Abstract
Purpose
To assess the safety and efficacy of topical lidocaine, levobupivacaine, and ropivacaine in cataract surgery with phacoemulsification.
Methods
One hundred and five patients scheduled for cataract surgery with topical anaesthesia were randomly allocated into 3 groups of 35 patients each to receive eye drops of lidocaine 2%, levobupivacaine 0.75%, or ropivacaine 1% every 5 min starting 30 min before surgery. Patients graded their pain using a 0–10-point verbal pain score (VPS) at different stages of the procedure. The levels of patient and surgeon satisfaction, the duration of surgery, complications, and the need for supplemental anaesthesia were recorded.
Results
There was no significant difference in duration of surgery and demographic variables among the groups. At the intraoperative period, end of surgery, and postoperative first hour the mean VPS in the lidocaine group was significantly higher than the others (P<0.01), but no significant difference was found between the levobupivacaine and ropivacaine groups. At incision and 24 h after surgery, it was not significantly different among the groups. Surgeon and patient satisfaction scores were significantly better in the levobupivacaine and ropivacaine groups than in the lidocaine group (P<0.01).
Conclusions
Topical anaesthesia with levobupivacaine and ropivacaine were safe, feasible and more effective than lidocaine in cataract surgery. Levobupivacaine and ropivacaine provided sufficient and long-lasting analgesia without the need of supplemental anaesthesia for each patient.
Similar content being viewed by others
Introduction
Topical anaesthesia for cataract surgery was first used by Knapp1 in 1884, and its use for phacoemulsification was first reported by Richard Fischmann, presented at the American Society of Cataract and Refractive Surgery meeting in April 1992. It is now a widely accepted procedure and has become a well-established technique in phacoemulsification surgery as an alternative to the retrobulbar and peribulbar techniques.2, 3, 4, 5, 6, 7 Because it is less invasive, reducing the risk of complications and eliminating complications from needle and systemic toxicity, topical anaesthesia has gained popularity among surgeons.8, 9, 10 Topical anaesthesia confers the advantages of relatively faster visual recovery and higher patient satisfaction, easy application, minimal discomfort on administration, rapid onset of anaesthesia, and lower cost.5, 11, 12, 13 However, the use of a topical anaesthetic permits the patient's full ocular movement during surgery, requires patient compliance, and may involve the administration of supplemental anaesthesia.5, 12
Unpreserved lidocaine is the most frequently used and safest agent in topical anaesthesia. Because of the short-acting effect, intraoperative and/or postoperative pain, and dissatisfaction may be associated with the use of topical lidocaine.13, 14, 15 Ropivacaine is a monoamide local anaesthetic (LA) agent with a long-acting effect and a great margin of safety. The cardiac and central nervous system toxicity is less than the others used in topical anaesthesia. Studies have shown that topical ropivacaine is at least as effective as lidocaine and is safe for use as a topical anaesthetic, although its onset of action is slower than that of lidocaine.12, 16, 17
Levobupivacaine, the S (−) isomer of bupivacaine, is less cardiotoxic than racemic bupivacaine. Ropivacaine is the first single isomer found, while levobupivacaine is the second to be studied clinically as a pure single isomer.18, 19, 20, 21 Although levobupivacaine is routinely used to provide regional anaesthesia, the results of clinical studies on its topical administration for ophthalmic surgery appears in only one study.22 In this study, we evaluated and compared the efficacy of topical application of lidocaine 2%, levobupivacaine 0.75%, and ropivacaine 1% in patients undergoing cataract surgery with phacoemulsification. The present study is the first report of a comparison of the effects of these three topical anaesthetic agents in cataract surgery.
