Abstract
BACKGROUND:
B-type natriuretic peptide (BNP) is a hormone secreted by the ventricles under hemodynamic stress and congestive failure.
OBJECTIVE:
The objective of the present study was to evaluate whether BNP can be used as a valid screening test for the presence of a hemodynamically significant patent ductus arteriosus (hsPDA) in the preterm neonate.
MATERIALS AND METHODS:
This was a prospective blinded study involving preterm neonates with birth weights ≤1500 g and gestational age ≤34 weeks. Each enrolled neonate underwent the initial echocardiogram for a clinical suspicion of patent ductus arteriosus (PDA) and BNP assay within 3 hours of each other. Those neonates who did not have a PDA or who were not treated underwent a repeat echo and BNP measurement 48 to 72 hours after the first echo. In patients who received treatment for a PDA, an echo and BNP were repeated 48 to 72 hours after completion of treatment.
RESULTS:
A total of 29 newborns with a median birth weight of 870 g (560 to 1325 g) and a median gestation of 26 weeks (24 to 31 weeks) were enrolled at a median age of 7 days (2 to 28 days). BNP levels were significantly higher in neonates with hsPDA (n=14) compared to those without (n=15) (508.5±618.2 vs 59.5±69.9 pg/ml, p<0.005). At a cutoff value of 70 pg/ml, BNP had a sensitivity of 92.9%, specificity of 73.3%, positive likelihood ratio of 3.5 and negative likelihood ratio of 0.09 for detection of hsPDA. BNP levels dropped significantly after medical or surgical closure of hsPDA (n=12), (404.9±159.2 to 25.1±4.1 pg/ml, p=0.03).
CONCLUSIONS:
Elevation of plasma BNP accurately detects the presence of hsPDA in premature infants. Successful closure is reflected by a corresponding decrease in BNP. At a cutoff of 70 pg/ml, BNP is a useful screening tool for diagnosis and for monitoring efficacy of treatment of hsPDA.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Reller MD, Lorenz JM, Kotagal UR, Meyer RA, Kaplan S . Hemodynamically significant PDA: an echocardiographic and clinical assessment of incidence, natural history, and outcome in very low birth weight infants maintained in negative fluid balance. Pediatr Cardiol 1985;6(1):17–23.
Shimada S, Kasai T, Hoshi A, Murata A, Chida S . Cardiocirculatory effects of patent ductus arteriosus in extremely low-birth-weight infants with respiratory distress syndrome. Pediatr Int 2003;45(3):255–262.
Evans N, Kluckow M . Early ductal shunting and intraventricular haemorrhage in ventilated preterm infants. Arch Dis Child Fetal Neonatal Ed 1996;75(3):F183–F186.
Dudell GG, Gersony WM . Patent ductus arteriosus in neonates with severe respiratory disease. J Pediatr 1984;104(6):915–920.
Fowlie PW, Davis PG . Prophylactic indomethacin for preterm infants: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed 2003;88(6):F464–F466.
Schmidt B, Davis P, Moddemann D, Ohlsson A, Roberts RS, Saigal S, et al. Long-term effects of indomethacin prophylaxis in extremely-low-birth-weight infants. N Engl J Med 2001;344(26):1966–1972.
Mellander M, Larsson LE, Ekstrom-Jodal B, Sabel KG . Prediction of symptomatic patent ductus arteriosus in preterm infants using Doppler and M-mode echocardiography. Acta Paediatr Scand 1987;76(4):553–559.
Skelton R, Evans N, Smythe J . A blinded comparison of clinical and echocardiographic evaluation of the preterm infant for patent ductus arteriosus. J Paediatr Child Health 1994;30(5):406–411.
Davis P, Turner-Gomes S, Cunningham K, Way C, Roberts R, Schmidt B . Precision and accuracy of clinical and radiological signs in premature infants at risk of patent ductus arteriosus. Arch Pediatr Adolesc Med 1995;149(10):1136–1141.
Archer LN, Glass EJ, Godman MJ . The silent ductus arteriosus in idiopathic respiratory distress syndrome. Acta Paediatr Scand 1984;73(5):652–656.
Maeda K, Tsutamoto T, Wada A, Hisanaga T, Kinoshita M . Plasma brain natriuretic peptide as a biochemical marker of high left ventricular end-diastolic pressure in patients with symptomatic left ventricular dysfunction. Am Heart J 1998;135(5 Part 1):825–832.
Maisel AS . B-type natriuretic peptide (BNP) levels: diagnostic and therapeutic potential. Rev Cardiovasc Med 2001;2(Suppl 2):S13–S18.
