Abstract
Purpose
To determine the trends and outcomes for treating primary rhegmatogenous retinal detachment (RRD) in a nationwide population-based study in Taiwan.
Methods
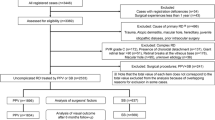
We collected admission data during the period of 1997–2005, from the Taiwan National Health Insurance Research Database, a source that covers over 96% of Taiwan's 23 million citizens. Totally 28 911 patients with a first-time admission diagnosis of RRD (ICD-9-CM codes 361 to 361.07) and undergoing surgical treatment (scleral buckling (SB), pars plana vitrectomy (PPV), or their combination) were identified. The utilized operation type, 180-day readmission rate for recurrent retinal detachment, length of hospital stay, and admission charge were obtained. Contingency table/χ2 test and t-test were employed for the statistical analysis.
Results
Primary PPV (with or without SB) was a primary procedure in 47.3% of cases in 1997. This rate rose significantly to 61.2% in 2005. A significant decrease in the total 180-day readmission rate occurred from 18.95% in 1997 to 13.81% in 2005. These rates also significantly decreased for each surgical modality (from 16.30 to 11.38% for SB, from 21.29 to 14.69% for PPV, and from 22.99 to 16.55% for PPV+SB). The length of hospital stay decreased for each surgical modality between 1997 and 2005.
Conclusions
There was a significant trend towards more frequently employing primary PPV (with or without SB) for the management of primary RRD. In addition, significant improvements in the primary success rates were shown for each surgical modality group and for total samples between 1997 and 2005.
Similar content being viewed by others
Introduction
The surgical cure of rhegmatogenous retinal detachment (RRD) was rare prior to the demonstration by Gonin1 of the importance of localizing and sealing retinal breaks. With the introduction of scleral buckling (SB),2 intraocular gas injection,3 and pars plana vitrectomy (PPV),4 the history of RRD repair greatly changed. Even more difficult cases of RRD can now be operated on with these advances in techniques and technology. In many vitreoretinal surgical centres, the use of SB constitutes the mainstay of treatment for RRD, either alone for routine uncomplicated cases (a single break and/or limited retinal detachment) or combined with vitrectomy in patients with more advanced forms of the disease (vitreous haemorrhage/opacity, proliferative vitreoretinopathy, or a posteriorly located break).5, 6, 7, 8, 9 Recently, several studies reported a trend towards primary PPV as the method of first choice for primary RRD treatment.10, 11, 12, 13, 14, 15, 16 Some of those studies supported this trend with statistical data.10, 11, 12, 13, 16 In those studies, some observed a statistically significant increase in the primary success rate concomitant with a trend towards a greater number of primary PPV,12, 13 while others did not.10, 11, 16 Those studies were either hospital or vitreoretinal surgical centre based. In those studies, there was a heavy reliance on data collected from a single hospital or a few selected hospitals, with coverage of only subgroups of populations.
In this study utilizing a nationwide population-based administrative database (Taiwan National Health Insurance Research Database (NHIRD), a source that covers over 96% of Taiwan's 23 million citizens), we determined the trends (PPV vs SB) and outcomes in the treatment for primary RRD over the years of 1997–2005.
Methods
Hospitalization data
This study used data from the NHIRD covering the years 1997–2005, published by the Taiwan National Health Research Institute.17 The NHIRD includes registries of contracted medical facilities, board-certified physicians, patients with catastrophic illnesses, claim summaries for both in-patient and ambulatory care, details of in-patient and ambulatory care orders, and all expenditures for prescriptions dispensed through contracted pharmacies.
Since the study used secondary data without patient, institution, or physician identifiers, the Ethics Committee of the authors’ institution granted a waiver of informed consent for the study.
