Abstract
Purpose
In an in vitrostudy, fixed-combination fortified vancomycin and amikacin ophthalmic solutions (VA solution) had the same potency and stable physical properties as the separate components. In this retrospective clinical study, we evaluated the efficacy of the topical VA solution in the treatment of bacterial corneal ulcer and comparison with separate topical fortified vancomycin and amikacin.
Methods
Separate topical fortified eye drops was used prior to January 2004 and switched to the VA solution afterwards in the treatment of bacterial corneal ulcer. The medical records of 223 patients diagnosed with bacterial corneal ulcers between January 2002 and December 2005 were reviewed retrospectively. There were 122 patients in the VA group and 101 in the separate group. Cure was defined as complete healing of the ulcer accompanied by a nonprogressive stromal infiltrate on two consecutive visits.
Results
No significant difference was found between the VA and separate therapy group. The mean treatment duration was 15.4 days in the VA group and 16.1 days in the separate therapy group. The average hospital stay was 5.4 days (VA) and 7.2 days (separate antibiotics). Stromal infiltration regressed significantly without further expansion in both groups. All corneal ulcers completely re-epithelialized without complications related to drugs.
Conclusion
VA solution provided similar efficacy to the conventional separate therapy in the treatment of bacterial corneal ulcers; however, it is more convenient and tolerable, promotes patient's compliance, avoids the washout effect, and reduces nurse utilization. Hence, VA solution is a good alternative to separate therapy.
Similar content being viewed by others
Introduction
Bacterial corneal ulcer is a destructive and emergent corneal disease, which should be treated immediately and properly to avoid further corneal damage and complications. Before the microorganism is identified, broad-spectrum antibiotic therapy is recommended. Combination therapy with an agent active against Gram-positive bacteria (eg, cafazolin or vancomycin) and an agent active against Gram-negative bacteria (eg, gentamycin, tobramycin, or amikacin) provides good initial broad-spectrum antibiotic coverage. Among these drugs, gentamycin or tobramycin and cefazolin are recommended as the first-line therapy, and amkacin and vancomycion are used as the second-line therapy. These antibiotics should initially be administered every 30–60 min. However, the frequent administration of multiple ophthalmic solutions is inconvenient for patients and reduces their compliance, or becomes a big workload for nurses. Moreover, only one of the multiple antibiotics will be of pharmacologic value, while the other has little therapeutic effect. If there is a single agent that is effective against both Gram-positive and Gram-negative pathogens, with the same effect as multiple fortified antibiotics, the alternative therapy would promote therapeutic efficiency.
An alternative to combination therapy is the use of fluoroquinolone monotherapy. Ciprofloxacin, a second-generation fluoroquinolone, has been reported to be as effective as the fortified multiple antibiotic therapy and is currently widely used as the first-line drug.1, 2, 3, 4, 5 However, Bower et al6 demonstrated that fluoroquinolones were not advisable as a single agent to treat vision-threatening bacterial ulcers because of gaps in Gram-positive coverage. Furthermore, several in vitro studies suggest that many bacteria, such as Staphylococcus aureus, Streptococcus, and coagulase-negative Staphylococcus species are becoming resistant to currently available fluoroquinolones.7, 8, 9 Moxifloxacin, a fourth-generation fluoroquinolone, has been reported to have similar efficacy compared with ciprofloxacin 0.3% and vancomycin 50 mg/ml.10 Although moxifloxacin has been suggested as a broad-spectrum agent in the treatment of bacterial keratitis, fluoroquinolone monotherapy is recommended only in compliant patients with less severe ulcers. In the medical center, most bacterial corneal ulcer patients are severe cases and these patients have usually received ciprofloxacin therapy or fortified first-generation cephalosporin and aminoglycoside solutions before referral. Hence, until the infecting microbe is identified, frequent (every 30–60 min) fortified vancomycin and amikacin solutions are usually used, which is inconvenient for both nurses and patients.
A second alternative to combination therapy is to mix the two drugs together. In our previous in vitro study, we found that the combination of fortified vancomycin and amikacin solutions into a so-called VA solution had the same antiseptic result as separate vancomycin and amikacin solutions.11 Moreover, the pH and osmolarity of the VA solution was closer to that of tears.11 The in vitro study suggested that the VA solution was as effective as the separate vancomycin and amikacin solutions but would cause less ocular irritation and be useful in the treatment of bacterial keratitis-pending clinical trials to determine its effectiveness and safety.
