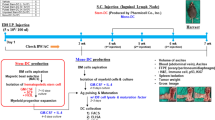
Purpose: Triggering of CD40 on antigen-presenting cells via its ligand CD154 is an important event in the initial phase of an immune response against cancer cells. In this study, we investigated the effects of adenoviral CD154 immunomodulatory gene therapy on the activation of human dendritic cells (DCs) in a well-defined in vitro system. Experimental design: Human bladder cancer cell lines and tumor cells from patients with renal cell carcinoma (RCC) were transduced with Ad-CD154 vectors or control vectors. Activation of human in vitro generated DCs after coculture with transduced tumor cells was analyzed. Therapeutic efficacy and cytotoxic T-lymphocyte (CTL) activity were assessed in a subcutaneous (s.c.) murine bladder cancer model. Results: Human bladder cancer cell lines expressing CD154 showed a decreased growth rate, increased apoptosis, and modulated expression of molecules important for recognition by cytotoxic lymphocytes. Further, CD154-expressing allogeneic bladder tumor cell lines and autologous tumor cells from patients with renal cell cancer induced maturation of DCs and stimulated IFN-γ production from lymphocytes cocultured with mature DCs. In vivo studies showed that CD154 gene therapy was highly effective in wild-type mice but only minimally effective in nude mice. Consequently, strong tumor-specific CTL activity was detected in mice vaccinated with tumor cells expressing CD154. Conclusions: Using tumor cell lines as well as patient-derived material, we could show that tumor cells expressing CD154 efficiently induce maturation and activation of DCs as well as activation of lymphocytes. Our murine in vivo studies demonstrate that lymphocytes contribute to the observed antitumor effect in a s.c. bladder tumor model. These studies should stimulate CD154 gene therapy approaches for the treatment of urologic malignancies.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout








Similar content being viewed by others
References
Gilboa E . How tumors escape immune destruction and what we can do about it Cancer Immunol Immunother 1999 48: 382–385
Ostrand-Rosenberg S . Tumor immunotherapy: the tumor cell as an antigen-presenting cell Curr Opin Immunol 1994 6: 722–727
Sogn JA . Tumor immunology: the glass is half full Immunity 1998 9: 757–763
Banchereau J, Briere F, Caus C et al. Immunobiology of dendritic cells Annu Rev Immunol 2000 18: 767–811
Lanzavecchia A, Sallusto F . Regulation of T cell immunity by dendritic cells Cell 2001 106: 263–266
Lanzavecchia A . Licence to kill Nature 1998 393: 413–414
Cella M, Scheidegger D, Palmer-Lehmann K et al. Ligation of CD40 on dendritic cells triggers production of high levels of interleukin-12 and enhances T cell stimulatory capacity: T–T help via APC activation J Exp Med 1996 184: 747–752
Bennett SRM, Carbone FR, Karamalis F et al. Help for cytotoxic-T-cell responses is mediated by CD40 signaling Nature 1998 393: 478–480
Schoenberger SP, Toes REM, van der Voort EIH et al. T-cell help for cytotoxic T lymphocytes is mediated by CD40–CD40L interactions Nature 1998 393: 480–483
Kikuchi T, Moore MSA, Crystal RG . Dendritic cells modified to express CD40 ligand elicit therapeutic immunity against preexisting murine tumors Blood 2000 96: 91–99
Klein C, Bueler H, Mulligan RC . Comparative analysis of genetically modified dendritic cells and tumor cells as therapeutic cancer vaccines J Exp Med 2000 191: 1699–1708
Dallal RM, Lotze MT . The dendritic cell and human cancer vaccines Curr Opin Immunol 2000 12: 583–588
Fong L, Engelmann EG . Dendritic cells in cancer immunotherapy Annu Rev Immunol 2000 18: 245–273
Dilloo D, Brown M, Roskrow M et al. CD40 ligand induces an antileukemia immune response in vivo Blood 1997 5: 1927–1933
Chiodoni C, Paglia P, Stoppacciaro A et al. Dendritic cells infiltrating tumors cotransduced with granulocyte/macrophage colony stimulating factor (GM-CSF) and CD40 ligand genes takes up and present endogenous tumor-associated antigen, and prime naïve mice for a cytotoxic T lymphocyte response J Exp Med 1999 190: 125–133
