Abstract
Aim
To estimate the arylesterase activity of serum paraoxonase-1 (PON1-ARE), which is reported to have an antioxidant and antiatherogenic potential and to correlate with plasma homocysteine (Hcys) and plasma TBARS in young adult central retinal venous occlusion (CRVO) patients.
Methods
A case–control prospective study carried out in 10 CRVO patients (mean age 27±5 years; 7 males, 3 females) and 20 healthy controls (mean age 29±5 years; 15 males, 5 females).
Results
The CRVO patients showed a significantly lowered serum PON1-ARE activity (P=0.009) along with a significant increase in the levels of plasma Hcys (P=0.018) when compared to the control subjects. There was a negative correlation between serum PON1-ARE and plasma Hcys levels (P=0.058) as well as between PON1-ARE and plasma TBARS levels (P=0.001) in the CRVO patients.
Conclusion
This is the first report of lowered serum PON1-ARE level as a risk factor for CRVO (OR= 1.108, CI=0.914, 1.314; P=0.296), which is found to correlate with oxidative stress.
Similar content being viewed by others
Introduction
Hyperhomocysteinemia (HHcys) has been reported to be associated with the risk of cardiovascular diseases.1 Recent studies have shown that the atherogenic effect of plasma homocysteine (Hcys) may be accounted for by the homocysteine thiolactone (HCTL).2 HCTL is formed from Hcys as a result of an error editing function of tRNA, which takes Hcys in the place of methionine. Inadvertent reactions of thiolactone with proteins are potentially harmful. Homocysteinylation of proteins can also occur as a result of incorporation of additional thiol groups, which may alter the physiochemical properties and biological activity of the proteins. Protein homocysteinylation may contribute to an increased atherothrombotic effect in individuals with HHcys.3 Anti-homocysteinyllysine antibodies have been detected in the plasma of healthy humans and their titre is elevated in patients with ischaemic heart disease or ischaemic cerebral stroke.4
Acute retinal vascular occlusive (RVO) disorders collectively constitute one of the major causes of seriously impaired vision, and still there are marked controversies reported in their pathogeneses, clinical features, and management.5 Of the various types of RVO disorders, CRVO is the most frequently occurring and clinically relevant type. The cause of CRVO is said to be multifactorial.6, 7 Mild HHcys has been reported as one of the risk factors for CRVO. However, the molecular mechanisms underlying the prothrombotic actions of Hcys are incompletely understood, especially in young adults with mild HHcys.8 We have recently reported HHcys as a risk factor for CRVO in the Indian population. Accordingly, 10% of the CRVO cases seen at this referral hospital were young adults in the age group of 20–40 years; 51% of the young adult CRVO cases recruited showed HHCys.9
In order to see a link between Hcys and other thrombotic factors, paraoxonase-1 (PON1) activity was determined in young adult CRVO cases with no other systemic complications manifested. PON1, a calcium-dependent esterase synthesized in the liver and contained in plasma high-density lipoproteins (HDL) tightly associated with apolipoprotein A-1, mitigates atherogenesis not only by inhibiting HDL oxidation, thereby preserving its function,10 but also by PON1 activity.11 PON1 has been found to have essential functions of arylesterase (ARE), organophosphatase, and lactonase activity depending on the substrate they act upon.12 PON1 is an essential antioxidant enzyme that possesses Peroxidase-like activity and also hydrolyses platelet-activating factor and bioactive phospholipids, which are involved in lipid peroxidation and vascular disease development.13 Apart from preserving the function of HDL, PON1 has been reported to beneficially influence atherogenesis through the inhibition of LDL oxidation.14
The PON1 enzyme, which has been implicated in the pathogenesis of atherosclerosis, has not been studied in the context of RVO diseases, although a decreased PON1 activity correlating negatively with malondialdehyde (MDA) levels that evaluates oxidative stress has been reported in patients with age-related macular degeneration.15 Serum PON1 is also one of the endogenous free-radical scavenging systems in the human body. Serum PON1, together with ARE, has been demonstrated to function as a single enzyme.16 Moreover, it has been found that serum PON1 activity accounted for more than 95% of the enzyme activity in serum, for its ARE activity, as tested by the in vitro hydrolysis of phenylacetate.17 In this study, the serum PON1 enzyme activity in terms of its ARE activity (PON1-ARE) has been estimated along with total plasma Hcys and oxidative stress marker in terms of TBARS in young adult CRVO patients. Serum PON1-ARE level can therefore be proposed as a marker for determining the susceptibility of CRVO cases to the deleterious effects of elevated Hcys and oxidative stress, as the enzyme has both antioxidant activity and HCTL activity.
