Abstract
Routine neonatal circumcision can be a painful procedure. Although analgesia for circumcision has been studied extensively, there are few studies comparing which surgical technique may be associated with the least pain and discomfort when carried out by pediatric trainees.
OBJECTIVE: We studied two commonly used techniques for circumcision to determine which was associated with less pain and discomfort.
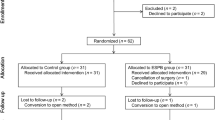
STUDY DESIGN: In a randomized, prospective, but not blinded study, newborns were circumcised either by Mogen clamp or by PlastiBell. All received dorsal nerve blocks with lidocaine. Fifty-nine well, term, newborn infants at San Francisco General Hospital were studied from 1997 to 1998. Circumcisions were carried out mostly by interns and residents in family practice and pediatrics. Pain was assessed by measuring duration of the procedure and by a simple behavioral score done sequentially.
RESULTS: Dorsal nerve blocks were judged to be fully effective in over 70% of cases. Neither Mogen nor PlastiBell was associated with greater pain per 3-minute time period, but the PlastiBell technique on average took nearly twice as long as the Mogen procedure (20 vs 12 minutes). We judged that 60% of the infants had pain or discomfort associated with the procedure that was excessive. Residents and interns universally preferred the Mogen technique over the PlastiBell because of the former's simplicity.
CONCLUSION: During the procedure, Mogen circumcision is associated with less pain and discomfort, takes less time, and is preferred by trainees when compared with the PlastiBell.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Wiswell TE . Circumcision circumspection N Engl J Med 1997 3336: 1244–5
Gollaher D . Circumcision: A History of the World's Most Controversial Surgery New York: Basic Books 2000
Wellington N, Rieder MJ . Attitudes and practices regarding analgesia for newborn circumcisions Pediatrics 1993 92: 541–3
Lovell J . Maternal attitudes towards circumcision J Fam Pract 1979 9: 811–3
Patel D . Factors affecting the practice of circumcision Am J Dis Child 1982 136: 634–6
Grossman E, Posner N . Surgical circumcision of neonates: a history of its development Obstet Gynecol 1981 58: 241–6
Circumcision. Circumcision policy statement Pediatrics 1999 103: 686–93
Grimes D . Routine circumcision of the newborn infant: a reappraisal Am J Obstet Gynecol 1978 130: 125–9
Dixon S, Snyder J, Holve R . Behavioral effects of circumcision with and without anesthesia J Dev Behav Pediatr 1984 5: 246–50
Marshall R, Stratton W, Moore J . Circumcision I: effects on newborn behavior Infant Behav Dev 1980 3: 1–14
Anand K, Hickey P . Pain and its effects in the human neonate and fetus N Engl J Med 1987 317: 1321–9
Taddio A, Katz J, Ilersich A, Koren G . Effect of neonatal circumcision on pain response during subsequent routine vaccination Lancet 1997 349: 599–603
Kurtis PS, DeSilva HN, Bernstein BA, Malakh L, Schechter NL . A comparison of the Mogen and Gomco clamps in combination with dorsal penile nerve block in minimizing the pain of neonatal circumcision Pediatrics 1999 103: E23
Benini F, Johnston CC, Faucher D, Aranda JV . Topical anesthesia during circumcision in newborn infants JAMA 1993 270: 850–3
Kirya C, Werthmann M . Neonatal circumcision and penile dorsal nerve block — a painless procedure J Pediatr 1978 92: 998–1000
Holliday MA, Pinchert TL, Kiernan SC, Kunos I, Angelus P, Keszler M . Dorsal penile nerve block vs topical placebo for circumcision in low-birth-weight neonates Arch Pediatr Adolesc Med 1999 153: May 476–80
Fontaine P, Toffler WL . Dorsal penile nerve block for newborn circumcision Am Fam Physician 1991 43: 1327–33
Abu-Saad H, Bours H-G, Stevens B, Hamers J . Assessment of pain in the neonate Semin Perinatol 1998 22: 402–16
Stang H, Snellman L, Condon L et al. Beyond dorsal penile nerve block: a more humane circumcision Pediatrics 1997 100: E3
Barr R . Reflections on measuring pain in infants: dissociation in responsive systems and “honest signalling” Neonat Intensive Care 1998 12: 19–24
Schoen EJ, Wiswell TE, Moses S . New policy on circumcision — cause for concern Pediatrics 2000 105: 620–3
Multiple authors. Supplement on circumcision Br J Urol 1999 83: 1–109
NOHARMM. Available at http://www.noharmm.org1999
Laumann EO, Masi CM, Zuckerman EW . Circumcision in the United States: prevalence, prophylactic effects, and sexual practices JAMA 1997 277: No. 13 April 1052–7
Hammond T . A preliminary poll of men circumcised in infancy or childhood Br J Urol 1999 83: Suppl 1 85–92
O'Hara K, O'Hara J . The effect of male circumcision on the sexual enjoyment of the female partner Br J Urol 1999 83: (Suppl 1) 79–84
Kaplan G . Complications of circumcision Urol Clin North Am 1983 10: 543–9
Williams N, Kapila L . Complications of circumcision Br J Surg 1993 80: Oct 1231–6
Oskan S, Gurpinar T . A serious circumcision complication: penile shaft amputation. A new reattachment technique with a successful outcome J Urol 1997 158: 1946–7
Gluckman G, Stoller M, Jacobs M, Kogan B . Newborn penile glans amputation during circumcision and successful reattachment J Urol 1995 153: 778–9
Bliss D, Healey P, Waldhausen J . Necrotizing fasciitis after PlastiBell circumcision J Pediatr 1996 131: 459–62
Acknowledgements
The interest, support, and participation of the University of California — San Francisco pediatric house staff, medical students, and the San Francisco General Hospital Infant Care Center nursing staff was critical for the conduct of this study.
Author information
Authors and Affiliations
Additional information
Financial support for this study was provided by the Department of Pediatrics, University of California — San Francisco.
Rights and permissions
About this article
Cite this article
Taeusch, H., Martinez, A., Partridge, J. et al. Pain During Mogen or PlastiBell Circumcision. J Perinatol 22, 214–218 (2002). https://doi.org/10.1038/sj.jp.7210653
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.jp.7210653
This article is cited by
-
Neonatal Infant Pain Scale in assessing pain and pain relief for newborn male circumcision
International Journal of Impotence Research (2023)
-
Management of pain in newborn circumcision: a systematic review
European Journal of Pediatrics (2021)
-
Analgesia for infants’ circumcision
Italian Journal of Pediatrics (2013)