Abstract
Purpose
To report the clinical features of the eye of young patients with an idiopathic macular epiretinal membrane (ERM), and the visual outcomes after the surgical removal of the ERM.
Methods
A retrospective review of the medical records of eight young patients (age, 23–39 years; mean, 32.5 years) with an idiopathic macular ERM was performed. The patients underwent vitrectomy and removal of the ERM with peeling of the internal limiting membrane (ILM). The pre- and postoperative visual acuity and intra- and postoperative complications were investigated.
Results
Ophthalmoscopically, the ERMs in seven eyes were white, opaque, and dense, while one was grayish-white and less dense. A posterior vitreous detachment was not present and the ERM adhered strongly to the underlying retina in all eight eyes. The mean best-corrected visual acuity (BCVA) preoperatively was 20/140 (Snellen; range: 20/250–20/63), and the BCVA improved significantly to 20/30 (range: 20/40–20/20) postoperatively with an average follow-up of 14.6 months (range: 6–42 months; Wilcoxon sign-rank test, P<0.001). An improvement of >7 lines was observed in seven of eight eyes. A recurrence of an ERM without involving the macula was detected in one eye (12.5%).
Conclusions
The clinical features of the ERMs in young patients are different from those in elderly patients, eg, thicker, more adherent to the retina, and still attached to the vitreous. Vitrectomy and removal of ERM with ILM peeling are effective and safe surgical procedures. Removal of the ILM may minimize the recurrence of an ERM.
Similar content being viewed by others
Introduction
A macular epiretinal membrane (ERM) is a non-vascular fibrocellular proliferation that develops on the surface of the internal limiting membrane (ILM) resulting in retinal wrinkling and distortion. An ERM is usually idiopathic and is found predominantly in patients over 50 years of age.1 It can lead to different degrees of visual disturbances, and vitrectomy with the removal of the ERM has become the established surgical procedure for the treatment of an ERM in elderly patients.2, 3, 4
As opposed to elderly patients, an idiopathic ERM is very rare in young patients, but when it does occur, it can lead to significant visual disturbances. In young patients, a non-progressive course and spontaneous separation of the macular idiopathic ERM from the retina have been described with good visual recovery. Therefore, a conservative approach has been suggested for eyes with an ERM, and only observation was advocated in some cases.5, 6, 7, 8, 9, 10 Other studies have found that the visual acuity (VA) improved after vitrectomy, and vitrectomy with the removal of the ERM has been recommended in eyes whose vision was significantly reduced by the ERM. However, a high recurrence of ERM was also observed.11, 12, 13, 14 Because of these contradictory recommendations, more studies are necessary to determine the optimal management of young patients with a macular idiopathic ERM.
The benefits of ILM peeling have been reported for macular hole closures, and the prevention of recurrent postoperative formation of an ERM.15, 16 The incidence of ERM recurrences were significantly lower in elderly ERM patients undergoing ILM peeling compared with those without ILM peeling.17, 18, 19
The purpose of this study was to determine the clinical features and surgical outcomes following the removal of an idiopathic macular ERM in young patients who underwent vitrectomy with ILM peeling for ERM removal.
Methods
The medical records of eight eyes of eight consecutive patients with severe reduction of VA and metamorphopsia because of an idiopathic ERM were studied. The Ethics Committee of the School of Medicine, Zhejiang University, approved the procedures used in this study and the procedures were conformed to the Tenets of the Declaration of Helsinki.
The patients were less than 40 years of age and were examined between 2002 and 2005. They had completed preoperative and postoperative ocular examinations including measurement of the best-corrected visual acuity (BCVA) with a standard Snellen chart, slit-lamp examination of the anterior segment, +90 D lens-aided fundus biomicroscopy, colour fundus photography, and fluorescein angiography. No ocular trauma or disease was detected in any eye.
The preoperative appearance of the ERM and condition of the posterior vitreous were determined by fundus biomicroscopy. A complete posterior vitreous detachment (PVD) was considered to be present if a Weiss ring was detected.
Surgical techniques
All patients consented to surgery after a discussion of the risks and benefits. The surgical technique consisted of a standard three-port pars plana vitrectomy using 20-gauge instruments. After core vitrectomy, the posterior hyaloid was detached around the optic nerve head by active aspiration with a vitrectomy probe. Then a sharp vitreoretinal pick or bent microvitreoretinal blade was used to pick-up an edge of the epiretinal membrane, which was then grasped with the intraocular forceps, separated from the underlying retina, and removed from the eye.
