Abstract
Purpose
To compare the therapeutic efficacy of photodynamic therapy (PDT) to that of transpupillary thermotherapy (TTT) for polypoidal choroidal vasculopathy (PCV).
Methods
PDT or TTT was performed on 46 eyes of 46 patients with PCV; 19 eyes were treated with TTT (TTT group) and 27 eyes with PDT (PDT group). PCV was diagnosed by fundus examination, fluorescein angiography (FA) , and indocyanine green angiography (ICGA) . The best-corrected visual acuity (BCVA) in logarithm of the minimum angle of resolution (logMAR) units and OCT-determined foveal thickness were evaluated before and after treatment. For statistical analyses, the Student’s t-test and χ2 test were used.
Results
The number of treatments during the 12-month follow-up period was significantly higher in the TTT group (1.7 times) than in the PDT group (1.3 times; P=0.0134). The difference in the BCVA between the TTT and PDT groups at the baseline was not significant (P=0.3150), but the BCVA in the PDT group was significantly better than that in the TTT group at 3, 6, and 12 months after treatment (P=0.0093, P=0.0074, P=0.0006, respectively). The foveal thickness decreased markedly at 6 months after treatment in the PDT group (P<0.0001) but not significantly in the TTT group (P=0.8982). A vitreous haemorrhage was observed after treatment in two eyes in the TTT group.
Conclusions
BCVA was significantly better and the fovea was significantly thinner in the PDT group than in the TTT group after treatment. Thus, PDT may be more effective than TTT for the treatment of eyes with PCV.
Similar content being viewed by others
Introduction
Idiopathic polypoidal choroidal vasculopathy (PCV), first described by Yannuzzi et al,1 appears as reddish-orange lesions that are polypoidal dilations of the choroidal vascular network. The lesions are located immediately below the retinal pigment epithelium (RPE). The pathogenesis of PCV has not been fully determined, but PCV is considered to be a choroidal vascular disease characterized by a dilated network of vessels with multiple terminal aneurismal protuberances in a polypoidal configuration. Polypoidal choroidal vasculopathy frequently leads to an insidious decrease of visual acuity (VA) due to serosanguinous complications affecting the macula,2 but some eyes with PCV may remain clinically silent with no leakage, that is, asymptomatic polyps. Occasionally, eyes with PCV have an acute and severe loss of vision secondary to massive submacular or vitreous haemorrhage from spontaneously ruptured vessels.
Yannuzzi et al3 reported that 7.8% patients diagnosed with choroidal neovascularisation (CNV) secondary to age-related macular degeneration (AMD) had PCV and that 23.1% of these patients with PCV were non-white. In Japan, Sho et al4 reported that 23% patients were diagnosed as having PCV among patients with neovascular AMD, suggesting that the incidence of PCV in the Japanese is higher than in Caucasians.
Vedantham et al5 reported a case of PCV that was successfully treated with transpupillary thermotherapy (TTT). For TTT, the energy of the diode-laser is mainly absorbed by the choroidal tissues and elevates the choroidal temperature by approximately 10°C. The heat then induces an involution of the neovascular vessel indirectly rather than direct heating by conventional laser therapy.6
It has been reported that photodynamic therapy (PDT) with verteporfin is also safe and effective for treating PCVs with subfoveal involvement.2, 7 Quaranta et al8 first reported two cases of exudative PCV that were successfully treated with PDT. The responsiveness of PCV to PDT may be because it shares some similarities in its clinical properties and histology with the CNVs of eyes with AMD.
The purpose of this study was to compare the therapeutic efficacy of PDT to TTT for PCV.
Subjects and methods
Forty-six consecutive eyes of 46 patients with PCV, subfoveal exudation, and no history of treatment for PCV were treated with PDT with verteporfin or subthreshold TTT with a diode laser. The diagnosis of PCV was based on clinical examination, fluorescein angiography (FA), and indocyanine green angiography (ICGA). The criteria for a diagnosis of PCV were the presence of reddish-orange lesions, recurrent serosanguinous detachment of the retinal pigment epithelium (RPE), and dilated network of inner choroidal vessels with terminal hyperfluorescent aneurysm-like dilatations (polyps) on ICGA. The diagnosis for PCV was positive only in the presence of the ICG features or reddish-orange lesions. No case had a secondary CNV on clinical examination or FA before treatment.
