Abstract
Objective:
The primary aim of this study was to determine if an association exists between amino-acid levels and development of cholestasis. The secondary aim of our amino-acid dose comparison trial was to identify factors associated with the development of prolonged cholestatic jaundice.
Study Design:
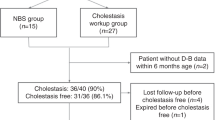
We compared demographic characteristics and amino-acid levels in neonates who developed cholestasis with those who did not. Parenteral-associated cholestatic liver disease was defined as a direct serum bilirubin above 5 mg per 100 ml any time during the first 28 days after birth in neonates with no history of biliary atresia or viral hepatitis. We obtained filter paper blood spots for amino acid and acylcarnitine measurements on the day of randomization and days 7 and 28 of age to identify a profile of values that could be used to identify neonates with evidence of abnormal liver function.
Result:
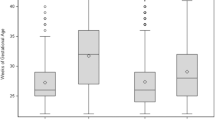
We enrolled 122 neonates in our study; 13 (10.7%) developed cholestasis. Neonates who developed cholestasis were more immature, had lower birth weight, were exposed to parenteral nutrition for a longer period, had a higher cumulative dose of amino acids, were less often on enteral nutrition by day 7 of age, more often had a patent ductus arteriosus and severe intraventricular hemorrhage and were more commonly treated with steroids by 28 days of age. Amino acid and acylcarnitine values were not different for the two groups on the day of randomization. On day 7 (parenteral phase of nutrition), blood urea nitrogen, citrulline, histidine, methionine and succinyl carnitine were higher, and serine, glutamate and thyroxine levels were lower in the neonates who developed cholestasis than in who did not.
Conclusion:
Cholestasis remains an important complication of parenteral nutrition, and several clinical and biochemical factors may be helpful in identifying high-risk patients.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Venigalla S, Gourley GR . Neonatal cholestasis. Semin Perinatol 2004; 28: 348–355.
Emerick KM, Whitington PF . Molecular basis of neonatal cholestasis. Pediatr Clin North Am 2002; 49: 221–235.
Karpen SJ . Update on the etiologies and management of neonatal cholestasis. Clin Perinatol 2002; 29: 159–180.
Peden VH, Witzleben CL, Skelton MA . Total parenteral nutrition. J Pediatr 1971; 78: 180–181.
Teitelbaum DH, Tracy T . Parenteral nutrition-associated cholestasis. Semin Pediatr Surg 2001; 10: 72–80.
Clark RH, Chace DH, Spitzer AR . The effects of two different doses of amino acid administration on growth and blood amino acids in premature neonates admitted to the NICU: a randomized controlled trial. Pediatrics 2007 (in press).
Spencer AU, Yu S, Tracy TF, Aouthmany MM, Llanos A, Brown MB et al. Parenteral nutrition-associated cholestasis in neonates: multivariate analysis of the potential protective effect of taurine. JPEN J Parenter Enteral Nutr 2005; 29: 337–343.
Zambrano E, El Hennawy M, Ehrenkranz RA, Zelterman D, Reyes-Mugica M . Total parenteral nutrition induced liver pathology: an autopsy series of 24 newborn cases. Pediatr Dev Pathol 2004; 7: 425–432.
Suchy FJ, Balistreri WF, Heubi JE, Searcy JE, Levin RS . Physiologic cholestasis: elevation of the primary serum bile acid concentrations in normal infants. Gastroenterology 1981; 80: 1037–1041.
Colomb V, Jobert-Giraud A, Lacaille F, Goulet O, Fournet JC, Ricour C . Role of lipid emulsions in cholestasis associated with long-term parenteral nutrition in children. JPEN J Parenter Enteral Nutr 2000; 24: 345–350.
Krawinkel MB . Parenteral nutrition-associated cholestasis—what do we know, what can we do? Eur J Pediatr Surg 2004; 14: 230–234.
Bougle D, Bureau F, Deschrevel G, Hecquard C, Neuville D, Drosdowsky M et al. Chromium and parenteral nutrition in children. J Pediatr Gastroenterol Nutr 1993; 17: 72–74.