To prepare the indocyanine green (ICG) solution, 25 mg of commercially available ICG powder was dissolved in 5 ml of the package solvent. Then 1 ml of this solution was diluted with 5 ml of buffered saline solution (BSS) to a final concentration of 0.1%. After the removal of the ERM, 0.2–0.4 ml of the 0.1% ICG solution was injected into the vitreous over the macular area. After 1 min, the dye was washed out, and 3 to 4 disc diameters of the ILM centred on the fovea was peeled off. At the end of surgery, the peripheral retina was examined with scleral depression to search for retinal tears and dialysis.
Patients were examined preoperatively and at 1 day, 1 week, 2 weeks, 1 month, and 2 months after surgery, and at different times thereafter. The follow-up examinations included: BCVA, slit-lamp examination of the anterior segment, intraocular pressure measurements, +90 D lens-aided fundus biomicroscopy, colour fundus photography, and fluorescein angiography. The Snellen BCVA was converted into the logarithm of the minimum angle of resolution (logMAR) for statistical analyses. The Wilcoxon sign-rank test was used to compare a patient's preoperative and postoperative BCVA.
Results
Clinical features
The eight patients were made up of six men and two women whose mean age was 32.5 years with a range from 23 to 39 years. The ocular findings for the eight subjects are summarized in Table 1. The most common complaint was the reduction of VA and metamorphopsia, and the symptoms in the involved eyes lasted from 3 to 5 months (mean, 4 months). The postoperative follow-up period ranged from 6 to 42 months (mean, 14.6 months).
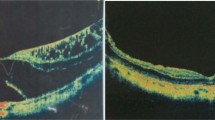
Lens-aided fundus biomicroscopy showed that the ERM appeared as a white, thick, opaque, and dense membrane. The retinal vessels near the ERM were very tortuous, and the retina had radiating folds that obscured the appearance of the underlying retina in seven eyes (Figure 1a). In the remaining eye, the ERM was grayish-white, and the retina was semi-transparent with fine tortuous blood vessels and radiating folds over the macula (Figure 2a). Fluorescein angiography demonstrated late hyperfluorescence in four eyes. A posterior vitreous detachment was not observed in any of the eyes on the initial examination, and was created in each of the eyes at the time of surgery.
Pre- and postoperative fundus photographs of Case 6. (a) The ERM appears as a white, opaque, and dense membrane. The retinal vessels are tortuous, and the retina has radiating folds around the ERM. The ERM blocks the underlying retina and vasculature. (b) Fundus photography at 3 months postoperatively. The ERM has completely disappeared, and the appearance of the macular has returned to normal.
Pre- and postoperative fundus photographs of Case 3. (a) Preoperative fundus photograph showing a grayish-white, semi-transparent ERM with fine tortuous vessels and radiating retinal folds around the macula. (b) Fundus photography at 1 month postoperatively. The ERM has completely disappeared and the macular has returned to normal. (c) Fundus photography at 3 month postoperatively. White and contractile ERM with radiating retinal folds can be seen at the temporal edge of the peeled ILM (arrow).
The ERM was strongly adherent to the underlying retina, however a complete removal of the ERM was possible in all eight eyes. The ILM could be easily identified after the ICG staining and peeled in all eight eyes. Local ILM defects were noted near to the centre of the ILM peeled area in three eyes indicating that segments of the ILM had been removed together with the ERM during the removal of the ERM.
The fellow eye in each of the eight patients was normal.
Visual acuities
The mean preoperative BCVA was 20/140 with a range from 20/250 to 20/63, and the mean of the final postoperative BCVA was 20/30 with a range from 20/40 to 20/20. This improvement was significant (Figure 3, Wilcoxon sign-rank test, P<0.01). The visual acuity improved by >3 lines in all eyes with a mean improvement of 7.6 lines. Seven of the eight eyes (87.5%) had an improvement of >7 lines.
Intraoperative and postoperative complications
Slight intraretinal and preretinal haemorrhages occurred during ERM removal in five eyes, and the bleeding stopped within a few days without consequences in all cases. No pre-existing or iatrogenic peripheral or posterior retinal breaks were found.
In one eye (12.5%), a recurrent ERM was detected at the 3-month follow-up examination. It was located at the temporal peeled-edge of the ILM, and this case is only followed as the ERM did not alter the VA and only a slight metamorphosia was reported (Figures 2b and c). No recurrence of a macular ERM was seen in any of the other eyes (Figure 1b).
No postoperative retinal detachment, persistent increase in intraocular pressure, or increase in cataract formation was noted in any of the operated eyes during the follow-up period.