Among the 46 eyes, 19 eyes were treated by TTT (TTT group) between January 2002 and May 2004, and 27 eyes were treated by PDT (PDT group) between June 2004 and January 2005. There were 3 women and 16 men in the TTT group, and 3 women and 24 men in the PDT group (P=0.6427; χ2 test; Table 1). The mean age at presentation was 72.2±6.6 (±SD) years in the TTT group and 70.1±8.5 years in the PDT group (P=0.3768, χ2 test).
TTT was performed as reported9 with a three-mirror Goldmann’s lens. The energy of the diode laser was delivered for 1 min through a slit-lamp-mounted delivery system. The threshold power was determined with an inferonasal test spot. No retinal blanching occurred during the TTT procedure. PDT with verteporfin was performed according to the guidelines of the treatment of age-related macular degeneration with photodynamic therapy (TAP) study.10 Five minutes after the completion of a standard verteporfin infusion, the laser beam at 689 nm was given.Indocyanine green angiography is regarded to be the gold standard in confirming a diagnosis of PCV, because it allows better detection of the choroidal circulation, and it delineates the distribution and extension of the polyps clearly.2 Silva et al7 reported that the ICG hot spots would probably indicate the size of the PCV lesions to be treated with PDT. In our study, the size of the laser spot for PDT was chosen to cover the polyps and the surrounding abnormally dilated choroidal vessels shown on ICGA plus an additional 1000-μm margin.2, 7
TTT or PDT was repeated if there was new or persistent leakage from the polyps on both FA and ICGA at the 3 month examination. The treatment end point was a complete absence of angiographic leakage on FA and ICGA. A total disappearance of polyps or dilated choroidal vessels was not always required.
The mean postoperative follow-up period was 30.9 months in the TTT-group and 16.2 months in the PDT-group. The best-corrected visual acuity (BCVA) in logarithm of the minimal angle of resolution (logMAR) units was measured before, and 1, 3, 6, and 12 months after treatment. Visual acuity was measured with a Japanese standard Landolt visual acuity chart and converted into logMAR visual acuity for statistical analyses. A significant improvement or decrease of the visual acuity was defined as a change of >0.2 logMAR units.
Foveal thickness was measured by optical coherence tomography (OCT; Stratus III OCT, Carl Zeiss, Dublin, CA, USA) using 5 mm scans before, and 1, 3, and 6 months after treatment. When the fixation was poor, the scans were centred on the fovea under video surveillance. An improvement of foveal thickness was defined as a >20% decrease in foveal thickness. Although an RPE detachment or subretinal fluid was noted to decrease in thickness in many patients, the quantitative evaluation of this change could not be obtained by the current OCT software.
To determine the significance of the changes in the two treatment groups, the Student’s t-test for continuous variables and χ2 test for categorical variables were used. The level of statistical significance was set at P<0.05.
Results
Eight of the 19 eyes (42.1%) treated with TTT and 21 of the 27 eyes (77.8%) treated with PDT had only one treatment during the 12-month follow-up period. Retreatment was performed for cases with persistent angiographic leakage (Figure 1). The mean number of follow-up treatments during the 12-month period was 1.74±0.73 in the TTT group and 1.26±0.51 in the PDT group (Table 2). The number of treatments was significantly higher in the TTT group than in the PDT group (P=0.0134, t-test). The size of treatment area was 5146.7±2070.9 μm in the TTT group and 5252.9±1939.3 μm in the PDT group. There was no significant difference between the TTT and PDT groups (P=0.8597, t-test).
Fundus photograph, fluorescein angiographic (FA) and indocyanine green angiographic (ICGA) images in representative cases treated with transpupillary thermotherapy (TTT) or photodynamic therapy (PDT). The fundus photographs are shown in the upper column, the FA images in the middle, and the ICGA images in the lower column. After TTT, the terminal hyperfluorescent aneurysm-like dilatations (polyps) are still present in the ICGA images and retreatment was performed. On the other hand, polyps disappear after PDT.