Methods
After approval for the study had been obtained from the Ethics Committee, written informed consent that included an explanation of the study design and goals was obtained from all patients. This prospective, randomized, single-centre controlled, and comparative study comprised 105 patients who were selected based on the American Society of Anaesthesiologists Physical Status classification system (ASA I–III) to undergo planned routine phacoemulsification surgery. The exclusion criteria were as follows: axial length >26 mm or <22 mm, hypermature cataract, pseudoexfoliation syndrome, iris–lens synechias, previous use of miotics and/or small pupil, nystagmus, reported allergy to topical anaesthetics, unwillingness to receive topical anaesthesia, and poor patient cooperation, ie, those with dementia or hearing impairment.
After having undergone a routine preoperative ophthalmic examination of all patients, and standard monitorization including blood pressure, heart rate (HR) and oxygen saturation, using a computer-generated random order (Microsoft Excel), patients were randomized into 1–3 groups to receive eye drops containing lidocaine 2% (Aritmal®; Biosel, Istanbul, Turkey) (group 1, n=35), levobupivacaine 0.75% (Chirocaine®; Abbott, Elverum, Norvay) (group 2, n=35), and ropivacaine 1% (Naropin®; AstraZeneca, London, UK) (group 3, n=35). Five doses (∼40 μl per dose) of each anaesthetic were instilled on the ocular surface 5 min apart starting 30 min before surgery. Each patient's blood pressure, HR, and oxygen saturation value were obtained before receiving anaesthesia, just before the procedure, during surgery, and during a postoperative period. No significant differences among the groups were noted. No sedative systemic medications were given to the patients preoperatively or postoperatively. All patients received topical phenyleprine 2.5%, tropicamide 1%, and cyclopentolate 1% every 10 min for 30 min before surgery.
All operations were performed by the same surgeon (MB). Both patients and surgeon were blind to which anaesthetic agent was given. In the operation a 3.2 mm clear corneal temporal incision was made, after which sodium condroitin sulphate 4% and sodium hyaluronate 2% (Viscoat®; Alcon, TX, USA) were injected and 5.0 mm capsulorhexis was accomplished. Using the divide-and-conquer technique, the surgeon performed standard phacoemulsification, and implanted a foldable acrylic intraocular lens. The viscoelastic was removed, and the anterior chamber was reformed. No suture was used to close the incision. If the patient's verbal pain score (VPS) reached a value of 8 during surgery, a supplemental topical anaesthetic was administered.
Hemodynamic variables including the noninvasive blood pressure (NIBP) value, the results of an electrocardiogram (ECG), and heart rate (HR) were recorded every 5 min until the completion of surgery. To assess the pain score, a 10-point scale VPS was used (Table 1). Patients were asked to evaluate and grade the level of their pain and discomfort during surgery, at the end of the procedure, and 1 h and 24 h after surgery. The patient's pain score, the level of patient and surgeon satisfaction (from 0 to 10), the duration of surgery, the need for supplemental anaesthesia, and surgical complications were recorded. Clinical evaluations of every patient's VPS score were performed by an external ophthalmologist who was blind to which anaesthetic agents were used. Patients were discharged 1 h after the procedure following VPS evaluations and these pain scores were repeated at 24 h postoperatively.
Statistical analyses
Statistical analyses were performed with SPSS software (Statistical Package for the Social Sciences, version 9.0, SPSS Inc., Chicago, IL, USA). The correlation between the VPS of the three groups was performed using one-way ANOVA with post hoc Tukey's test. We used a χ2-test only for comparison among categorical variables such as sex. A P-value of less than 0.05 was considered significant.
Results
Table 2 shows the demographic data of the groups. There were no significant differences among the groups with regard to age, weight, and female/male ratio, and the mean duration of surgery. Nor were significant differences found in hemodynamic data, systolic blood pressure (SBP) values, diastolic blood pressure (DBP) values, HR, and oxygen saturation among the three groups.