In this study, we compared the clinical efficacy and safety of the VA solution with those of separate vancomycin and amikacin solutions in the treatment of clinically suspected/diagnosed cases of bacterial keratitis.
Materials and methods
The VA solution clinical trial started since January 2004. We used separate topical fortified vancomycin and amikacin eye drops prior to January 2004 and switched to the VA solution afterwards in the treatment of bacterial corneal ulcer.
The diagnosis of bacterial corneal ulcer was based on clinical findings. Microbial keratitis is defined as an epithelial defect with stromal infiltration, with or without anterior chamber reaction. Because some features of fungal corneal ulcers are similar to those of bacterial corneal ulcers, before microbiologic data were available, clinically fungal keratitis was diagnosed on the basis of at least two of the following criteria: (1) patients with a history of trauma to the eye with vegetable or organic matter; (2) ulcers with irregular and feathery margins; (3) ulcers with satellite lesions; and (4) dry-looking ulcers. Initial smears and cultures were performed for patients with suspected microbial keratitis. The scraping smears were routinely processed for Gram staining and acid-fast staining. Culture specimens were sent to the microbiological laboratory for bacterial, fungal, and mycobacterial culture.
The preparation of fortified antibiotic eye drops has been described in a previous study.10 The concentration of topical vancomycin solution was 5% (50 mg/ml) and topical amikacin solution was 2% (20 mg/ml). The fixed combination VA solution was prepared by adding 5 ml of 10% vancomycin (the hydrochloride salt; that of Vancocin CP®, Eli Lilly, Japan K.K) solution to 5 ml of 4% amikacin (250 mg/2 ml, Amikin®, Bristol–Myers Squibb Srl, Italy) solution, so that each millilitre contained 50 mg of vancomycin and 20 mg of amikacin, which was equal to the concentration of each antibiotic in the separate solutions. All ophthalmic antibiotic solutions were placed in standard ophthalmic dispensing bottles by an aseptic technique. The solution bottles were preserved at 4°C.
To achieve the therapeutic level rapidly, each topical solution was given hourly. Therefore, patients were instructed to instill one drop of VA solution every hour, and the separate vancomycin and amikacin solutions were alternatively instilled every 30 min. Both eye drops were tapered depending on the clinical response. Usually, after the frequency of administration was reduced to every 3 h, the patient was discharged and followed up later in the outpatient clinic.
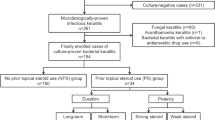
The medical records of all patients diagnosed with bacterial corneal ulcer who were admitted to the China Medical University Hospital, Taichung, Taiwan between January 2002 and December 2005 were selected for retrospective review. Patients were identified through a computerized diagnostic code search and patients with a diagnosis of microbial keratitis were enrolled in the retrospective historical controlled study. Ulcers diagnosed as fungal or viral infections were excluded.
The clinical records of 223 patients with a history of bacterial ulcer episodes were reviewed retrospectively. There were 122 patients treated with the VA solution and 101 patients treated with separate topical vancomycin and amikacin. Every patient's salient features, including age, sex, predisposing factors, results of microbiological examinations and treatment type, and baseline characteristics, including ulcer size, depth, location, and the presence of stromal thinning or hypopyon, were recorded. Associated ocular and systemic conditions, therapies received before referral, and concurrent factors for ulcer occurrence, healing, complications, duration of intensive therapy (hourly), clinical response, and length of hospital stay were also reviewed. These factors were compared between the two groups of patients. The primary outcome evaluation of this study included the number of days of therapy required, duration of hospital stay, healing time, and clinical signs. Cured was defined as no evidence of active bacterial infection, wound healing (re-epithelialization) complete (ie, absence of macropunctate staining), and inflammation resolved.
The research followed the tenets of the Declaration of Helsinki, and informed consent was obtained from each patient after counselling regarding the current hypothesis. The study was approved by the China Medical University Hospital institutional review board. Statistical analysis was performed by Student's t-test to compare the mean difference between the two groups. A P value <0.05 was considered statistically significant.
Results
Demographics
Bacterial corneal ulcer was diagnosed in 223 eyes of 223 patients during the 4-year study period. A total of 122 patients (57 males and 65 females) aged from 11 to 86 years (mean, 43.5±11.7 years) were enrolled in the VA solution group and 101 patients (42 males and 59 females) aged from 14 to 79 years (mean, 41.9±22.8 years) were enrolled in separate vancomycin and amkacin group. There was no significant difference between both groups in gender and mean age (P=0.42 and 0.18, respectively).