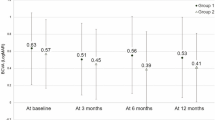
There was no significant difference in BCVA between the TTT and PDT groups at baseline and 1 month after treatment (P=0.3150, P=0.5739, respectively, t-test; Table 1). However, BCVA in the PDT group was significantly better than that in the TTT group at 3, 6, and 12 months after the treatment (P=0.0093, P=0.0074, P=0.0006, respectively, t-test; Figure 2). Compared with pretreatment BCVA, mean BCVA was significantly worse at 12 months after treatment in the TTT group (P=0.0111), but the difference was not significantly different in the PDT group (P=0.3243, paired t-test).
Comparison of logMAR visual acuity (VA) between the transpupillary thermotherapy (TTT) and photodynamic therapy (PDT) groups after treatment. There was no significant difference in VA between the TTT and PDT groups at baseline (P=0.3150).VA is significantly better in the PDT group than in the TTT group at 3, 6, and 12 months after treatment (P=0.0093, P=0.0074, P=0.0006, respectively).
In the TTT group, BCVA improved by >0.2 logMAR units in 1 eye (5.3%), remained unchanged in 9 eyes (47.4%), and worsened in 9 eyes (47.4%; Table 2). In the PDT group, BCVA improved in 10 eyes (37.0%), remained unchanged in 14 eyes (51.9%), and worsened in 3 eyes (11.1%). The number of eyes whose BCVA improved by >0.2 logMAR units was significantly higher in the PDT group than in the TTT group (P=0.0129, t-test).
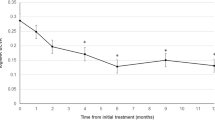
There was no significant difference in the pretreatment foveal thickness between the TTT and PDT groups (P=0.9628, t-test; Table 1). The foveal thickness decreased significantly at 6 months after treatment in the PDT group (P<0.0001), but there was no significant change in the TTT group (P=0.8982; paired t-test; Figure 3). The fovea was significantly thinner in the PDT group than in the TTT group at 6 months after treatment (P=0.0019, t-test; Table 2).
Comparison of OCT-determined foveal thickness between the transpupillary thermotherapy (TTT) and photodynamic therapy (PDT) groups after treatment. The fovea is significantly thinner at 6 months after treatment in the PDT group (P<0.0001), but there was no significant change in the TTT group (P=0.8982).
A decrease in the foveal thickness by >20% was achieved in 7 eyes (36.8%) in the TTT group and in 21 eyes (77.8%) in the PDT group (P=0.0051, χ2 test; Table 2).
A vitreous haemorrhage was observed after treatment in 2 (10.5%) eyes, and a secondary CNV developed in 3 (15.8%) eyes in the TTT group. In the PDT group, 4 (14.8%) eyes developed a secondary CNV (Table 2). Other complications, including RPE tears, photosensitivity, low back pain or catheter-induced complications, were not observed.
Discussion
Our investigation showed that the number of treatments during the 12-month follow-up period was significantly higher in the TTT group and that BCVA was significantly better in the PDT group than in the TTT group at 3, 6, and 12 months after treatment. The foveal thickness decreased markedly at 6 months after treatment in the PDT group but not significantly in the TTT group. Thus, our observations indicate that the visual outcome and foveal thickness after PDT were significantly better than those following TTT.