Bove KE, Kosmetatos N, Wedig KE, Frank DJ, Whitlatch S, Saldivar V et al. Vasculopathic hepatotoxicity associated with E-Ferol syndrome in low-birth-weight infants. JAMA 1985; 254: 2422–2430.
Erikson KM, Thompson K, Aschner J, Aschner M . Manganese neurotoxicity: a focus on the neonate. Pharmacol Ther 2007; 113: 369–377.
Forbes A, Jawhari A . Manganese toxicity and parenteral nutrition. Lancet 1996; 347: 1774.
Klein GL . Aluminum: new recognition of an old problem. Curr Opin Pharmacol 2005; 5: 637–640.
Albers MJ, Gast-Bakker DA, van Dam NA, Madern GC, Tibboel D . Male sex predisposes the newborn surgical patient to parenteral nutrition-associated cholestasis and to sepsis. Arch Surg 2002; 137: 789–793.
Herzog D, Chessex P, Martin S, Alvarez F . Transient cholestasis in newborn infants with perinatal asphyxia. Can J Gastroenterol 2003; 17: 179–182.
Chessex P, Lavoie JC, Rouleau T, Brochu P, St Louis P, Levy E et al. Photooxidation of parenteral multivitamins induces hepatic steatosis in a neonatal guinea pig model of intravenous nutrition. Pediatr Res 2002; 52: 958–963.
Chessex P, Friel J, Harrison A, Rouleau T, Lavoie JC . The mode of delivery of parenteral multivitamins influences nutrient handling in an animal model of total parenteral nutrition. Clin Nutr 2005; 24: 281–287.
Silvers KM, Darlow BA, Winterbourn CC . Lipid peroxide and hydrogen peroxide formation in parenteral nutrition solutions containing multivitamins. JPEN J Parenter Enteral Nutr 2001; 25: 14–17.
Clayton PT, Whitfield P, Iyer K . The role of phytosterols in the pathogenesis of liver complications of pediatric parenteral nutrition. Nutrition 1998; 14: 158–164.
Bindl L, Lutjohann D, Buderus S, Lentze MJ, Bergmann K . High plasma levels of phytosterols in patients on parenteral nutrition: a marker of liver dysfunction. J Pediatr Gastroenterol Nutr 2000; 31: 313–316.
Thureen PJ, Hay Jr WW . Early aggressive nutrition in preterm infants. Semin Neonatol 2001; 6: 403–415.
Thureen PJ, Melara D, Fennessey PV, Hay Jr WW . Effect of low versus high intravenous amino acid intake on very low birth weight infants in the early neonatal period. Pediatr Res 2003; 53: 24–32.
Kotsopoulos K, Benadiba-Torch A, Cuddy A, Shah PS . Safety and efficacy of early amino acids in preterm <28 weeks gestation: prospective observational comparison. J Perinatol 2006; 26: 749–754.
Poindexter BB, Langer JC, Dusick AM, Ehrenkranz RA . Early provision of parenteral amino acids in extremely low birth weight infants: relation to growth and neurodevelopmental outcome. J Pediatr 2006; 148: 300–305.
Clark RH, Wagner CL, Merritt RJ, Bloom BT, Neu J, Young TE et al. Nutrition in the neonatal intensive care unit: how do we reduce the incidence of extrauterine growth restriction? J Perinatol 2003; 23: 337–344.
Suita S, Yamanouchi T, Masumoto K, Ogita K, Nakamura M, Taguchi S . Changing profile of parenteral nutrition in pediatric surgery: a 30-year experience at one institute. Surgery 2002; 131: S275–S282.
Wright K, Ernst KD, Gaylord MS, Dawson JP, Burnette TM . Increased incidence of parenteral nutrition-associated cholestasis with aminosyn PF compared to trophamine. J Perinatol 2003; 23: 444–450.
Adamkin DH . Total parenteral nutrition-associated cholestasis: prematurity or amino acids? J Perinatol 2003; 23: 437–438.