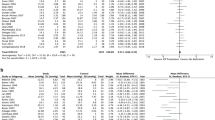
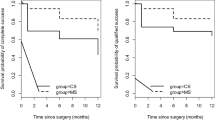
Verbal pain scores at various time intervals are shown in Figure 1. With respect to the VPS during incision, the difference among the groups was not statistically significant. Intraoperative mean VPS in the lidocaine group was significantly higher than that in the levobupivacaine and ropivacaine groups (P=0.005), but no significant difference was found between the levobupivacaine and ropivacaine groups. At the end of surgery and the postoperative first hour, mean VPS was significantly higher in the lidocaine group than that in the other two groups (P<0.01). However, no statistically significant difference was found among the groups in the mean VPS 24 h after surgery.
While two patients in the lidocaine group required supplemental anaesthesia, no patients in the levobupivacaine or ropivacaine group required additional anaesthesia. This difference was not statistically significant.
Both surgeon and patient satisfaction scores were significantly better in both the levobupivacaine and ropivacaine groups as compared to the lidocaine group (P<0.01), whereas the satisfaction scores did not show any significant difference between the levobupivacaine and ropivacaine groups (Table 3).
The rate and severity of intraoperative complications were similar among the groups. In the lidocaine group, one patient experienced intraoperative miosis. In addition, posterior capsule perforation occured in one patient in the ropivacaine group. No complications were encountered in the levobupivacaine group.
Discussion
In this study we aimed to compare the efficacy of three topical anaesthetic agents used in phacoemulsification surgery by comparing the patients’ subjective pain evaluations and satisfaction scores with surgeon's satisfaction levels. Both levobupivacaine and ropivacaine provided satisfactory analgesia during surgery. The mean VPS in the lidocaine 2% group was higher than that in the other two groups. We thought that this was related to lidocaine's acting time: close to the end of the procedure the effect of the lidocaine diminished and patients began to experience pain, so additional anaesthesia was administered to finish the surgery.
Di Donato et al22 in their recent study of 203 patients undergoing phacoemulsification surgery, clinically compared the efficiency of levobupivacaine 0.75% and lidocaine 4% as topical anaesthetic, and found that topical levobupivacaine 0.75% had the same efficacy and safety as lidocaine 4% in cataract surgery by phacoemulsification. There was an adequate block with a good level of satisfaction of surgeon and patients. They suggested that levobupivacaine 0.75% offers a new and acceptable choice for topical anaesthesia in cataract surgery. In our study, levobupivacaine 0.75% and ropivacaine 1% were more effective and feasible than lidocaine 2% as a topical anaesthetic agent used in phacoemulsification.
It has been shown that the pharmacokinetics of the LA agents probably has a role in the distribution of topically applied drugs to various eye tissues. In addition to corneal penetration, LA agents reach the iris and ciliary body by the conjunctival–scleral route.23, 24 Topical anaesthesia does not block all pain fibers from the iris and ciliary body, so manipulation of the iris might be expected to cause pain.25 As we know, some manipulations performed during phacoemulsification cause significant levels of pain. O’Brien et al1 showed that hydrodissection, phacoemulsification, lens aspiration, and intraocular lens insertion require the most manipulation of the iris and were associated with higher pain scores during surgery. In our study most patients in the levobupivacaine and ropivacaine groups reported either no pain or mild discomfort during all surgical stages per-operatively which implies high efficiency of these agents.
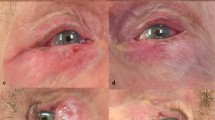
Local anaesthetic agents may exert a toxic effect on the cornea epithelium. Repeated use of LAs may result in an epithelial defect that can cause discomfort after surgery.26, 27 To avoid this adverse effects, the long-acting agents can be used in order not to repeat the instillation. For these reasons using less toxic and long-acting agents is safer and more reliable. It has been reported that intense or repeated application of topical anaesthetics can cause reduced lacrimation, breakdown of tear film layer, and epithelial cell sloughing. Although Zehetmayer et al3 found a significant defect in corneal transparency when either tetracaine or cocaine was used, Sun et al28 found no significant corneal toxicity in rabbits with topical bupivacaine and lidocaine. In our study, no cases of epithelial defect after the application of LA agent occurred during preoperative instillation or at the end of surgery.