Men were predominant (87.0%) in both of our groups, and this male predominance was also reported for Japanese and Chinese patients in which approximately 70% of patients were men.11, 12, 13 This is in contrast to other series with predominantly Caucasian populations in which 15–47% were men.14, 15
It has been reported that 36% (5/14) of eyes with PCV and not treated had a worsening of visual acuity by >2 lines after a follow-up period of at least 2 years.11 Direct photocoagulation with an argon laser was the most widely used method to treat a PCV. Despite its widespread use, Lafaut et al14 reported unfavourable results of direct laser treatment for PCV due to a worsening of macular exudation after the treatment. A long-term follow-up study of eyes treated with laser photocoagulation targeting only polypoidal lesions showed bleeding and exudation from recurrent polypoidal lesions at the edges of the network of vessels, which resulted in a decrease of VA.16 Uyama et al13 reported that VA decreased in 24% (4/17) of the eyes treated with direct laser photocoagulation for PCV and that the visual outcomes in untreated eyes were better than those in treated eyes. These findings indicate that the visual function following the natural course of PCV or treatment with direct photocoagulation is poor.
Recently, TTT has been used to treat CNV in eyes with AMD,9 and to the best of our knowledge, there is only one case report of the successful treatment of a PCV by TTT.5 In this case, the macular serous detachment and reddish–orange lesions resolved one month after TTT, but VA remained unchanged during the 6-month follow-up period. They suggested that TTT caused a selective closure of the choroidal vascular network of leaking PCV by the hyperthermia-induced endothelial damage.
It has also been reported that PDT is effective for treating PCV with subfoveal involvement.2, 7 Chan et al2 reported that VA was stable or improved in 95% (21/22) eyes at the 1-year follow-up, and Silva et al7 reported that BCVA improved or stabilized in 17 of 21 (81%) eyes after one year. In our study, BCVA improved or stabilized in 24 of the 27 (88.9%) eyes one year after PDT. Thus, our results are comparable with those of previous reports. Overall, the visual outcomes following PDT are better than that after the natural history of PCV reported by Uyama et al11
As for the mechanism of efficacy of PDT for PCV, the relative uptake of verteporfin by the leaking choroidal vascular network in eyes with PCV is still uncertain, and it may be selective or non-selective.2 However, it has been reported that there is a selective uptake of verteporfin in CNV by low-density lipoprotein receptors,10 and a choroidal vascular remodelling for abnormally dilated choroidal vessels has been reported after PDT in eyes with central serous chorioretinopathy.17
Maberley et al18 reported that the effects of TTT and PDT on the VA and activity of the lesion were not significantly different for eyes with AMD. However, there was a significant difference in the baseline BCVA and size of the lesion between the TTT and PDT eyes in their study. In our study, BCVA, foveal thickness, and lesion size were not significantly different in the two groups at baseline, but BCVA was significantly better and the fovea was significantly thinner in the PDT group than in the TTT group after treatment. Thus, PDT may be more effective than TTT for PCV at 12 months after treatment.
A vitreous haemorrhage was observed in 2 (10.5%) eyes in the TTT group, and a secondary CNV developed in 3 (15.8%) TTT eyes and 4 (14.8%) PDT eyes. Uyama et al13 reported that 11% (2/18) of untreated eyes with PCV developed massive vitreous haemorrhage during a 20-month follow-up. It has been reported that a classic CNV was detected in 10 (9%) of 110 eyes with PCV at the first visit.4 Thus, there is a possibility that these complications might be more related to the underlying disease process than the specific treatment.
Although our study was retrospective and the sample size is small with a limited follow-up period, our results suggest that PDT is more effective than TTT in treating PCV.
References
Yannuzzi LA, Sorenson J, Spaide RF, Lipson B . Idiopathic polypoidal choroidal vasculopathy (IPCV). Retina 1990; 10: 1–8.
Chan WM, Lam DS, Lai TY, Liu DT, Li KK, Yao Y et al. Photodynamic therapy with verteporfin for symptomatic polypoidal choroidal vasculopathy: one-year results of a prospective case series. Ophthalmology 2004; 111: 1576–1584.
Yannuzzi LA, Wong DWK, Sforzolini BS, Goldbaum M, Tang KC, Spaide RF et al. Polypoidal choroidal vasculopathy and neovascularized age-related macular degeneration. Arch Ophthalmol 1999; 177: 1503–1510.
Sho K, Takahashi K, Yamada H, Wada M, Nagai Y, Otsuji T et al. Polypoidal choroidal vasculopathy: incidence, demographic features, and clinical characteristics. Arch Ophthalmol 2003; 121: 1392–1396.