Discussion
A spontaneous separation of a macular idiopathic ERM from retina with visual recovery has been described in some cases, but in most of the young patients with a vision-altering ERM, the vision decreases progressively. Thus, these patients are quite eager to undergo the surgical intervention. Banach et al11 reported that 10 of 13 eyes (77%) of young patients with an ERM and initial VA <20/50 had a mean visual improvement of 3.7 lines with a recurrence rate of 23% after ERM peeling with a mean follow-up of 22.5 months. Smiddy et al12 performed vitrectomy membrane peeling on 11 young patients with an ERM, and reported a mean visual improvement of 3.7 lines with a recurrence rate of 36% after a mean follow-up of 33.4 months. Benhamou et al14 reported on the surgical outcomes of 13 idiopathic macular ERM cases with preoperative VA of 20/100, and stated that the mean improvement of the VA was 3.3 lines with a recurrence rate of 25%. In our study, the mean improvement of vision was 7.6 lines, and seven of eight eyes had an improvement of >7 lines and a recurrence rate of 12.5%. These results demonstrate that the BCVA can be significantly improved after surgery in eyes of young patients with visually significant ERM.
Comparing our results to those reported for young ERM patients, no modifications of the surgical procedures were made except for the intentional ILM peeling in our study. Although Smiddy et al12, 13 observed some fragments of the ILM on the surgically removed ERM, they did not intentionally peel the ILM during the surgery. Banach and Benhamou et al11, 14 also did not intentionally peel the ILM during the surgery. The removal of the ILM during macular surgery in elderly patients is generally done to enhance the surgical outcome.15, 16, 20 Removal of the ILM was expected to reduce the recurrence rates by limiting the myofibroblasts proliferation, consequently minimizing the development of a recurrent ERM. Researches have also demonstrated that the surgical outcome is better and ERM recurrence is significantly lower in elderly ERM patients undergoing ILM peeling compared with those without ILM peeling.17, 18, 19
The effect of intentional ILM peeling during ERM surgery in young patients has not been reported. In our cases, the improvement of postoperative BCVA is better than those in the earlier reports. An ERM developed at the temporal edge of the peeled ILM 3 months postoperatively in one patient, however the macular area was not involved. Kwok et al18 also described the development of an ERM at the edge of the peeled ILM in elderly ERM patients. Although we cannot state definitively that ILM removal reduces the recurrence rates due to the small number of cases and the absence of a control group, the lower recurrence rate of macular ERM in the eyes of our study suggests that ILM peeling may be beneficial in young patients.
The efficacy of ICG to stain and assist in visualization of ILM and increases the ease of peeling the ILM, which make ILM peeling procedure safer and faster in macular surgery, is well known. However, adverse effects of ICG –assisted ILM peeling in macular surgery, for example, peripheral visual field defect, RPE atrophy, and optic nerve atrophy, have been subsequently reported.21, 22, 23, 24 Thus, the use of ICG during the macular surgery is still controversial. Some modified techniques for safer ICG-assisted peeling of the internal limiting membrane during vitrectomy and safer intraocular dyes have been reported.25, 26 Nevertheless, ICG is still commonly used in macular surgery. However, it is generally considered that the lowest effective concentration of ICG should be used in order to decrease the potential risk of its toxicity.
In contrast to the thin, cellophane- or sheet-like appearance of a typical macular pucker in elderly patients, seven of eight eyes in our series had thick, opaque, and dense ERM, and they were attached to the posterior vitreous hyaloid. In addition, the ERMs were adherent firmly to the underlying retina at the time of operation. This characteristic of the ERM in our young patients is consistent with the previous reports.8, 9, 10, 11, 12, 13, 14
Although the aetiology and pathophysiological mechanism controlling the development of an idiopathic ERM remains speculative, histological studies on surgically obtained ERMs have shown proliferation of cells derived mainly from retinal glial or retinal pigment epithelial cells. Smiddy et al12, 13 studied surgically-excised idiopathic macular ERM, and found that myofibroblasts, myoblastic differentiated retinal pigment epithelial cells, and fibrous astrocytes, and new collagen formation were more commonly found in the ERMs of young patients than those of elderly patients. This would indicate a more rapidly changing, contractile tissue in young patients compared with the usually more quiescent features in elderly patients.
The association of a PVD with the formation of an ERM in elderly patients has been described.1, 27, 28 The tractional forces of a PVD may induce focal disruptions in the ILM which would allow retinal glial or retinal pigment epithelial cells to gain access to the ILM and proliferate along the retinal surface.10, 11 Fifteen percent of young patients with an ERM have a PVD;11, 14 whereas Smiddy et al12 reported all of their young patients with an ERM had a PVD. The difficulty in visually confirming a PVD due to variations in the appearance of a PVD may account for the discrepancy.29 In our series, a PVD was not noted by lens-aided biomicroscopy on the preoperative examination in any of eyes, and this was confirmed intraoperatively.