Study sample
We selected patients with a principal diagnosis of retinal detachment and defects (ICD-9-CM code 361 to 361.07) admitted to hospitals between 1 January 1997 and 31 December 2005. Patients with a concomitant diagnosis of proliferative diabetic retinopathy (ICD-9-CM code 362.02) were excluded. Since a patient may have had more than one operation for the treatment of retinal detachment, we only selected first-time admissions as the index hospitalization. Given universal health-care coverage, negligible financial barriers to access (patients have to pay only 10% of the medical costs for the admission from their own pocket, which was an average of US$149 for each admission for RD treatment. Note that the per capita gross national product for Taiwan was US$13 34818 in 2001), and the grave visual outcomes if RRD is left untreated, we believe most of the existing patients with RRD were included.
Statistical analysis
The main outcome measures were the proportion of the surgical modality employed, 180-day readmission rate (with a diagnosis of RRD or tractional RD, ICD codes 361 to 361.07, 361.8, 361.81, 361.89, and 361.9, and undergoing surgery of SB or PPV), length of hospital stay (LOS), and hospitalization costs. All statistical analyses were performed using the SAS statistical package (SAS System for Windows, version 8.2). Descriptive analyses, including frequencies, proportions, means, and standard deviations, were performed on all of the identified variables. χ2 test was performed to examine the statistical significance of the trends and outcomes of the treatment. The LOS and hospitalization costs were compared with t-test. In this study, any P-values of <0.05 were considered statistically significant.
Results
Our study sample was comprised of 28 911 cases of patients hospitalized first time for the treatment of RRD in Taiwan in 1997–2005, inclusive. Among these sampled patients, 11 423 (39.5%) underwent SB, 10 491 (36.3%) PPV, and the remaining 6997 (24.2%) both PPV and SB at the index hospitalization. There was a consistent increase in the annual admissions for treatment of primary RRD during the 9-year study period, with total annual admissions for the treatment of retinal detachments of 2501 in 1997, 2731 in 1998, 2855 in 1999, 2919 in 2000, 3310 in 2001, 3456 in 2002, 3467 in 2003, 3749 in 2004, and 3923 in 2005 (Table 1).
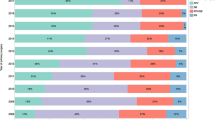
Table 1 also summarizes the surgical approaches for primary RRD repair for the period from 1997 to 2005 in Taiwan. In 1997, 52.7% of the patients underwent primary SB (without PPV), 29.9% underwent primary PPV (without SB), and 17.4% were treated by combined PPV and SB. At the end of the study period (in 2005), the proportion of primary RRD treated by SB had significantly decreased to 38.8% (P<0.001, χ2 test). Concurrently, there was a rise in the proportion of patients treated by primary PPV alone (to 39.8%) and combined PPV plus SB (to 21.4%) (both P<0.001, χ2 test). The trends of the percentages of the surgical modalities utilized during the study period are plotted in Figure 1.
Table 2 shows the rate of readmission within 180 days with a diagnosis of RD (RRD or tractional RD) and treatment with either SB, PPV, or both procedures combined during the readmission period. This defined 180-day readmission rate served as an indicator for the anatomical failure rate of the primary surgery, ie, 1–180-day readmission rate could serve as an indicator of the anatomical success rate of the primary surgery. The 180-day readmission rate for primary SB was 16.30% in 1997. This rate progressively decreased, despite some fluctuation during the study period, to 11.38% in 2005. The decrease in the 180-day readmission rate from 1997 to 2005 was statistically significant (P<0.001, χ2 test). For primary PPV alone, the 180-day readmission rate was 21.29% in 1997. There was a trend for this ratio to decrease during the study period, despite some fluctuation. This ratio significantly decreased to 14.69% in 2005 (P<0.001, χ2 test). For patients whose eyes were treated primarily with combined PPV and SB, the 180-day readmission rate was 22.99% in 1997. This rate significantly decreased to 16.55% in 2005 (P=0.005, χ2 test). When all patients with primary RRD were considered, the 180-day readmission rate was 18.95% in 1997. This rate progressively decreased with some fluctuation to 13.81% in 2005. This decrease of 5.14% in the readmission rate was statistically significant (P<0.001, χ2 test). The trend in the 180-day readmission rate for each surgical modality during the study period is plotted in Figure 2.