Methods
As part of a 2-year prospective case–control study of consecutive young Indian adult CRVO cases seen at Sankara Nethralaya, a referral centre for vitreoretinal diseases in India, in the age group of 20–40 years (n=10, mean age 27±5 years), cases with no other systemic or ocular disease were included in the study. The inclusion and exclusion criteria were based on the ocular, biochemical, and haematological examinations apart from a detailed questionnaire. The exclusion criteria included a history of diabetes mellitus, renal disease, hypertension (130/90), cardiovascular disease, smoking, habitual alcohol intake, antioxidant supplements, trauma, or other major thrombotic episodes based on questionnaire and case records. Haematological diseases and coagulation disorders were ruled out by laboratory investigations. Other ocular diseases were ruled out by ophthalmic examination. Apparently healthy age and sex-matched controls (n=20; mean age 29±5 years; 15M, 5F) were recruited from the volunteers at the institution on the basis of their medical history and a detailed questionnaire. Informed consent was obtained from all the participants in the study. The author's institutional research board approved the study. All procedures pertaining to human subjects adhered strictly to the tenets of the Declaration of Helsinki. All the CRVO cases included in the study had unilateral CRVO. Of the 10 cases included in the study, 8 were non-ischaemic and 2 turned out to be ischaemic.
Blood samples were collected after ensuring overnight fasting. Serum and plasma were separated immediately by spinning at 3500 r.p.m. for 5 min and stored at −20°C until analysis within 1 month. Serum PON1-ARE activity, total plasma Hcys, and plasma TBARS were analysed. As calcium EDTA inhibits PON activity, no EDTA-containing tubes were used for PON assay. All the chemicals used in the assays were of analytical grade.
Determination of paraoxonase1 activity
Serum PON1-ARE activity was estimated using phenylacetate as the substrate and the rate of hydrolysis was measured spectrophotometrically in kinetic mode by detecting the increase in phenol concentration at 270 nm. Serum samples were prepared in buffer containing 10 mM Tris and 1 mM CaCl2, pH 8.0. Enzyme activity was expressed as μM phenylacetate hydrolysed per min per ml (IU/ml). A blank containing incubation mixture without serum was run simultaneously to correct for spontaneous substrate breakdown for activity determination.18
Determination of plasma homocysteine
Fasting plasma total Hcys analysis was performed using a commercial ELISA kit (Bio-Rad, CA, USA). Levels >15 μM were considered to be HHcys.
Determination of plasma thiobarbituric reactive substance (TBARS)
Plasma TBARS, a lipid peroxidation indicator of oxidative stress, was measured spectrophotometrically at 530 nm using MDA as standard (which reacts with thiobarbituric acid). The results were expressed as nmol MDA per ml.19, 20
Statistical analysis
The Student's t-test was used to compare continuous variables between groups. Pearson's correlation was employed to calculate the r-value. Statistical significance was defined as P<0.05. Multivariate logistic odds ratio analysis was performed to determine the risk factors associated with CRVO cases. The statistical analysis was performed using SPSS version 14.0.
Results
The serum PON1-ARE levels were found to be significantly lowered in the CRVO cases (P=0.009), with a mean value of 67±12 IU/ml as against the control, which showed a mean value of 79±12 IU/ml. There was a significant increase in plasma total Hcys (19.2±12 μ M) in the CRVO cases compared to the control, which showed a mean value of 11.04±3.8 μ M of Hcys (P=0.018). A significant increase in the oxidative stress marker TBARS (P=0.000) was observed in the CRVO patients (5.1±2 nmol MDA per ml) when compared to age and sex-matched controls (1.83±0.62) as given in Table 1. Table 2 shows the clinical details of the patient diagnosed as CRVO.