Vedantham V, Kolluru C, Ramasamy K . Treatment of polypoidal choroidal vasculopathy with transpupillary thermotherapy: an interventional case report. Eye 2005; 19: 915–917.
Rogers AH, Reichel E . Transpupillary thermotherapy of subfoveal occult choroidal neovascularization. Curr Opin Ophthalmol 2001; 12: 212–215.
Silva RM, Figueira J, Cachulo ML, Duarte L, Faria de Abreu JR, Cunha-Vaz JG . Polypoidal choroidal vasculopathy and photodynamic therapy with verteporfin. Graefes Arch Clin Exp Ophthalmol 2005; 243: 973–979.
Quaranta M, Mauget-Faysse M, Coscas G . Exudative idiopathic polypoidal choroidal vasculopathy and photodynamic therapy with verteporfin. Am J Ophthalmol 2002; 134: 277–280.
Atarashi T, Tamaki Y, Inoue Y, Obata R, Muranaka K, Yanagi Y . Transpupillary thermotherapy for treatment of exudative age-related macular degeneration in Japanese patients. Eye 2004; 18: 615–618.
Treatment of age-related macular degeneration with photodynamic therapy (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: one-year results of 2 randomized clinical trials:TAP report 1. Arch Ophthalmol 1999; 117: 1329–1345.
Uyama M, Wada M, Nagai Y, Matsubara T, Matsunaga H, Fukushima I et al. Polypoidal choroidal vasculopathy: natural history. Am J Ophthalmol 2002; 133: 639–648.
Kwok AK, Lai TY, Chan CW, Neoh EL, Lam DS . Polypoidal choroidal vasculopathy in Chinese patients. Br J Ophthalmol 2002; 86: 892–897.
Uyama M, Matsubara T, Fukushima I, Matsunaga H, Iwashita K, Nagai Y et al. Idiopathic polypoidal choroidal vasculopathy in Japanese patients. Arch Ophthalmol 1999; 117: 1035–1042.
Lafaut BA, Leys AM, Snyers B, Rasquin F, De Laey JJ . Polypoidal choroidal vasculopathy in Caucasians. Graefes Arch Clin Exp Ophthalmol 2000; 238: 752–759.
Yannuzzi LA, Ciardella A, Spaide RF, Rabb M, Freund KB, Orlock DA . The expanding clinical spectrum of idiopathic polypoidal choroidal vasculopathy. Arch Ophthalmol 1997; 115: 478–485.
Yuzawa M, Mori R, Haruyama M . A study of laser photocoagulation for polypoidal choroidal vasculopathy. Jpn J Ophthalmol 2003; 47: 379–384.
Chan WM, Lam DS, Lai TY, Tam BS, Liu DT, Chan CK . Choroidal vascular remodelling in central serous chorioretinopathy after indocyanine green guided photodynamic therapy with verteporfin: a novel treatment at the primary disease level. Br J Ophthalmol 2003; 87: 1453–1458.
Maberley DA, Chew H, Ma P, Chang A, Hollands H, Maberley A . Comparison of photodynamic therapy and transpupillary thermotherapy for subfoveal choroidal neovascularization due to age-related macular degeneration. Can J Ophthalmol 2005; 40: 378–383.
Acknowledgements
This study was supported by the Ministry of Education, Culture, Sports, Science and Technology of Japan (Y Mitamura).
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary interests: None.
Meeting presentation: Presented in part at the 2006 ARVO annual meeting, Fort Lauderdale, FL, USA.
Rights and permissions
About this article
Cite this article
Mitamura, Y., Kubota-Taniai, M., Okada, K. et al. Comparison of photodynamic therapy to transpupillary thermotherapy for polypoidal choroidal vasculopathy. Eye 23, 67–72 (2009). https://doi.org/10.1038/sj.eye.6702996
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702996
Keywords
This article is cited by
-
Verteporfin PDT for non-standard indications—a review of current literature
Graefe's Archive for Clinical and Experimental Ophthalmology (2010)