We also compared the 180-day readmission rate among different surgical modalities. In 1997, the 180-day readmission rates were 16.30, 21.29, and 22.99% for primary SB, primary PPV, and primary PPV+SB, respectively. The 180-day readmission rate was significantly lower for primary SB than for primary PPV and primary PPV+SB (both P<0.001, χ2 test). However, the rates did not statistically differ between primary PPV and primary PPV+SB (P=0.4948, χ2 test). In 2005, the 180-day readmission rates were 11.38, 14.69, and 16.55% for primary SB, primary PPV, and primary PPV+SB, respectively. The 180-day readmission rate was significantly lower for primary SB than for primary PPV and primary PPV+SB (both P<0.001, χ2 test). However, the rates did not statistically differ between primary PPV and primary PPV+SB (P=0.2351, χ2 test).
During the study period, the LOS significantly decreased for each surgical modality between 1997 and 2005 (from 6.64±4.71 to 6.00±4.31 days for primary SB; from 7.62±5.14 to 5.36±4.22 days for primary PPV; and from 10.37±7.23 to 6.96±5.54 days for primary PPV+SB; all P<0.01, t-test). The percentages of the decrease in LOS during this period were 9.6, 29.7, and 32.9% for SB, PPV, and PPV+SB, respectively.
In 1997, the hospitalization costs were US$US1327±641, 1470±661, and 1879±772 for primary SB, primary PPV, and primary PPV+SB, respectively. There were significant differences in the hospitalization costs among these three surgical modalities (all P<0.001, t-test). In 2005, the hospitalization costs were US$1515±644, 1478±587, and 1822±706 for primary SB, primary PPV, and primary PPV+SB, respectively. While the hospitalization costs for primary PPV+SB was significantly higher than those for primary PPV and primary SB (both P<0.001, t-test), there was no significant difference in hospitalization costs between primary PPV and primary SB (P=0.10, t-test).
Discussion
It was shown in this nationwide population-based study that from 1997 to 2005, there was a statistically significant trend towards more frequently employing PPV (with or without SB) for managing primary RRD (from 47.3 to 61.2%). During the same period, the 180-day readmission rates for the total sample, primary SB alone, primary PPV alone, and primary PPV+SB significantly decreased, indicating improvements in surgical outcomes for each surgical modality. We excluded cases undergoing primary pneumatic retinopexy in this study because of the small number of cases (<1.5%), and some of them were not admitted to a hospital (ie, ambulatory surgery). There was a consistent increase in the annual admissions for treatment of primary RRD during the 9-year study period. The causes may include an increasingly ageing population, increased numbers of people who have undergone cataract surgery, and a higher proportion of myopia in the population with time.
Ah-Fat et al10 reported a statistically significant rise in the proportion of primary RRD patients treated by primary PPV (with or without SB) from 10.9 to 32.3% between 1987 and 1996 in a tertiary referral centre in the United Kingdom. Their primary anatomical success rate rose from 76.6 to 84.7% (with a difference of 8.1%). However, that increase in the primary success rate was not statistically significant. That study included 77 and 149 primary RRD patients in 1987 and 1996, respectively. Minihan et al11 found that the vitrectomy was the primary procedure in 1 and 63% of cases in 1979 and 1999 in the vitreoretinal unit of St Thomas’s Hospital in the United Kingdom. The primary anatomical success rates were statistically similar: 79.8% in 1979 and 84% in 1999 (with a difference of 4.2%). That study included 124 and 126 primary RRD patients in 1979 and 1999, respectively. Sullivan et al16 reported an audit comparing results between different periods at Moorfields Eye Hospital (1967–1972 vs 1997) and showing primary success rate increasing from 75% to 80% (with a difference of 5%), but this was not found to be statistically significant. The case numbers were 452 and 153, respectively, in the years 1967–1972 and 1997. That study was interpreted as showing the effects of advancing surgical techniques in improving re-detachment treatment but not in primary RRD treatment. The absence of statistical significance in the improvement in the primary success rate in those three studies may have been caused by the small number of samples, although the possibility that there was indeed no improvement at all in outcomes during the study periods cannot be excluded. The 5.14% improvement in the primary anatomical success rate in our study, despite being smaller than that of the study by Ah-Fat et al (8.1%), achieved statistical significance because of the large number of cases in our study. This demonstrates one of the advantages of a study with a large number of cases, such as this nationwide population-based study.