The mechanism for an ERM development in eyes without a PVD has not been determined. A small congenital defect in the ILM was postulated to allow the entry of retinal pigment epithelial cells and retinal glial cells into the vitreous cavity.
One of the most common complications after vitrectomy is the development and progression of a cataract. We observed that the lens was transparent throughout the follow-up period in all of the eyes in our series. Our results are consistent with previous reports concerning vitrectomy in young patients.11, 14 The effect of the age of the patient and the use of intraocular gas in cataract progression after vitrectomy are well known. The rate of nuclear sclerotic cataracts in patients more than 50 years of age is approximately sixfold greater than in patients less than 50 years of age.30 Intravitreal gas bubbles are associated with the increase in nuclear sclerosis to approximately 60% compared with the eyes without the use of a gas bubble. The age of our young patients and the nonuse of a gas-tamponade postoperatively may account for the absence of cataract formation. In addition, the shorter follow-up in the present study may also be the cause of low rate of cataract because the rate of cataract formation has been shown to increase over time after vitrectomy.31 A longer follow-up is needed to determine whether cataracts develop after the vitrectomy surgery in young patients.
In conclusion, our results have shown that ERMs in young patients are different from those of adults by being thicker, more adherent to the retina, and still attached to the vitreous. Vitrectomy and removal of ERM with ILM peeling are effective and safe surgical procedures. Removal of the ILM may minimize the recurrence of an ERM.
References
Appiah AP, Hirose T, Kado M . A review of 324 cases of idiopathic premacular gliosis. Am J Ophthalmol 1988; 106: 533–535.
Pesin SR, Olk RJ, Grand MG, Boniuk I, Arribas NP, Thomas MA et al. Vitrectomy for premacular fibroplasias. Prognostic factors, long-term follow up, and time course of visual improvement. Ophthalmology 1991; 98: 1109–1114.
Margherio RR, Cox Jr MS, Trese MS, Murphy PL, Johnson J, Minor LA . Removal of epiretinal membrane. Ophthalmology 1985; 92: 1075–1083.
Grewing R, Mester U . Results of surgery for epiretinal membranes and their recurrences. Br J Ophthalmol 1996; 80: 323–326.
Sidd RJ, Fine SL, Owens SL, Patz A . Idiopathic preretinal gliosis. Am J Ophthalmol 1982; 94: 44.
Barr CC, Michels RG . Idiopathic nonvascularized epiretinal membranes in young patients: report of six cases. Ann Ophthalmol 1982; 14: 335–341.
Meyer CH, Rodrigues EB, Mennel S, Schmidt JC, Kroll P . Spontaneous separation of epiretinal membrane in young subjects: personal observations and review of the literature. Graefes Arch Clin Exp Ophthalmol 2004; 242: 977–985.
Mulligan TG, Daily MJ . Spontaneous peeling of an idiopathic epiretinal membrane in a young patient. Arch Ophthalmol 1992; 110: 1367–1368.
Desatnik H, Treister G, Moisseiev J . Spontaneous separation of an idiopathic macular pucker in a young girl. Am J Ophthalmol 1999; 127: 729–731.
Kimmel AS, Weingeist TA, Blodi CF . Idiopathic premacular gliosis in children and adolescents. Am J Ophthalmol 1989; 108: 578–581.
Banach MJ, Hassan TS, Cox MS, Margherio RR, Williams GA, Garretson BR et al. Clinical course and surgical treatment of macular epiretinal membranes in young subjects. Ophthalmology 2001; 108: 23–26.
Smiddy WE, Michels RG, Gilbert HD, Green WR . Clinicopathologic study of idiopathic macular pucker in children and young adults. Retina 1992; 12: 232–236.
Smiddy WE, Maguire AM, Green WR, Michels RG, de la Cruz Z, Enger C et al. Idiopathic epiretinal membranes. Ultrastructural characteristics and clinicopathologic correlation. Ophthalmology 1989; 96: 811–820.
Benhamou N, Massin P, Spolaore R, Paques M, Gaudric A . Surgical management of epiretinal membrane in young patients. Am J Ophthalmol 2002; 133: 358–364.
Kwok AK, Li WW, Pang CP, Lai TY, Yam GH, Chan NR et al. Indocyanine green staining and removal of internal limiting membrane in macular hole surgery: histology and outcome. Am J Ophthalmol 2001; 132: 178–183.
