Abstract
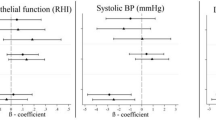
Previous studies have shown an association between elevated concentrations of particulate air pollution and cardiovascular morbidity and mortality. Therefore, the association between daily variation of ultrafine and fine particulate air pollution and cardiac autonomic control measured as heart rate variability (HRV) was studied in a large multicenter study in Amsterdam, the Netherlands, Erfurt, Germany, and Helsinki, Finland. Elderly subjects (n=37 in Amsterdam, n=47 in both Erfurt and Helsinki) with stable coronary artery disease were followed for 6 months with biweekly clinical visits. During the visits, ambulatory electrocardiogram was recorded during a standardized protocol including a 5-min period of paced breathing. Time and frequency domain analyses of HRV were performed. A statistical model was built for each center separately. The mean 24-h particle number concentration (NC) (1000/cm3) of ultrafine particles (diameter 0.01–0.1 μm) was 17.3 in Amsterdam, 21.1 in Erfurt, and 17.0 in Helsinki. The corresponding values for PM2.5 were 20.0, 23.1, and 12.7 μg/m3. During paced breathing, ultrafine particles, NO2, and CO were at lags of 0–2 days consistently and significantly associated with decreased low-to-high frequency ratio (LF/HF), a measure of sympathovagal balance. In a pooled analysis across the centers, LF/HF decreased by 13.5% (95% confidence interval: −20.1%, −7.0%) for each 10,000/cm3 increase in the NC of ultrafine particles (2-day lag). PM2.5 was associated with reduced HF and increased LF/HF in Helsinki, whereas the opposite was true in Erfurt, and in Amsterdam, there were no clear associations between PM2.5 and HRV. The results suggest that the cardiovascular effects of ambient ultrafine and PM2.5 can differ from each other and that their effect may be modified by the characteristics of the exposed subjects and the sources of PM2.5.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 6 print issues and online access
$259.00 per year
only $43.17 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Berkey C.S., and Laird N.M. Nonlinear growth curve analysis: estimating the population parameters. Ann Hum Biol 1986: 13: 111–128.
Brunekreef B., and Holgate S.T. Air pollution and health. Lancet 2002: 360: 1233–1242.
Creason J., et al. Particulate matter and heart rate variability among elderly retirees: the Baltimore 1998 PM study. J Expo Anal Environ Epidemiol 2001: 11: 116–122.
Devlin R.B., et al. Elderly humans exposed to concentrated air pollution particles have decreased heart rate variability. Eur Respir J 2003: 21(Suppl. 40): 76s–80s.
Dominici F., et al. National Maps of the effects of particulate matter on mortality: exploring geographical variation. Environ Health Perspect 2003: 111: 39–43.
Eckberg D.L. Sympathovagal balance. A critical appraisal. Circulation 1997: 96: 3224–3232.
Godleski J.J., et al. Mechanisms of morbidity and mortality from exposure to ambient air particles. HEI research report no. 91, Cambridge, MA, USA, 2000.
Gold D.R., et al. Ambient pollution and heart rate variability. Circulation 2000: 101: 1267–1273.
de Hartog J.J., et al. Size distribution on particulate matter in three European cities. J Environ Monit 2005: 4: 302–310.
Holguin F., et al. Air pollution and heart rate variability among the elderly in Mexico City. Epidemiology 2003: 14: 521–527.
Houle M.S., and Billman G.E. Low-frequency component of the heart rate variability spectrum: a poor marker of sympathetic activity. Am J Physiol Heart Circ Physiol 1999: 276: H215–H223.
Huikuri H.V., and Makikallio T.H. Heart rate variability in ischaemic heart disease. Auton Neurosci 2001: 90: 95–101.
Ibald-Mulli A., et al. Effects of particulate air pollution on blood pressure and heart rate in subjects with cardiovascular disease: a multicenter approach. Environ Health Perspect 2004: 112: 369–377.