A retrospective subregional audit showed a statistically significant improvement in the primary success rate from 76.1 to 88.8% during a period of increasing subspecialization (1989–1990 and 1995–1997).13 That study contained 142 and 160 cases in the two audit periods, respectively. Vitrectomy accounted for 4.9 and 42.5% cases in the initial audit and reaudit periods, respectively. However, this study concluded that increasing subspecialization, rather than change in surgical technique was responsible for the improvement in the primary success rate, since there was no significant difference in the primary success rate among different techniques. Another triple-cycle audit of primary RRD surgery over a 10-year period in Newcastle (UK) showed a statistically significant improvement in the total primary anatomical success rate from 67 to 87% between 1987 and 1997.12 The percentage of primary PPV significantly increased from 1.5 to 47.9%. However, that study did not present the primary success rate for each surgical modality. The authors concluded that the improvement in the total primary anatomical success rate was caused by greater individual experience, an increasing range of treatment options (especially the increased availability of vitrectomy), and audit-driven, organizational changes of increased subspecialization. In the third audit cycle of that study (1997), the primary PPV was performed in 47.9% of cases. This was close to our data, in which this proportion was 47.3% in 1997.
As a retrospective study, we did not control for the severity of disease (primary RRD) among different surgery groups. Conventionally, SB is employed for routine and simpler cases, and primary PPV is employed in more complicated cases.5, 6, 7, 8, 9 This may (at least partially) explain why the 180-day readmission rate for the primary PPV group was higher than that for primary SB group in our study. The significant decrease in the 180-day readmission rate for primary PPV (with or without SB) between 1997 and 2005 may have resulted from the shift of some of the ‘medium-complicated’ RRD cases from the primary SB group to the primary PPV group, and/or increased success rates in more complicated cases during this period owing to improvements in instrumentation and techniques (eg, the wide-angle fundus viewing system and high-speed vitrector).14 During the same period, the 180-day readmission rate also significantly decreased for primary SB. This may have resulted from a shift of the medium-complicated RRD cases to the primary PPV group, leaving only the ‘simplest’ RRD cases in the primary SB group. The techniques and technology of SB surgery have been established for decades, and no further enhancements have been introduced in recent years.15 Therefore, we do not think that the decrease in the 180-day readmission rate in the primary SB group was due to improvements in techniques or technology of SB. It may be argued that this improvement in the primary success rate in SB is from increased subspecialization.10, 12, 13 However, in the National Health Insurance System (Taiwan), the charge for retinal detachment surgery is paid for by the Bureau of National Health Insurance of the government only if the surgery is performed in a hospital. The charge is not paid if the surgery is performed in a clinic by a general ophthalmologist. In addition, in Taiwan, vitreoretinal surgery is routinely performed by ophthalmologists who were trained in vitreoretinal surgery during the resident or fellow stage. General ophthalmologists or ophthalmologists of other subspecialties usually refer cases to a vitreoretinal specialist and normally do not perform such surgery. Therefore, the increased primary success rate (either for primary SB or primary PPV±SB) observed during the study period should not have been due to increased subspecialization, unlike what was observed in the United Kingdom.10, 12, 13 Thus, we suggest that the causes for the increased primary success rate for each surgical modality (SB, PPV, and PPV+SB) and the total sample in our study may include more frequent employment of primary PPV as the surgical modality, improvements in the technique and technology of the vitrectomy, and greater individual experience.