Richards AM, Nicholls MG, Espiner EA, Lainchbury JG, Troughton RW, Elliott J, et al. B-type natriuretic peptides and ejection fraction for prognosis after myocardial infarction. Circulation 2003;107(22):2786–2792.
Maisel AS, Krishnaswamy P, Nowak RM, McCord J, Hollander JE, Duc P, et al. Rapid measurement of B-type natriuretic peptide in the emergency diagnosis of heart failure. N Engl J Med 2002;347(3):161–167.
Morrison LK, Harrison A, Krishnaswamy P, Kazanegra R, Clopton P, Maisel A . Utility of a rapid B-natriuretic peptide assay in differentiating congestive heart failure from lung disease in patients presenting with dyspnea. J Am Coll Cardiol 2002;39(2):202–209.
Kunii Y, Kamada M, Ohtsuki S, Araki T, Kataoka K, Kageyama M, et al. Plasma brain natriuretic peptide and the evaluation of volume overload in infants and children with congenital heart disease. Acta Med Okayama 2003;57(4):191–197.
Puddy VF, Amirmansour C, Williams AF, Singer DR . Plasma brain natriuretic peptide as a predictor of haemodynamically significant patent ductus arteriosus in preterm infants. Clin Sci (Lond) 2002;103(1):75–77.
Holmstrom H, Hall C, Thaulow E . Plasma levels of natriuretic peptides and hemodynamic assessment of patent ductus arteriosus in preterm infants. Acta Paediatr 2001;90(2):184–191.
Nagaya N, Nishikimi T, Okano Y, Uematsu M, Satoh T, Kyotani S, et al. Plasma brain natriuretic peptide levels increase in proportion to the extent of right ventricular dysfunction in pulmonary hypertension. J Am Coll Cardiol 1998;31(1):202–208.
McCullough PA, Duc P, Omland T, McCord J, Nowak RM, Hollander JE, et al. B-type natriuretic peptide and renal function in the diagnosis of heart failure: an analysis from the Breathing Not Properly Multinational Study. Am J Kidney Dis 2003;41(3):571–579.
Skinner J . Diagnosis of patent ductus arteriosus. Semin Neonatol 2001;6(1):49–61.
Fleiss JL . Constant chi-square boundaries. In: Fleiss JL, editor. Statistical Methods for Rates and Proportions. 2nd ed. New York: John Wiley & sons; 1981.
Muta H, Ishii M, Maeno Y, Akagi T, Kato H . Quantitative evaluation of the changes in plasma concentrations of cardiac natriuretic peptide before and after transcatheter closure of atrial septal defect. Acta Paediatr 2002;91(6):649–652.
Fagan TJ . Letter: Nomogram for Bayes theorem. N Engl J Med 1975;293(5):257.
Levin ER, Gardner DG, Samson WK . Natriuretic peptides. N Engl J Med 1998;339(5):321–328.
Tsuchida K, Tanabe K . Influence of paroxysmal atrial fibrillation attack on brain natriuretic peptide secretion. J Cardiol 2004;44(1):1–11.
Maron BJ, Tholakanahalli VN, Zenovich AG, Casey SA, Duprez D, Aeppli DM, et al. Usefulness of B-type natriuretic peptide assay in the assessment of symptomatic state in hypertrophic cardiomyopathy. Circulation 2004;109(8):984–989.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Sanjeev, S., Pettersen, M., Lua, J. et al. Role of Plasma B-Type Natriuretic Peptide in Screening for Hemodynamically Significant Patent Ductus Arteriosus in Preterm Neonates. J Perinatol 25, 709–713 (2005). https://doi.org/10.1038/sj.jp.7211383
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211383
This article is cited by
-
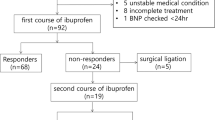
Plasma B-type natriuretic peptide cannot predict treatment response to ibuprofen in preterm infants with patent ductus arteriosus
Scientific Reports (2020)
-
Early prediction of spontaneous Patent Ductus Arteriosus (PDA) closure and PDA-associated outcomes: a prospective cohort investigation
BMC Pediatrics (2019)
-
Base excess and hematocrit predict response to indomethacin in very low birth weight infants with patent ductus arteriosus
Italian Journal of Pediatrics (2019)
-
Early NT-proBNP levels as a screening tool for the detection of hemodynamically significant patent ductus arteriosus during the first week of life in very low birth weight infants
Journal of Perinatology (2018)
-
The relationship between BNP, NTproBNP and echocardiographic measurements of systemic blood flow in very preterm infants
Journal of Perinatology (2014)