Abstract
OBJECTIVE: To evaluate the effect of radiant warmers on skin barrier function in preterm infants.
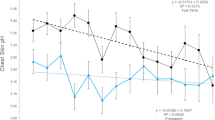
METHODOLOGY: Transepidermal water loss (TEWL) and stratum corneum hydration were measured in 30 preterm infants (birth weight 825 to 2220 g) in seven body areas: forehead, upper back, cubital fossa, palms, soles, abdomen, and inguinal region. Measurements were performed under radiant warmer and incubator conditions. Each patient served as his/her control.
RESULTS: TEWL was significantly higher in the radiant warmer compared to the incubator condition in only two areas: forehead and back. The overall mean difference in percentage TEWL between the conditions was 15%. Stratum corneum hydration was not affected by the radiant warmer.
CONCLUSIONS: The use of radiant warmers does not significantly decrease barrier function in the preterm infant.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Nachman RL, Esterly NB . Increased skin permeability in preterm infants. J Pediatr 1971;79:628–632.
Harpin VA, Rutter N . Barrier properties of the newborn infant's skin. J Pediatr 1983;102:419–425.
Fanaroff AA, Wald M, Gruber HS, Klaus MH . Insensible water loss in low birth weight infants. Pediatrics 1972;49:236–245.
Wu PY, Hodgman JE . Insensible water loss in preterm infants: changes with postnatal development and non-ionizing radiant energy. Pediatrics 1974;54:704.
Williams PR, Oh W . Effects of radiant warmer on insensible water loss in newborn infants. Am J Dis Child 1974;128:511–514.
Visscher MO, Srinath M, Munson K, Bare D, Hoath SB . Early adaptation of human skin following birth: a biophysical assessment. Skin Res Technol 1999;5:312–320.
Hammarlund K, Sedin G . Transepidermal water loss in newborn infants. Acta Paediatr Scand 1979;68:795–801.
Kalia YN, Nonato LB, Lund CH, Guy RH . Development of skin barrier function in premature infants. J Invest Dermatol 1998;111:320–326.
Hammarlund K, Nilsson GE, Oberg PA, Sedin G . Transepidermal water loss in newborn infants. Relation to ambient humidity and site of measurement and estimation of total transepidermal water loss. Acta Paediatr Scand 1979;68:371–376.
Avery BG, Fletcher AM, MacDonald GM . Neonatology. J.B. Lippincott Company: Philadelphia, 4th ed. 1994, 358–360.
Yosipovitch G, Maayan-Metzger A, Merlob P, Sirota L . Skin barrier properties in different body areas in neonates. Pediatrics 2000;106:105–108.
Visscher MO, Chatterjee R, Ebel J, et al. Biomedical assesemnt and instrumental evaluation of healthy infants skin. Pediatr Dermatol 2002;19:473–481.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Maayan-Metzger, A., Yosipovitch, G., Hadad, E. et al. Effect of Radiant Warmer on Transepidermal Water Loss (TEWL) and Skin Hydration in Preterm Infants. J Perinatol 24, 372–375 (2004). https://doi.org/10.1038/sj.jp.7211107
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7211107