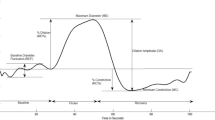
There was a negative correlation between PON1-ARE and plasma total Hcys (P=0.058) as well as between PON1-ARE and plasma TBARS (P=0.001) in the CRVO cases (Figures 1 and 2). A significant negative correlation was also seen for the serum PON1-ARE vs TBARS in the control subjects (P=0.000) (Figure 3), implying a strong relationship between PON1-ARE activity and oxidative stress as estimated by plasma TBARS levels. The multivariate logistic regression (OR) analysis revealed that PON1-ARE is a risk factor for CRVO (OR=1.108, CI=0.914, 1.314; P=0.296), apart from TBARS (OR=25.26, CI=1.292, 494.17; P=0.033*), whereas Hcys showed an OR of 0.871, CI of 0.608, 1.247; P=0.450 as shown in Table 3.
Discussion
Elevated Hcys has been reported as a risk factor for occlusive disease of the retina such as in CRVO.20 The current study reports on the decreased serum PON1-ARE activity along with HHcys and increased oxidative stress in young adult CRVO patients. High levels of plasma Hcys are toxic to the vascular endothelium, directly injuring the vessel endothelium by the release of free radicals creating an environment of hypercoagulability by modifying the vessel wall as well as by causing homocysteinylation, which affects the structure and functions of various proteins in the vascular system. An increase in Hcys levels leads to an elevation of thiolactone levels in human cells.4 In this context, the levels of PON1, which acts as lactonase as well as an antioxidant, could play an important role as a protective agent against the deleterious effect of elevated Hcys. The physiological substrate of PON1 is unknown,21 and measurements of PON1 activity are done by monitoring the rates of hydrolysis of exogenous substrates such as phenylacetate and paraoxon, although this may not quantify the degree of the antiatherogenic or antioxidant potential of PON1. As a strong correlation between the PON1 levels assessed by ELISA and the PON1 activity measurements has been reported, PON1 activity measurements qualify as markers for PON1 levels in serum as reported by Himbergen et al.22 In this study, the PON1 activity is measured in terms of its ARE activity using phenylacetate as the substrate.
This study reveals significantly elevated levels of plasma total Hcys and lowered levels of PON1-ARE activity along with increased plasma TBARS levels in young adult CRVO cases. Previous studies have revealed mild Hcys as a risk factor for CRVO in various populations including Asian Indians. The effect of Hcys on the disease pathology of CRVO is not well understood at the molecular level, eventhough its atherogenic effect is known. Recently, the relationship between Hcys and PON1 has been given by Jakubowski.23 This study reveals a negative correlation between serum PON1-ARE and plasma Hcys in CRVO patients (P=0.058). However, a larger study is needed to establish this relationship in the CRVO patients. High levels of Hcys correlating with the low levels of serum PON1-ARE activity and glutathione peroxidase activity have been shown in children with autism.24 Previous studies have also reported that HCTL activity of the PON1 protein detoxifies HCTL in human blood and could thus delay the development of atherosclerosis.25
The odds ratio analysis in this study shows TBARS and PON1-ARE as risk factors for CRVO, with TBARS showing significance. A decrease in PON1-ARE level associated with increasing oxidative stress has been reported in Bechet's disease26 as well as in diabetic and senile subjects suffering from cataract.27 This study also reveals a similar picture of PON1-ARE activity significantly decreasing with an increase in TBARS. The observed decrease in PON1-ARE activity is probably due to increased oxidative stress. Thus, a strong correlation between PON1 levels and TBARS seems to be associated with the pathology of CRVO. Baskol et al15 observed an increase in MDA levels related to decreased PON1 activity in patients with age-related macular degeneration.
To our knowledge, this is the first report that reveals a significant lowering of serum PON1-ARE activity in young adult CRVO patients. Low levels of serum PON1-ARE are also found to be significantly associated with increased oxidative stress in these CRVO cases. High level of Hcys, together with low PON1 activity, results in increased plasma HCTL concentration leading to protein N-homocysteinylation and the development and progression of vascular changes such as atherosclerosis.28 Martin et al29 have shown that patients with RVO are at increased risk of cardiovascular disease. Therefore, the treatment protocol in addition to reducing the elevated levels of Hcys, by nutritional supplements such as vitamin B12 and folate,30 can also include antioxidants as it may be associated with improving the PON1 levels. Supplementations of antioxidants, such as vitamin C31 and polyphenolic32 compounds, have been shown to increase the activity of serum PON1, which in turn reduces the lipid peroxidation and oxidative stress that plays a key role in the disease process.