Microbiology
Out of 101 smear specimens in the separate antibiotic group, 59 (58.4%) smear specimens showed organisms on Gram staining. There were 36 Gram-negative bacilli, 5 Gram-positive bacilli, and 18 Gram-positive cocci. Forty-eight (47.5%) specimens had positive culture results. Pseudomonas aeruginosa was present in 30 cases, S. aureus in 12, Propionibacterium acnes in 4, and Serratia marcesceus in 2 cases. Out of the 122 smear specimens in the VA group, 75 (61.5%) specimens showed organisms on Gram staining. There were 44 Gram-negative bacilli, 10 Gram-positive bacilli, and 21 Gram-positive cocci. Fifty-seven (46.7%) specimens had positive culture results. P. aeruginosa was present in 37 cases, S. aureus in 12, Klebsiella pneumoniae in 2, and P. acnes in 6 cases. No pathogens were isolated after 2 weeks in the remaining specimens.
Predisposing factors
Predisposing factors were identified in 136 eyes (61.0%) in VA solution group and 85 eyes (69.7%) in separate vancomycin and amikacin group. The most common predisposing factor for microbial keratitis in both groups was contact-lens wear (43.1% and 52.9%), followed by ocular trauma (26.8% and 22.4%). Other predisposing factors were chronic ocular or systemic disorders, including blepharitis and dry eye (17.6% and 7.6%), lagophthalmos (2.9% and 2.3%), recent surgical intervention (2.3% and 1.8%), and diabetes (7.3% and 12.9%).
Treatment and outcome
There were no significant differences between both groups in ulcer size, depth, stromal thinning, and hypopyon. In the VA solution group, the mean ulcer size was 8.2±0.6 mm2, and in the separate therapy group it was 7.6±1.1 mm2 (P=0.46).
The mean duration of treatment was 15.4 days (range, 12–19 days) in the VA solution group and 16.1 days (range, 7–26 days) in the separate antibiotic group (P=0.61). All corneal ulcers were responsive to treatment with either topical VA solution or the separate therapy with an average hospital stay of 5.4 days (range, 3–9 days) and 7.2 days (range, 5–12 days), respectively (P=0.24). Stromal infiltration regressed significantly without further expansion in both groups.
There were no serious complications (perforation or enucleation and evisceration) in either group. All corneal ulcers completely re-epithelialized without limbal deficiency, symblepharon, or other complications related to the drugs.
Discussion
Our study shows that the VA solution was as effective and safe as the separate vancomycin and amikacin topical eye drops in the treatment of bacterial corneal ulcer. With intensive VA solution therapy, no serious complications such as perforation, enucleation, or evisceration occurred in any case, all ulcerative infiltrations regressed obviously without further progression and completely re-epithelialized. Moreover, the utilization of the nursing staff was largely reduced.
The biochemical activity and pharmacologic interaction between mixed drugs is a matter of concern in preparing fixed combination drugs. In our previous in vitro study, we found that the VA solution had the same potency to inhibit microbial growth as separate vancomycin and amikacin solution.11 In addition, the VA solution has a stable osmolarity and pH for at least 2 weeks. The osmolarity of the VA solution ranges from 193 to 202 mOsm, which is higher than that of amikacin (range, 45.00–48.67 mOsm) and vancomycin (range, 48.67–50.33 mOsm) solutions separately and within the well-tolerated range of human eye (150–450 mOsm).11, 12 The pH of normal tear film is 6.5–7.6.13 Topical drops with a pH between 6 and 9 are well tolerated by human eyes.12 From this point of view, the pH of VA solution (range, 5.01–5.18) was nearer that of normal tear film than the vancomycin solution (range 3.00–3.07). The pH of the VA solution and amikacin is not different. Hence, the VA solution has the same bactericidal effect but less drug irritation than vancomycin and amikacin solutions used separately. Clinically, all ulcers healed and all patients tolerated the treatment, supporting the results of the previous in vitro study.