The causes underlying the trends towards greater use of primary PPV for primary RRD in Taiwan may be multifactorial. Clinician might have gained the impression from their own clinical experiences that primary PPV is superior to SB in terms of safety and/or efficacy in greater proportion of RRD cases with improvements in techniques and technology of PPV. It was shown that clinical behaviour is driven by clinical evidence, especially when no large randomized clinical trials addressing the issue are available.19 In addition, increased availability of facilities for the vitrectomy across medical institutions in Taiwan may be another cause. On the other hand, financial reasons should not have been responsible for the trend towards a greater number of primary PPVs. In 1997, the average hospitalization cost for a primary SB was less than that for a primary PPV without SB (US$1327±641 vs 1470±661). In 2005, the average hospitalization cost for a primary SB did not statistically differ from that for a primary PPV without SB (US$1515±644 vs 1478±587). However, it still could not be excluded that a greater number of primary PPVs were chosen to comfort the surgeon, because PPV provides a higher sense of control intraoperatively for the surgeon.20
During the study period, the LOS significantly decreased for each surgical modality (primary SB alone, primary PPV alone, and primary PPV+SB) between 1997 and 2005. However, the percentage of decrease in the LOS was least in the primary SB group (9.6, 29.7, and 32.9% decreases for SB, PPV, and PPV+SB, respectively). This might reflect the striking progress made in PPV techniques and technology in recent years, in contrast to nearly no enhancements in SB techniques or technology during the same period.
In this study, we used the 180-day readmission rate as an indicator of the primary failure rate. Similar definition of primary success/failure by absence/presence of further retinal surgery has been adopted by the study of Sullivan et al.16 There must have been some patients with primary surgical failure (re-detachment), who chose not to undergo the re-operation. Given the negligible barriers to medical access and the serious visual impairment of untreated recurrent RD, we believe that the great majority of patients with re-detachment after primary RD repair would have selected to have the re-operation soon after onset of re-detachment.
In summary, in this nationwide population-based study from 1997 to 2005 in Taiwan, we found a significant trend towards more frequently employing primary PPV for the management of primary RRD. In addition, there was also a significant improvement in the primary success rate shown for each surgical modality group (SB, PPV, and PPV+SB) and for the total sample. This may have been related to more frequent use of primary PPV as the surgical modality, improvements in the techniques and technology of the vitrectomy, and greater individual experience. However, there remains scope for further improvement in primary success rate.
References
Gonin J . Le Decollement de la retine. Pathogenie-traitment. Libraire Payot: Lausanne, 1934.
Custodis E . Bedeutet die plombenaufnahung auf die sklera einen fortschritt in der operatven behandlung der netzhautablosung. Ber Zusammenkunft Dtsch Ophthalmol Ges 1953; 58: 102.
Norton EW . Intraocular gas in the management of selected retinal detachments. Trans Am Acad Ophthalmol Otolaryngol 1973; 77: OP85–OP98.
Machemer R, Buettner H, Norton EW, Parel JM . Vitrectomy: a pars plana approach. Trans Am Acad Ophthalmol Otolaryngol 1971; 75: 813.
Tani P, Robertson DM, Langworthy A . Prognosis for central vision and anatomic reattachment in rhegmatogenous retinal detachment with macula detached. Am J Ophthalmol 1981; 92: 611–620.
La Heij EC, Derhaag PF, Hendrikse F . Results of scleral buckling operations in primary rhegmatogenous retinal detachment. Doc Ophthalmol 2000; 100: 17–25.
Sharma T, Challa JK, Ravishankar KV, Murugesan R . Scleral buckling for retinal detachment. Retina 1994; 14: 338–343.
Devenyi RG, de Carvalho Nakamura H . Combined scleral buckle and pars plana vitrectomy as a primary procedure for pseudophakic retinal detachments. Ophthalmic Surg Lasers 1999; 30: 615–618.