References
Kazemi MB, Eshraghian K, Omrani GR, Lankarani KB, Hosseini E . Homocysteine level and coronary artery disease. Angiology 2006; 57 (1): 9–14.
Jakubowski H . Homocysteine thiolactone: metabolic origin and protein homocysteinylation in humans. J Nutr 2000; 30: 377S–381S.
Beltowski J . Protein homocysteinylation: a new mechanism of atherogenesis? Postepy Hig Med Dosw (online) 2005; 59: 392–404.
Jakubowski H . Anti-N-homocysteinylated protein autoantibodies and cardiovascular disease. Clin Chem Lab Med 2005; 43 (10): 1011–1014.
Hayreh SS . Prevalent misconceptions about acute retinal vascular occlusive disorders. Prog Retin Eye Res 2005; 24 (4): 493–519.
Lattanzio R, Sampirtro F, Ramonia A, Fattorini A, Brancato R . Moderate hyperhomocysteinemia and early-onset central retinal vein occlusion. Retina 2006; 26: 65–70.
Yildirim C, Yayali V, Tatlipinar S, Kaptanoglu B, Akpinar S . Hyperhomocysteinemia: a risk factor for retinal vein occlusion. Ophthalmologica 2004; 218: 102–106.
Parodi MB, Di Crecchio L . Hyperhomocysteinemia in central retinal vein occlusion in young adults. Semin Ophthalmol 2003; 18: 154–159.
Angayarkanni N, Barathi S, Coral K, Punitham R, Ramakrishnan S, Tarun S et al. Hyperhomocysteinemia and low methionine stress are risk factors for Central Retinal Venous Occlusion in an Indian population. Invest Ophthalmol Vis Sci 2007; 48: 1441–1446.
Aviram M, Rosenblat M, Bisgaier CL, Newton RS, Primo-Parmo SL, La Du BN . Paraoxonase inhibits high-density lipoprotein oxidation and preserves its function. A possible peroxidative role for paraoxonase. J Clin Invest 1998; 101 (8): 1581–1590.
Domagała TB, Łacinski M, Trzeciak WH, Mackness B . The correlation of homocysteine-thiolactonase activity of the paraoxonase (PON1) protein with coronary heart disease status. Cell Mol Biol 2006; 52 (5): 4–10.
Durrington PN, Mackness B, Mackness MI . Paraoxonase and atherosclerosis. Arterioscler Thromb Vasc Biol 2001; 21 (4): 473–480.
Yeunga DT, Josseb D, Nicholsona JD, Khanalc A, McAndrewc CW, Bahnsonc BJ et al. Structure/function analyses of human serum paraoxonase (HuPON1) mutants designed from a DFPase-like homology model. Biochim Biophys Acta 2004; 1702: 67–77.
Mackness MI, Arrol S, Abbott C, Durrington PN . Protection of low-density lipoprotein against oxidative modification by high-density lipoprotein associated paraoxonase. Atherosclerosis 1993; 104: 129–135.
Baskol G, Karakucuk S, Oner AO, Baskol M, Kocer D, Mirza E et al. Serum paraoxonase 1 activity and lipid peroxidation levels in patients with age-related macular degeneration. Ophthalmologica 2006; 220: 12–16.
Gan KN, Smolen A, Eckerson HW, La Du BN . Purification of human serum paraoxonase/arylesterase. Evidence for one esterase catalyzing both activities. Drug Metab Dispos 1991; 19 (1): 100–106.
Liao F, Zhu X-Y, Wang Y-M, Zhao Y-S, Zhu L-P, Zuo Y-P . Correlation of serum arylesterase activity on phenylacetate estimated by the integrated method to common classical biochemical indexes of liver damage. J Zhejiang Univ Sci B 2007; 8 (4): 237–241.
Cabana VG, Reardon CA, Feng N, Neath S, Lukens J, Getz GS . Serum paraoxonase: effect of apolipoprotein composition of HDL and the acute phase response. J Lipid Res 2003; 44: 780–792.