Kadrofske MM, Parimi PS, Gruca LL, Kalhan SC . Effect of intravenous amino acids on glutamine and protein kinetics in low-birth-weight preterm infants during the immediate neonatal period. Am J Physiol Endocrinol Metab 2006; 290: E622–E630.
de Urbina JJ, Jorquera F, Culebras JM, Villares C, Gonzalez-Gallego J, Tunon MJ . Effects of parenteral nutrition supplemented with alanyl-glutamine on nutrition status in rats. JPEN J Parenter Enteral Nutr 2005; 29: 262–265.
Parimi PS, Kadrofske MM, Gruca LL, Hanson RW, Kalhan SC . Amino acids, glutamine, and protein metabolism in very low birth weight infants. Pediatr Res 2005; 58: 1259–1264.
Poindexter BB, Ehrenkranz RA, Stoll BJ, Wright LL, Poole WK, Oh W et al. Parenteral glutamine supplementation does not reduce the risk of mortality or late-onset sepsis in extremely low birth weight infants. Pediatrics 2004; 113: 1209–1215.
Tyson JE, Kennedy KA . Trophic feedings for parenterally fed infants. Cochrane Database Syst Rev 2005; (3): CD000504.
Kennedy KA, Tyson JE, Chamnanvanikij S . Early versus delayed initiation of progressive enteral feedings for parenterally fed low birth weight or preterm infants. Cochrane Database Syst Rev 2000; (2): CD001970.
Unachak K, Dejkhamron P . Primary congenital hypothyroidism: clinical characteristics and etiological study. J Med Assoc Thai 2004; 87: 612–617.
Author information
Authors and Affiliations
Consortia
Corresponding author
Additional information
Pediatrix Amino-Acid Study Group
Principal Investigators: Debra Bender, ARNP—Swedish Medical Center (WA); Barbara Carr, MD—St Luke's Hospital (MO); Carlos Flores, MD—Tucson Medical Center (AZ); Jose Gierbolini, MD—Stormont-Vail Regional Health Center (KS); David W Green, MD—Presbyterian Hospital of Dallas (TX); Joseph Harlan, MD—McLeod Regional Medical Center (SC); Michael Kamitsuka, MD—Swedish Medical Center (WA); Sridhar Kaushik, MD—Pinnacle Health—Harrisburg Hospital (PA); Amy S Kelleher, BS—Pediatrix Medical Group (FL); Jose Perez, MD—Arnold Palmer Medical Center (FL); Meera Sankar, MD—Good Samaritan Medical Center (CA); Bindya Singh, MD—Good Samaritan Medical Center (CA); Margaret Steinbach, NNP—Pediatrix Medical Group (FL); Robert White—Memorial Hospital of South Bend (IN); Henry H Wooldridge, MD—East Tennessee Children's Hospital (TN).
Study Registration Number: ClinicalTrials.gov Identifier: NCT00120926; http://clinicaltrials.gov/ct/show/NCT00120926?order=1.
Contributors: East Tennessee Children's Hospital (TN)—P Kathine Fulton, RNC, NNP; Good Samaritan Medical Center (CA)—Chrissy Weng RN; McLeod Regional Medical Center (SC)—Evelyn Fulmore, Pharm D; Memorial Hospital of South Bend (IN)—Delores Troyer NNP; Pinnacle Health—Harrisburg Hospital (PA)—Penny Barcavage NNP; Presbyterian Hospital of Dallas (TX)—Renuka K Reddy, MD; Stormont-Vail Regional Health Center (KS)—Renee Hunt, RNC, NNP; Tucson Medical Center (AZ)—Colleen Bakewell.
Conflict of interest: All of the authors are employees of Pediatrix Medical Group that owns Pediatrix Screening, a company that offers newborn screening for inborn errors of metabolism and hearing loss.
Rights and permissions
About this article
Cite this article
Steinbach, M., Clark, R., Kelleher, A. et al. Demographic and nutritional factors associated with prolonged cholestatic jaundice in the premature infant. J Perinatol 28, 129–135 (2008). https://doi.org/10.1038/sj.jp.7211889
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211889
Keywords
This article is cited by
-
A Review of Short Bowel Syndrome Including Current and Emerging Management Strategies
Current Treatment Options in Pediatrics (2021)