Janssen N.A.H., et al. Personal exposure to fine particulate matter in elderly subjects: relation between personal, indoor and outdoor concentrations. J Air Waste Management Assoc 2000: 50: 1133–1143.
Katsoyanni K., et al. Confounding and effect modification in the short-term effects of ambient particles on total mortality: results from 29 European cities within the APHEA2 project. Epidemiology 2001: 5: 521–531.
Kawaguchi T., et al. Predictors of disease severity and survival in patients with coronary artery disease. Coronary Artery Dis 1993: 4: 971–980.
Khlystov A., et al. Intercomparison using laboratory-generated aerosols. Atmos Environ 2001: 35: 2045–2051.
Lai S., et al. Treadmill scores in elderly men. J Am Coll Cardiol 2004: 43: 606–615.
Liao D., et al. Daily variation of particulate air pollution and poor cardiac autonomic control in the elderly. Environ Health Perspect 1999: 107: 521–525.
Littell R.C., et al. SAS® System for Mixed Models. SAS Institute Inc., Cary, NC, 1999.
Malliani A. The pattern of sympathovagal balance explored in the frequency domain. News Physiol Sci 1999: 14: 111–117.
Nemmar A., et al. Passage of inhaled particles into the blood circulation in humans. Circulation 2002: 105: 411–414.
Normand, S.-L.T. Tutorial in biostatistics. Meta-analysis: formulating, evaluating, combining, and reporting. Statist Med 1999: 18: 321–359.
Pekkanen J., et al. ULTRA. Exposure and Risk Assessment for Fine and Ultrafine Particles in Ambient Air. Study Manual and Data book. Publications of National Public Health Institute B9/2000, Kuopio, 2000 Available: http://www.ktl.fi/ultra.
Pekkanen J., et al. Particulate air pollution and risk of ST-segment depression during repeated submaximal exercise tests among subjects with coronary heart disease. The Exposure and risk assessment for fine and ultrafine particles in ambient air (ULTRA) study. Circulation 2002: 106: 933–938.
Pope III C.A., et al. Heart rate variability associated with particulate air pollution. Am Heart J 1999: 138: 890–899.
Pope III C.A., et al. Ambient particulate air pollution, heart rate variability, and blood markers of inflammation in a panel of elderly subjects. Environ Health Perspect 2004: 112: 339–345.
Ruuskanen J., et al. Concentrations of ultrafine, fine and PM2.5 particles in three European cities. Atmos Environ 2001: 35: 3729–3738.
Samet J.M., et al. Fine particulate air pollution and mortality in 20 US Cities, 1987–1994. N Engl J Med 2000: 343: 1742–1749.
Samoli E., et al. Investigating regional differences in short-term effects of air pollution on daily mortality in the APHEA project: a sensitivity analysis for controlling long-term trends and seasonality. Environ Health Perspect 2001: 109: 349–353.
SAS Institute Inc. SAS/STAT® Software: Changes and Enhancements through Release 6.11. SAS Institute Inc., Cary, NC, 1989, pp. 531–656.
Schwartz J. Air pollution and hospital admissions for heart disease in eight US counties. Epidemiology 1999: 10: 17–22.
Seaton A., et al. Particulate air pollution and acute health effects. Lancet 1995: 345: 176–178.
S-PLUS 2000. Guide to Statistics, Vol. 1. Data Analysis Products Division, Mathsoft, Seattle, WA, 1999, pp. 326–327.
Stone P.H., and Godleski J.J. First steps toward understanding the pathophysiologic link between air pollution and cardiac mortality. Am Heart J 1999: 138: 804–807.
Tarkiainen T., et al. Effect of acute carbon monoxide exposure on heart rate variability in patients with coronary artery disease. Clin Physiol Funct Imaging 2003: 23: 98–102.