Sun Y, Peng D, Lecanda J et al. In vivo gene transfer of CD40 ligand into colon cancer cells induces local production of cytokines and chemokines, tumor eradication and protective antitumor immunity Gene Ther 2000 7: 1467–1476
Loskog A, Björkland A, Brown MP et al. Potent antitumor effects of CD154 transduced tumor cells in experimental bladder cancer J Urol 2001 166: 1093–1097
Kato K, Cantwell MJ, Sharma S, Kipps TJ . Gene transfer of CD40L induces autologous immune recognition of chronic lymphocytic leukemia B-cells J Clin Invest 1998 101: 1133–1141
Wierda WG, Cantwell MJ, Woods SJ et al. CD40-ligand (CD154) gene therapy for chronic lymphocytic leukemia Blood 2000 96: 2917–2924
Yamada M, Shiroko T, Kawaguchi Y et al. CD40–CD40 ligand (CD154) engagement is required but not sufficient for modulating MHC class I, ICAM-1, and Fas expression and proliferation of human non-small cell lung tumors Int J Cancer 2001 4: 589–599
von Leoprechting A, van der Bruggen P, Pahl HL et al. Stimulation of CD40 on immunogenic human malignant melanomas augments their cytotoxic T lymphocyte-mediated lysis and induced apoptosis Cancer Res 1999 59: 1287–1294
Bergamo A, Bataille R, Pellat-Deceunynck C . CD40 and CD95 induce programmed cell death in the human myeloma cell line XG2 Br J Haematol 1997 3: 652–655
Hess S, Engelmann H . A novel function of CD40: induction of cell death in transformed cells J Exp Med 1996 183: 159–167
Alexandroff AB, Jackson AM, Paterson T et al. Role for CD40–CD40 ligand interactions in the immune response to solid tumours Mol Immunol 2000 37: 515–526
Hay RJ, Park J-G, Gazdar A . Cell lines form urinary bladder tumors In: Johansson SL, Unsgaard B, O'Toole CM, eds Atlas of Human Tumor Cell Lines New York: Academic Press 1994 341
Ahmed SA, Gogal RM Jr, Walsh JE . A new rapid and simple non-radioactive assay to monitor and determine the proliferation of lymphocytes: an alternative to 3H thymidine incorporation assay J Immunol Methods 1994 170: 211–224
Pantuck AJ, Zisman A, Belldegrun A . Gene and immune therapy for renal cell carcinoma Int J Urol 2001 166: 1611–1623
Rubartelli A, Poggi A, Zocchi MR . The selective engulfment of apoptotic bodies by dendritic cells is mediated by the αvβ3 integrin and requires intracellular and extracellular calcium Eur J Immunol 1997 27: 1893–1900
Albert ML, Sauter B, Bhardwaj N . Dendritic cells acquire antigen from apoptotic cells and induce class I-restricted CTLs Nature 1998 392: 86–89
van Kooten C, Banchereau J . CD40–CD40 ligand J Leukoc Biol 2000 67: 2–17
Cella M, Sallusto F, Lanzavecchia A . Origin, maturation and antigen presenting function of dendritic cells Curr Opin Immunol 1997 9: 10–16
Acknowledgements
This study was supported by The Swedish Cancer Society, the Lions' Cancer Fund at Uppsala University Hospital, and Deutsche Forschungsgemeinschaft SFB 367. The authors thank Gabriele Bentien (Research Center Borstel) for excellent technical assistance and the colleagues from the Department of Urology at the Medical University of Lübeck for providing tumor tissue and peripheral blood of patients with RCC.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Loskog, A., Tötterman, T., Böhle, A. et al. In vitro activation of cancer patient–derived dendritic cells by tumor cells genetically modified to express CD154. Cancer Gene Ther 9, 846–853 (2002). https://doi.org/10.1038/sj.cgt.7700507
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.cgt.7700507
Keywords
This article is cited by
-
Non-stem bladder cancer cell-derived extracellular vesicles promote cancer stem cell survival in response to chemotherapy
Stem Cell Research & Therapy (2021)
-
Enhanced metastatic potential in the MB49 urothelial carcinoma model
Scientific Reports (2019)
-
Activation of myeloid and endothelial cells by CD40L gene therapy supports T-cell expansion and migration into the tumor microenvironment
Gene Therapy (2017)
-
Immunotherapy for superficial bladder cancer
Cancer Immunology, Immunotherapy (2005)
-
Functional transfer of CD40L gene in human B-cell precursor ALL blasts by second-generation SIN lentivectors
Gene Therapy (2004)