Topical fortified antibiotics therapy, including gentamicin, tobramycin, amikacin, cefazolin, and vancomycin, has been widely used in bacterial corneal ulcer.14, 15, 16 For using as a broad-spectrum agent against Gram-positive and Gram-negative microorganisms, cefazolin combined with gentamycin, tobramycin, or commercial fluoroquinolones eye drops is recommended as the first-line therapy to treat bacterial corneal ulcer before culture result is available.14, 15, 16 Amikacin is active against many gentamycin- and tobramycin-resistant strains of Gram-negative bacilli,17 and vancomycin is recommended in keratitis caused by cefazolin-resistant Gram-positive microorganisms due to its high susceptibility for nearly all Gram-positive cocci.18, 19 Hence, amkacin and vancomycion are used as the second-line therapy. In a medical centre like ours, however, we used vancomycin and amikacin as the first-line therapy to treat bacterial corneal ulcer, because most patients were severe and had received fluoroquinolones or fortified first-generation cephalosporin and aminoglycoside solution before being referred.
Combining two drugs together has already been widely used in glaucoma therapy and satisfactory results were achieved.20, 21 Because glaucoma patients eventually require more than one medication noncompliance with recommended medical therapy is a major problem in the treatment of glaucoma. Clinical studies have shown that the efficacy and safety of the fixed combination of drugs are comparable to those observed with concomitant use of individual regimens. In addition, the combination therapy eliminates the need to wait for 5–10 min between drug instillations to avoid the dilution of drugs or washout from the cul-de-sac.21 Also, decreasing the frequency of medication can reduce the utilization of the nursing staff, and each instilled drop had sufficient pharmacologic effect, improving the treatment efficiency. The advantages of combination therapy, such as effectiveness, efficiency, and convenience, compared with concomitant therapy suggest that combinations of drugs should be recommended to replace the application of multiple drugs. Because corneal ulcer patients also require at least two medications, compliance of patients, washout effect of drugs, and workload of nurses are three major problems. Hence, in same way as in glaucoma therapy, fixed-combination VA solution is a good alternative to concomitant vancomycin and amikacin solutions in the treatment of bacterial keratitis.
There were some limitations of our study. First, we didn't compare the ocular irritation caused by VA solution and concomitant vancomycin and amikacin solutions. In our in vitro study,11 the pH and osmolarity of VA solution was nearer to that of normal tear film than either vancomycin or amikacin solutions separately. Hence, VA solution may be more tolerable than the vancomycin or amikacin solutions. Clinically, all patients tolerated the drug and none withdrew from treatment. Second, the microbiological findings were not adequate. The infecting microbes were identified in only 78 of 223 patients. The possible reason is that our hospital is a tertiary medical center, and most patients received broad-spectrum antibiotics before referral, which may have influenced the pathogen culture results.
Although VA solution was effective in treating bacterial corneal ulcer, we suggest that topical fluoroquinolones such as ciprofloxacin and ofloxacin or fortified first-generation cephalosporin and aminoglycoside solution should be used as the first-line drug to treat mild corneal ulcer to avoid drug resistance. In a medical centre, however, we suggest that VA solution can be used initially as a standard therapy to treat bacterial corneal ulcer, because most patients had received fluoroquinolones or fortified first-generation cephalosporin and aminoglycoside solution before being referred. For severe corneal ulcer, VA solution is recommended as the first choice.
In conclusion, topical VA solution provides similar therapeutic efficacy as separate vancomycin and amikacin solutions, but it is more convenient and tolerable to patients and reduces the workload of nurses. Hence, topical VA solution is a very good alternative to separate vancomycin and amikacin solutions.
References
Leibowitz HM . Clinical evaluation of ciprofloxacin 0.3% ophthalmic solution for treatment of bacterial keratitis. Am J Ophthalmol 1991; 112 (4 Suppl): 34S–47S.
Parks DJ, Abrams DA, Sarfarazi FA, Katz HR . Comparison of topical ciprofloxacin to conventional antibiotic therapy in the treatment of ulcerative keratitis. Am J Ophthalmol 1993; 115: 471–477.
Callegan MC, Engel LS, Hill JM, O'Callaghan RJ . Ciprofloxacin versus tobramycin for the treatment of staphylococcal keratitis. Invest Ophthalmol Vis Sci 1994; 35: 1033–1037.
Guzek JP, Chacko D, Kettering JD, Wessels IF, Aprecio RM . Comparison of topical ciprofloxacin to conventional antibiotic therapy in the treatment of experimental Pseudomonas aeruginosa keratitis. Cornea 1994; 13: 500–524.