In our study, we recorded the blood pressure value, HR, and peripheral oxygen saturation as indicators of intraoperative stress and pain. The data in all groups studied were not significantly different with respect to hemodynamic parameters.
Previous reports have noted that lidocaine 2–4%, oxybuprocaine 0.4%, and tetracaine 0.5% were associated with ocular discomfort and corneal toxicity.29, 30 Martini et al12 showed that topical ropivacaine is safe in endothelial toxicity and seemed to be a good alternative to lidocaine, but could cause transient corneal oedema. None of our patients in the ropivacaine group displayed any kind of corneal oedema.
Our study has some limitations as we could not evaluate the endothelial cell profiles postoperatively. Further studies are warranted to evaluate endothelial cell function in patients treated with topical levobupivacaine, and to confirm the lower corneal toxicity of this drug.
The results of this study indicate that long-acting LA agents such as levobupivacaine and ropivacaine can be used safely in order to provide topical anaesthesia in cataract surgery and to avoid the necessity for repeated instillation doses. This reflects a greater degree of comfort and compliance by the patient and could thus justify its use by the surgeon.
References
O’Brien PD, Fulcher T, Wallace D, Power W . Patient pain during different stages of phacoemulsification using topical anaesthesia. J Cataract Refract Surg 2001; 27: 880–883.
Novak KD, Koch DD . Topical anaesthesia for phacoemulsification: initial 20-case series with one month follow-up. J Cataract Refract Surg 1995; 21: 672–675.
Zehetmayer M, Radax U, Skorpic C, Menapace R, Schemper M, Weghaupt H et al. Topical vs peribulbar anaesthesia in clear corneal cataract surgery. J Cataract Refract Surg 1996; 22: 480–484.
Johnston RL, Whitefield LA, Giralt J, Harrun S, Akerele T, Bryan SJ et al. Topical vs peribulbar anaesthesia, without sedation, for clear corneal phacoemulsification. J Cataract Refract Surg 1998; 24: 407–410.
Sauder G, Jonas JB . Topical vs peribulbar anaesthesia for cataract surgery. Acta Ophthalmol Scand 2003; 81: 596–599.
Koch PS . Efficacy of lidocaine 2% jelly as a topical agent in cataract surgery. J Cataract Refract Surg 1999; 25: 632–634.
Tseng SH, Chen FK . A randomized clinical trial of combined topical-intracameral anaesthesia in cataract surgery. Ophthalmology 1998; 105: 2007–2011.
Duker JS, Belmont JB, Benson WE, Brooks Jr HL, Brown GC, Federman JL et al. Inadvertent globe perforation during retrobulbar and peribulbar anesthesia; patient characteristics, surgical management, and visual outcome. Ophthalmology 1991; 98: 519–526.
Morgan CM, Schatz H, Vine AK, Cantrill HL, Davidorf FH, Gitter KA et al. Ocular complications associated with retrobulbar injections. Ophthalmology 1988; 95: 660–665.
Fichman RA . Use of topical anaesthesia alone in cataract surgery. J Cataract Refract Surg 1996; 22: 612–614.
MacLean H, Burton T, Murray A . Patient comfort during cataract surgery with modified topical and peribulbar anaesthesia. J Cataract Refract Surg 1997; 23: 277–283.
Martini E, Cavallini GM, Campi L, Lugli N, Neri G, Molinari P . Lidocaine vs ropivacaine for topical anaesthesia in cataract surgery(1). J Cataract Refract Surg 2002; 28: 1018–1022.
Soliman MM, Macky TA, Samir MK . Comparative clinical trial of topical anaesthetic agents in cataract surgery: lidocaine 2% gel, bupivacaine 0.5% drops, and benoxinate 0.4% drops. J Cataract Refract Surg 2004; 30: 1716–1720.
Gills JP, Cherchio M, Raanan MG . Unpreserved lidocaine to control discomfort during cataract surgery using topical anaesthesia. J Cataract Refract Surg 1997; 23: 545–550.