Task Force of The European Society of Cardiology and The North American Society of Pacing and Electrophysiology. Heart rate variability. Standards of measurement, physiological interpretation and clinical use. Circulation 1996: 93: 1043–1065.
Tsuji H., et al. Reduced heart rate variability and mortality risk in an elderly cohort. The Framingham Heart Study. Circulation 1994: 90: 878–883.
Tuch T., et al. Comparison of two particle size spectrometers for ambient aerosol measurements in environmental epidemiology. Atmos Environ 2000: 34: 139–149.
Vallius M., et al. Sources and elemental composition of ambient PM2.5 in three European cities. Sci Total Environ 2005: 337: 147–162.
Watkinson W.P., et al. Cardiac arrhythmia induction after exposure to residual oil fly ash particles in a rodent model of pulmonary hypertension. Toxicol Sci 1998: 41: 209–216.
Acknowledgements
The study was carried out within the framework of the “Exposure and risk assessment for fine and ultrafine particles in ambient air”(ULTRA) project. The project was funded by the EU ENVIRONMENT and CLIMATE Research Programme Contract ENV4-CT97-0568. The project was coordinated by the Unit of Environmental Epidemiology, National Public Health Institute, PO Box 95, Kuopio 70701, Finland with funding also from Academy of Finland, the Centre of Excellence Programme 2002–2007 of the Academy of Finland (Contract 53307), and the National Technology Fund (TEKES, Contract 40715/01). Dr. Gold was supported by EPA 826780-01-0 and NIH PO1 ES09825. The contribution of following persons and institutions to the field work of the project is gratefully acknowledged: Helsinki: Aadu Mirme, Ph.D., Gintautas Buzorius, Ph.D., Ismo Koponen, M.Sc., Marko Vallius, M.Sc., Sami Penttinen, Kati Oravisjärvi, Annalea Lohila, M.Sc., Anita Tyrväinen, Helsinki Metropolitan Area Council, Helsinki (Päivi Aarnio, Lic Tech., and Tarja Koskentalo, Lic Tech.), and the Finnish Heart Association. Erfurt: Gabi Wölke, M.A., Martina Stadeler, M.D., Regina Müller, Cornelia Engel, Thomas Tuch, Ph.D., and Sabine Koett, Klaus Koschine, Mike Pitz, MA. Amsterdam: Andrey Khlystov, Ph.D., Gerard Kos, Carolien Mommers, M.Sc., Marloes Jongeneel, M.Sc., Boukje de Wit, Isabella van Schothorst, Veronique van den Beuken, M.Sc., Marieke Oldenwening, Nicole Janssen, Ph.D., Jean Pierre van Mulken, and Environmental Medicine, Municipal Health Service Amsterdam (Saskia van der Zee, Ph.D., Willem Roemer, Ph.D., and Joop van Wijnen, M.D.).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Timonen, K., Vanninen, E., de Hartog, J. et al. Effects of ultrafine and fine particulate and gaseous air pollution on cardiac autonomic control in subjects with coronary artery disease: The ULTRA study. J Expo Sci Environ Epidemiol 16, 332–341 (2006). https://doi.org/10.1038/sj.jea.7500460
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jea.7500460
Keywords
This article is cited by
-
Inhalation of printer-emitted particles impairs cardiac conduction, hemodynamics, and autonomic regulation and induces arrhythmia and electrical remodeling in rats
Particle and Fibre Toxicology (2020)
-
Acute effect of ambient fine particulate matter on heart rate variability: an updated systematic review and meta-analysis of panel studies
Environmental Health and Preventive Medicine (2020)
-
Large-scale blow spinning of heat-resistant nanofibrous air filters
Nano Research (2020)
-
Transparent Polyurethane Nanofiber Air Filter for High-Efficiency PM2.5 Capture
Nanoscale Research Letters (2019)
-
Longitudinal follow-up of health effects among workers handling engineered nanomaterials: a panel study
Environmental Health (2019)