Abstract
Objective:
To identify factors associated with the development of neonatal injury in the setting of shoulder dystocia.
Study design:
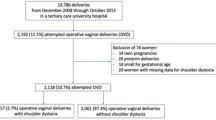
Medical record ICD-9 codes and a computerized perinatal database were reviewed to identify cases of shoulder dystocia from January 1996 to January 2001 in a tertiary care center. For confirmation of the diagnosis and collection of data, both maternal and neonatal charts were then reviewed and neonatal injuries categorized as either neurological (brachial plexus injury) or skeletal (clavicular fracture, humeral fracture). Shoulder dystocia cases were divided into groups based on the presence of neonatal injury at delivery or at discharge (with or without Erb's palsy). The group with neonatal injury was compared for demographic and obstetrical factors to the group without injury (control). χ2 test, Mann–Whitney test and logistic regression were used as appropriate.
Results:
During this 5-year period, there were 25 995 deliveries and 206 (0.8%) confirmed cases of shoulder dystocia. Of these cases, 36 (17.5%) had neonatal injury diagnosed at delivery and 25 (12%) remained with significant residual injury at discharge. Of these there were 19 cases of Erb's palsy and six cases of clavicular fracture. No association was found between neonatal injury and maternal age, ethnicity, diabetes, operative vaginal delivery or number of obstetrical maneuvers. However, maternal body mass index >30 kg/m2, a second stage of labor >20 min and a birth weight >4500 g were all associated with an increased risk of neonatal injury at delivery and at discharge, including Erb's palsy. After logistic regression analysis, only a second stage of delivery >20 min remained significantly associated with neonatal injury at discharge.
Conclusion:
In our population, maternal obesity was associated with an increased risk of neonatal injury after shoulder dystocia. In addition, a short second stage of labor (<20 min) was associated with a lower rate of neonatal injury.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
ACOG practice bulletin clinical management guidelines for obstetrician-gynecologists. Obstet Gynecol 2002; 100(40): 1045–1050.
Gherman RB, Goodwin TM, Ouzounian JG, Miller DA, Paul RH . Brachial plexus palsy associated with cesarean section: an in utero injury? Am J Obstet Gynecol 1997; 177: 1462–1464.
Baskett TF, Allen AC . Perinatal implications of shoulder dystocia. Obstet Gynecol 1995; 86: 14–17.
Hope P, Breslin S, Lamont L, Lucas A, Martin D, Moore I et al. Fatal shoulder dystocia: a review of 56 cases reported to the confidential enquiry into stillbirths and deaths in infancy. Br J Obstet Gynecol 1996; 276: 1480–1486.
Ouzounian JG, Korst LM, Phelan JP . Permanent Erb's palsy: a lack of a relationship with obstetrical risk factors. Am J Perinatol 1998; 15: 221–223.
Poggi SH, Stallings SP, Ghidini A, Spong CY, Deering SH, Allen RH . Intrapartum risk factors for permanent brachial plexus injury. Am J Obstet Gynecol 2003; 189: 725–729.
Ecker JL, Greenberg JA, Norwitz ER, Nadel AS, Repke JT . Birth weight as a predictor of brachial plexus injury. Obstet Gynecol 1997; 89: 643–647.
Christoffersson M, Kannisto P, Rydhstroem H, Stale H, Walles B . Shoulder dystocia and brachial plexus injury: a case-control study. Acta Obstet Gynecol Scand 2003; 82: 147–151.
Mehta SH, Bujold E, Blackwell SC, Sorokin Y, Sokol RJ . Is abnormal labor associated with shoulder dystocia in nulliparous women? Am J Obstet Gynecol 2004; 190: 1604–1607.
Gonik B, Walker A, Grimm M . Mathematic modeline of forces associated with shoulder dystocia: a comparison of endogenous and exogenous sources. Am J Obstet Gynecol 2000; 182: 689–691.
Jennett RJ, Tarby TJ, Kreinick CJ . Brachial plexus injury: an old problem revisited. Am J Obstet Gynecol 1992; 166: 1673–1677.
Jensen DM, Damm P, Sorensen B, Molsted-Pedersen L, Westergaard JG, Ovesen P et al. Pregnancy outcome and prepregnancy body mass index in 2459 glucose-tolerant Danish women. Am J Obstet Gynecol 2003; 189: 239–244.
Robinson H, Tkatch S, Mayes DC, Bott N, Okun N . Is maternal obesity a predictor of shoulder dystocia? Obstet Gynecol 2003; 101: 24–27.
Lewis DF, Edwards MS, Asrat T, Adair CD, Brooks G, London S . Can shoulder dystocia be predicted? J Reprod Med 1998; 43: 654–658.
Cedergren MI . Maternal morbid obesity and the risk of adverse outcome. Obstet Gynecol 2004; 103: 219–224.
Walle T, Hartikainen-Sorri AL . Obstetric shoulder injury. Associated risk factors, prediction and prognosis. Acta Obstet Gynecol Scand 1993; 72: 450–454.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mehta, S., Blackwell, S., Bujold, E. et al. What factors are associated with neonatal injury following shoulder dystocia?. J Perinatol 26, 85–88 (2006). https://doi.org/10.1038/sj.jp.7211441
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211441
Keywords
This article is cited by
-
Epidemiologic aspects of shoulder dystocia-related neurological birth injuries
Archives of Gynecology and Obstetrics (2015)
-
Severe shoulder dystocia leading to neonatal injury: a case control study
Archives of Gynecology and Obstetrics (2009)
-
Maternal Obesity: A Problem for Both Mother and Child
Obesity (2008)