Assia EI, Pras E, Yehezkel M, Rotenstreich Y, Jager-Roshu S . Topical anaesthesia using lidocaine gel for cataract surgery. J Cataract Refract Surg 1999; 25: 635–639.
Nicholson G, Sutton B, Hall GM . Ropivacaine for peribulbar anaesthesia. Reg Anaesth Pain Med 1999; 24: 337–340.
Luchetti M, Magni G, Marraro G . A prospective randomized double-blinded controlled study of ropivacaine 0.75% vs bupivacaine 0.5%-mepivacaine 2% for peribulbar anaesthesia. Reg Anaesth Pain Med 2000; 25: 195–200.
McGlade DP, Kalpokas MV, Mooney PH, Buckland MR, Vallipuram SK, Hendrata MV et al. Comparison of 0.5% ropivacaine and 0.5% bupivacaine in lumbar epidural anaesthesia for lower limb orthopaedic surgery. Anaesth Intensive Care 1997; 25: 262–266.
McLure HA, Kumar CM, Ahmed S, Patel A . A comparison of lidocaine 2% with levobupivacaine 0.75% for subtenon block. Eur J Anaesthesiol 2005; 22: 500–503.
McLeod G, Burke D . Levobupivacaine. Anesthesia 2001; 56: 331–341.
Glaser C, Marhofer P, Zimpher G, Heinz MT, Sitzwohl C, Kapral S et al. Levobupivacaine vs racemic bupivacaine for spinal anaesthesia. Anaesth Analg 2002; 94: 194–198.
Di Donato A, Fontana C, Lancia F, Di Giorgio K, Reali S, Caricati A . Levobupivacaine 0.75% vs lidocaine 4% for topical anaesthesia: a clinical comparison in cataract surgery. Eur J Anaesthesiol 2007; 24: 438–440.
Schoenwald RD, Deshpande GS, Rethwisch DG, Barfknecht CF . Penetration into the anterior chamber via the conjunctival/scleral pathway. J Ocul Pharmacol Ther 1997; 13: 41–59.
Ahmed I, Patton TF . Importance of the noncorneal absorption route in topical ophthalmic drug delivery. Invest Ophthalmol Vis Sci 1985; 26: 584–587.
O’Brien PD, Fitzpatrick P, Power W . Patient pain during stretching of small pupils in phacoemulsification performed using topical anaesthesia. J Cataract Refract Surg 2005; 31: 1760–1763.
Rosenwasser GO . Complications of topical ocular anaesthetics. Int Ophthalmol Clin 1989; 29: 153–158.
Durham RA, Sawyer DC, Keller WF, Wheeler CA . Topical ocular anaesthetics in ocular irritancy testing: a review. Lab Anim Sci 1992; 42: 535–541.
Sun R, Hamilton RC, Gimbel HV . Comparison of 4 topical anaesthetic agents for effects and corneal toxicity in rabbits. J Cataract Refract Surg 1999; 25: 1232–1236.
Neilsen PJ . Immediate visual capability after cataract surgery: topical vs retrobulbar anaesthesia. J Cataract Refract Surg 1995; 21: 302–304.
Dinsmore SC . Drop, and then decide approach to topical anaesthesia. J Cataract Refract Surg 1995; 21: 666–671.
Acknowledgements
We have no personal or financial relationships that have any potential to inappropriately influence (bias) our actions or the manuscript, and no financial or other potential conflicts of interest exist (including involvement with any organization with a direct financial, intellectual, or other interest in the subject of the manuscript) regarding the manuscript. There are no grants and sources of financial support related to the topic or topics of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Borazan, M., Karalezli, A., Akova, Y. et al. Comparative clinical trial of topical anaesthetic agents for cataract surgery with phacoemulsification: lidocaine 2% drops, levobupivacaine 0.75% drops, and ropivacaine 1% drops. Eye 22, 425–429 (2008). https://doi.org/10.1038/sj.eye.6702973
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702973