Devasagayam TP, Tarachand U . Decrease in lipid peroxidation in the rat kidney during gestation. Biochem Biophys Res Commun 1987; 145 (1): 134–138.
Ledwozyw A, Michalak J, Stepień A, Kadziolka A . The relationship between plasma triglycerides, cholesterol, total lipids and lipid peroxidation products during human atherosclerosis. Clin Chim Acta 1986; 155: 275–284.
Draganov DI, Teiber JF, Speelman A, Osawa Y, Sunahara R, La Du BN . Human paraoxonases (PON1, PON2, and PON3) are lactonases with overlapping and distinct substrate specificities. J Lipid Res 2005; 46: 1239–1247.
van Himbergen TM, Roest M, de Graaf J, Jansen EH, Jansen M, Hattori H et al. Indications that paraoxonase-1 contributes to plasma high density lipoprotein levels in familial hypercholesterolemia. J Lipid Res 2005; 46: 445–451.
Jakubowski H . Calcium-dependent human serum homocysteine thiolactone hydrolase. A protective mechanism against protein N-homocysteinylation. J Biol Chem 2000; 275 (6): 3957–3962.
Pasca SP, Nemes B, Vlase L, Gagyi CE, Dronca E, Miu AC et al. High levels of homocysteine and low serum paraoxonase 1 arylesterase activity in children with autism. Life Sci 2006; 78: 2244–2248.
Goa W, Wang YS, Zhang P, Wang HY . Hyperhomocyeinemia and low plasma folate as risk factor for CRVO, Case control study in Chinese population. Grafes Arch Clin Exp Opthalmol 2006; 244: 1246–1249.
Karakucuk S, Baskol G, Oner AO, Baskol M, Miza E, Ustdal M . Serum paraoxonase activity is decreased in the active stage of Behcet's disease. Br J Ophthalmol 2004; 88 (10): 1256–1258.
Hashim Z, Zarina S . Assessment of paraoxonase activity and lipid peroxidation levels in diabetic and senile subjects suffering from cataract. Clin Biochem 2007; 40 (9–10): 705–709.
Kerkeni M, Addad F, Chauffert M, Chuniaud L, Miled A, Trivin F et al. Hyperhomocysteinemia, paraoxonase activity and risk of coronary artery disease. Clin Biochem 2006; 39 (8): 821–825.
Martin SC, Butcher A, Martin N, Farmer J, Dobson PM, Bartlett WA et al. Cardiovascular risk assessment in patients with retinal vein occlusion. Br J Ophthalmol 2002; 86: 774–776.
Clarke R, Armitage J . Vitamin supplements and cardiovascular risk: review of the randomized trials of homocysteine-lowering vitamin supplements. Semin Thromb Hemost 2000; 26 (3): 341–348.
Calla MS, Lynch SM . Vitamin C preserves the cardio-protective paraoxonase activity of high-density lipoprotein during oxidant stress. Arch Biochem Biophy 2006; 452 (2): 129–137.
Abu-Amsha R, Croft KD, Puddey IB, Proudfood JM, Beilin LJ . Phenolic content of various beverages determines the extent of inhibition of human serum and low-density lipoprotein oxidation in vitro: identification and mechanism of action of some cinnamic acid derivatives from red wine. Clin Sci 1996; 91 (4): 449–458.
Acknowledgements
This study was funded by Vision Research Foundation (51-2004p), Sankara Nethralaya, Chennai, India.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Angayarkanni, N., Barathi, S., Seethalakshmi, T. et al. Serum PON1 arylesterase activity in relation to hyperhomocysteinaemia and oxidative stress in young adult central retinal venous occlusion patients. Eye 22, 969–974 (2008). https://doi.org/10.1038/sj.eye.6703062
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6703062
Keywords
This article is cited by
-
Follistatin-like 1 (FSTL1) levels as potential early biomarker of cardiovascular disease in a Mexican population
Heart and Vessels (2024)
-
Paraoxonase 1 and homocysteine metabolism
Amino Acids (2012)
-
Comparative modeling of PON2 and analysis of its substrate binding interactions using computational methods
Journal of Ocular Biology, Diseases, and Informatics (2010)