Lauffenburger MD, Cohen KL . Topical ciprofloxacin versus topical fortified antibiotics in rabbit models of Staphylococus and Pseudomonas keratitis. Cornea 1993; 12: 517–521.
Bower KS, Kowalski RP, Gordon YJ . Fluoroquinolones in the treatment of bacterial keratitis. Am J Ophthalmol 1996; 121: 712–715.
Kowalski RP, Dhaliwal DK, Karenchak LM, Romanowski EG, Mah FS, Ritterband DC et al. Gatifloxacin and moxifloxacin: an in vitro susceptibility comparison to levofloxacin, ciprofloxacin, and ofloxacin using bacterial keratitis isolates. Am J Ophthalmol 2003; 136: 500–505.
Wilhelmus KR, Abshire RL, Schlech BA . Influence of fluoroquinolone susceptibility on the therapeutic response of fluoroquinolone-treated bacterial keratitis. Arch Ophthalmol 2003; 121: 1229–1233.
Goldstein MH, Kowalski RP, Gordon YJ . Emerging fluoroquinolone resistance in bacterial keratitis: a 5-year review. Ophthalmology 1999; 106: 1313–1318.
Aliprandis E, Ciralsky J, Lai H, Herling I, Katz HR . Comparative efficacy of topical moxifloxacin versus ciprofloxacin and vancomycin in the treatment of P. aeruginosa and ciprofloxacin-resistant MRSA keratitis in rabbits. Cornea 2005; 24: 201–205.
Lin JM, Tsai YY, Fu YL . The fixed combination of fortified vancomycin and amikacin ophthalmic solution—VA solution: in vitro study of the potency and stability. Cornea 2005; 24: 717–721.
Rexed U . The pH of the lachrymal fluid determined by a capillary micro-glass electrode. Acta Ophthalmol 1958; 36: 711–718.
Fechner PU, Teichmann KD . Ocular Therapeutics: Pharmacology and Clinical Application. Thorofare, NJ: Slack Inc., 1998.
Fong CF, Hu FR, Tseng CH, Wang IJ, Chen WL, Hou YC . Antibiotic susceptibility of bacterial isolates from bacterial keratitis cases in a university hospital in Taiwan. Am J Ophthalmol 2007; 144 (5): 682–689.
Bourcier T, Thomas F, Borderie V, Chaumeil C, Laroche L . Bacterial keratitis: predisposing factors, clinical and microbiological review of 300 cases. Br J Ophthalmol 2003; 87 (7): 834–838.
Bu P, Riske PS, Zaya NE, Carey R, Bouchard CS . A comparison of topical chlorhexidine, ciprofloxacin, and fortified tobramycin/cefazolin in rabbit models of Staphylococcus and Pseudomonas keratitis. J Ocul Pharmacol Ther 2007; 23 (3): 213–220.
Yu VL, Rhame FS, Pesanti EL, Axline SG . Amikacin therapy. Use against infections caused by gentamicin- and tobramycin-resistant organisms. JAMA 1977; 238: 943–947.
Bharathi MJ, Ramakrishnan R, Vasu S, Meenakshi R, Palaniappan R . In-vitro efficacy of antibacterials against bacterial isolates from corneal ulcers. Indian J Ophthalmol 2002; 50 (2): 109–114.
Sharma S, Kunimoto DY, Garg P, Rao GN . Trends in antibiotic resistance of corneal pathogens: part I. An analysis of commonly used ocular antibiotics. Indian J Ophthalmol 1999; 47: 95–100.
Ventura MP, Saheb NE, Solari HP, Saraiva VS, Vianna RN, Burnier Jr MN . Cost considerations of the new fixed combinations for glaucoma medical therapy. J Clin Pharm Ther 2005; 30: 251–254.
Zimmerman TJ, Zalta AH . Facilitating patient compliance in glaucoma therapy. Surv Ophthalmol 1983; 28: 252–258.
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary/Financial interest: The authors have no proprietary or financial interest in any material or device mentioned
Rights and permissions
About this article
Cite this article
Chiang, CC., Lin, JM., Chen, WL. et al. Comparison of topical fixed-combination fortified vancomycin–amikacin (VA solution) to conventional separate therapy in the treatment of bacterial corneal ulcer. Eye 23, 294–298 (2009). https://doi.org/10.1038/sj.eye.6703078
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6703078