Brooks HL . Macular hole surgery with and without internal limiting membrane peeling. Ophthalmology 2000; 107: 1939–1948.
Park DW, Dugel PU, Garda J, Sipperley JO, Thach A, Sneed SR et al. Macular pucker removal with and without internal limiting membrane peeling: pilot study. Ophthalmology 2003; 110: 62–64.
Kwok AK, Lai TY, Yuen KS . Epiretinal membrane surgery with or without internal limiting membrane peeling. Clin Experiment Ophthalmol 2003; 31: 470–475.
Haritoglou C, Eibl K, Schaumberger M, Mueller AJ, Priglinger S, Alge C et al. Functional outcome after trypan blue-assisted vitrectomy for macular pucker: a prospective, randomized, comparative trial. Am J Ophthalmol 2004; 138: 1–5.
Bardak Y, Cekic O, Tig SU . Comparison of ICG-assisted ILM peeling and triamcinolone-assisted posterior vitreous removal in diffuse diabetic macular edema. Eye 2006; 20: 1357–1359.
Ikagawa H, Yoneda M, Iwaki M, Isogai Z, Tsujii K, Yamazaki R et al. Chemical toxicity of indocyanine green damages retinal pigment epithelium. Invest Ophthalmol Vis Sci 2005; 46: 2531–2539.
Cekic O, Morimoto T, Ohji M, Sawa M, Hasegawa T, Sakaguchi H et al. Nonaxoplasmic transfer of indocyanine green into the optic nerve after intravitreal application. Retina 2004; 24: 412–415.
Uemura A, Kanda S, Sakamoto Y, Kita H . Visual field defects after uneventful vitrectomy for epiretinal membrane with indocyanine green-assisted internal limiting membrane peeling. Am J Ophthalmol 2003; 136: 252–257.
Ando F, Yasui O, Hirose H, Ohba N . Optic nerve atrophy after vitrectomy with indocyanine green-assisted internal limiting membrane peeling in diffuse diabetic macular edema. Adverse effect of ICG-assisted ILM peeling. Graefes Arch Clin Exp Ophthalmol 2004; 242: 995–999.
Kusaka S, Oshita T, Ohji M, Tano Y . Reduction of the toxic effect of indocyanine green on retinal pigment epithelium during macular hole surgery. Retina 2003; 23: 733–734.
Kwok AK, Lai TY, Li WW, Yew DT, Wong VW . Trypan blue- and indocyanine green-assisted epiretinal membrane surgery: clinical and histopathological studies. Eye 2004; 18: 882–888.
Kishi S, Shimizu K . Oval defect in detached posterior hyaloid membrane in idiopathic preretinal macular fibrosis. Am J Ophthalmol 1994; 118: 451–456.
Heilskiov TW, Massicotte SJ, Folk JC . Epiretinal macular membranes in eyes with attached posterior cortical vitreous. Retina 1996; 16: 279–284.
Kakehashi A, Kado M, Akiba J, Hirokawa H . Variations of posterior vitreous detachment. Br J Ophthalmol 1997; 81: 527–532.
Thompson JT . The role of patient age and intraocular gas use in cataract progression after vitrectomy for macular holes and epiretinal membranes. Am J Ophthalmol 2004; 137: 250–257.
Cheng L, Azen SP, El-Bradey MH, Toyoguchi M, Chaidhawangul S, Rivero ME et al. Duration of vitrectomy and postoperative cataract in the vitrectomy for macular hole study. Am J Ophthalmol 2001; 132: 881–887.
Acknowledgements
This work was supported by a grant from the National Natural Science Foundation (No. 60671005), China.
Author information
Authors and Affiliations
Corresponding author
Additional information
Proprietary interests: none
Rights and permissions
About this article
Cite this article
Fang, X., Chen, Z., Weng, Y. et al. Surgical outcome after removal of idiopathic macular epiretinal membrane in young patients. Eye 22, 1430–1435 (2008). https://doi.org/10.1038/sj.eye.6702963
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702963
Keywords
This article is cited by
-
Clinical features of idiopathic epiretinal membrane in children and the factors influencing postoperative visual acuity
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Juvenile idiopathische epiretinale Membran
Der Ophthalmologe (2016)
-
Optical coherence tomographic characteristics and surgical outcome of eyes with myopic foveoschisis
Eye (2009)
-
Anatomical and visual outcome after vitrectomy with triamcinolone acedonide-assisted epiretinal membrane removal in highly myopic eyes with retinal detachment due to macular hole
Eye (2009)