Ambresin A, Wolfensberger TJ, Bovey EH . Management of giant retinal tears with vitrectomy, internal tamponade, and peripheral 360 degrees retinal photocoagulation. Retina 2003; 23: 622–628.
Ah-Fat FG, Sharma MC, Majid MA, McGalliard JN, Wong D . Trends in vitreoretinal surgery at a tertiary referral centre: 1987 to 1996. Br J Ophthalmol 1999; 83: 396–398.
Minihan M, Tanner V, Williamson TH . Primary rhegmatogenous retinal detachment: 20 years of change. Br J Ophthalmol 2001; 85: 546–548.
Johnson Z, Ramsay A, Cottrell D, Mitchell K, Stannard K . Triple cycle audit of primary retinal detachment surgery. Eye 2003; 16: 513–518.
Comer MB, Newman DK, George ND, Martin KR, Tom BD, Moore AT . Who should manage primary retinal detachments? Eye 2000; 14: 572–578.
McLeod D . Is it time to call time on the scleral buckle? Br J Ophthalmol 2004; 88: 1357–1359.
SPR Study Group. View 2: the case for primary vitrectomy. Br J Ophthalmol 2003; 87: 784–787.
Sullivan PM, Luff AJ, Aylward GW . Results of primary retinal reattachment surgery: a prospective audit. Eye 1997; 11: 869–871.
National Health Research Institute, Republic of China (Taiwan). Taiwan National Health Insurance Research Database, (Data provided by Bureau of National Health Insurance, Department of Health, Executive Yuan, Government of Taiwan). Taipei, Taiwan; 1997–2005.
Data from Directorate-General of Budget, Accounting and Statistics, Executive Yuan, Republic of China (Taiwan). Available athttp://www.dgbas.gov.tw/public/Attachment/782317174471.xls. accessed on 31 August 2007.
Thompson PL, Parson RW, Jamrozik K, Hockey RL, Hobbs MS, Broadhurst RJ . Changing patterns of medical treatment in acute myocardial infarction. Observations from the Perth MONICA Project 1984–1990. Med J Aust 1992; 157: 87–92.
Feltgen N, Weiss C, Wolf S, Ottenberg D, heimann H, SPR Study Group. Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment study (SPR Study): recruitment list evaluation. Study report no. 2. Graefes Arch Clin Exp Ophthalmol 2007; 245: 803–809.
Acknowledgements
This study is based in part on data from the National Health Insurance Research Database provided by the Bureau of National Health Insurance, Department of Health and managed by National Health Research Institute of Taiwan. The interpretation and conclusions contained herein do not represent those of Bureau of National Health Insurance, Department of Health or National Health Research Institute of Taiwan.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have no proprietary or commercial interest in any materials mentioned in this paper.
Rights and permissions
About this article
Cite this article
Ho, JD., Liou, SW., Tsai, CY. et al. Trends and outcomes of treatment for primary rhegmatogenous retinal detachment: a 9-year nationwide population-based study. Eye 23, 669–675 (2009). https://doi.org/10.1038/sj.eye.6703105
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6703105
Keywords
This article is cited by
-
Intraocular pressure outcomes after 23-G vitreoretinal surgery with two different transconjunctival sutureless sclerotomy techniques: vertical versus tunnel entry
International Ophthalmology (2022)
-
Computational fluid dynamics (CFD) simulation analysis on retinal gas cover rates using computational eye models
Scientific Reports (2021)
-
Recent trends in vitreoretinal surgery: a nationwide database study in Japan, 2010–2017
Japanese Journal of Ophthalmology (2021)
-
Evaluation of intraocular gas using magnetic resonance imaging after pars plana vitrectomy with gas tamponade for rhegmatogenous retinal detachment
Scientific Reports (2020)
-
Preoperative factors to select vitrectomy or scleral buckling for retinal detachment in microincision vitrectomy era
Graefe's Archive for Clinical and Experimental Ophthalmology (2020)