Abstract
Purpose
The current vitreous substitutes such as silicone oil, heavy silicone oil, and polymeric gels that are directly injected into vitreous cavity frequently cause severe intraocular complications. There is a very urgent need to find a more suitable artificial vitreous substitute for pars plana vitrectomy (PPV) surgery.
Methods
We have devised a novel capsular artificial vitreous using tailor-made silicone rubber elastomer. The novel device was implanted into the vitreous cavity of rabbit after PPV and the eye was examined by ophthalmoscopy, fundus photography, and tonometry during an 8-week treatment period. B-scan ultrasonography, electroretinogram (ERG), and histological studies by light microscopy were also performed at the end of 8 weeks.
Results
The novel artificial vitreous body consists of a thin vitreous-like capsule with a silicone tube–valve system. The capsule can be folded and implanted into vitreous cavity through 1.5 mm incision on sclera. Physiological balanced solution (PBS) was then injected into the capsule and inflated to support retina and control intraocular pressure (IOP) through the tube–valve system subsequently fixed under the conjunctiva. Experiments using rabbits showed that the novel vitreous body could effectively support the retina and apparently induced no significant pathological changes in the eye over 8 weeks.
Conclusion
This approach may provide a new research strategy in the vitreous replacement technology. The novel artificial vitreous body device can effectively support retina, control IOP, and has good biocompatibility. It may be a good alternative to injecting artificial vitreous although its tamponade properties and usefulness still have to be proven in complex vitreoretinal diseases.
Similar content being viewed by others
Introduction
Pars plana vitrectomy (PPV) is one of the most important ophthalmic surgeries for treating a number of blinding diseases including diabetic retinopathy, retinal detachment, traumatic retinopathy, and age-related macular degeneration by removing and replacing the diseased vitreous body since the 1970s. Successful PPV surgery has enabled ophthalmologists to restore vision in a number of patients that would have previously been regarded as incurable.1, 2, 3
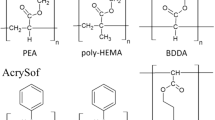
Clinically, a number of artificial vitreal materials are available, which include silicone oil, heavy silicone oil, and polymeric gels. However, these materials may lead to undesirable side effects and even severe complications. For example, silicone oil tamponade has 70% success rate of surgery according to anatomical integrity, but it is not without problems.4 Silicone oil may emulsify with time and must then be surgically removed, leading to an enhanced risk of retinal detachment. Further complications include cataract formation, glaucoma, and keratopathy.5, 6 Moreover, the relatively low density of silicone oil fails to support the inferior retina adequately and its refractive index leads to a high hyperopic shift and poor vision.7 Recently, heavy oil, a solution of perfluorohexyloctane and silicone oil as an internal tamponade, has been used in retinal detachment surgery, but its complications were emulsification and inflammatory reaction.8 A number of gel-form vitreous substitutes have been proposed, which included silicone gel, cross-linked polyvinyl alcohol (PVA), and cross-linked poly (1-vinyl-2-pyrrolidinone) (PVP). These materials are still in experimental stages and their long-term toxicity is unknown.9, 10, 11, 12
Current research on artificial vitreous body aims to find materials, which are transparent, injectable, and biocompatible in vivo. Therefore, these materials must be hydrophilic and able to form a gel within the vitreous cavity.13 However, such directly injected materials have so far been proven to be less than safe and practical as a vitreous body substitute. The current vitreous substitutes such as silicone oil that are directly injected into eyes frequently cause intraocular toxicity, and they are difficult to be removed completely. Ideally, the key properties of good biomaterials must firstly be safe, and secondly, easy to remove if need be. There is a very urgent need to find a more suitable artificial vitreous substitute for PPV surgery. In this study, we proposed a new strategy to replace the natural vitreous by a novel capsular artificial vitreous body with a pressure-control valve. It was designed to avoid those disadvantages mentioned above, and we have validated its feasibility and biocompatibility in the rabbit eye.
Methods
Cytotoxicity tests of the vitreous capsule material
The basic material belongs to tailor-made modified silicone rubber elastomer.14 It is a transparent macromolecule cross-linking polymer of polyvinylsiloxane and polyhydrosiloxane with good mechanical properties and biocompatibility. This test was performed by direct contact of silicone rubber elastomer with cultured fibroblast cells as described earlier.15, 16 Mouse fibroblast L929 cell lines were cultured in Dulbecco modified Eagle's medium (DMEM; GIBCO, Grand Island, Ny, USA), with 10% fetal calf serum, penicillin/streptomycin (100/100 U), and gentamycin (100 μg/ml), and incubated in 5% CO2 at 37°C for 24 h. Then, cell cultures were incubated with samples or negative (DMEM) and positive controls (0.1% phenol solution) at the same conditions for 24 h. The viability and cell metabolic activity were tested by the MTT assays. At least three replicates were performed for this test.
Novel capsular artificial vitreous body fabrication
The mould of the vitreous capsule was made equally based on rabbit's vitreous body physiological parameters as shown in Figure 1a. To produce a very thin capsule, the mould of capsule was dipped into the liquid silicone rubber material slowly and repeatedly, then it was put into the oven to vulcanize the silicone rubber. The 0.01-mm-thick capsule could be gently peeled off from the mould and its natural shape is similar to rabbit's vitreous body. Finally, the capsule was attached to a 1-mm-diameter silicone tube with a pressure-adjustable valve.
The rabbit artificial vitreous body consists of vitreous-shape capsule, tube, and valve. The intra-capsule pressure can be adjusted from the valve with a syringe. There is a slice of anti-penetrating metal in the valve. (a) Rabbit artificial vitreous body design (central depth of patellar fossa: 2.5 mm). (b–e) Illustration of pars plana vitrectomy (PPV) process using the novel artificial vitreous body implant. (f) Artificial vitreous body sample without physiological balanced solution (PBS). (g and h) Artificial vitreous body full of PBS viewing from the front and the back, respectively.
PPV surgery and artificial vitreous body implant
The novel artificial vitreous bodies were implanted into rabbit eyes using the PPV procedure to evaluate its practicality and ocular toxicity. All experimental procedures adhered to the Association for Research in Vision and Ophthalmology Resolution on the Use of Animals in Ophthalmic and Vision Research.
Before all surgical procedures, 20 New Zealand albino rabbits weighing 2 to 2.5 kg were anesthetized by an intramuscular injection of ketamine hydrochloride (30 mg/kg) and chlorpromazine hydrochloride (15 mg/kg). Pupils were dilated with 0.5% tropicamide (Mydrin P; Santen, Osaka, Japan) and phenylephrine (2.5%). Rabbits were equally divided into two groups: PPV with artificial vitreous body implantation and PPV alone with balanced salt solution (BSS; Shike, Shenyang, China). Standard three-port PPV, with sclerotomies 2.5-mm posterior to the limbus, was performed on the right eye of each rabbit using the Geuder vitrectomy machine (Germany).17 The left eyes did not undergo surgery and served as contralateral controls. After the vitrectomy, the artificial vitreous body was folded and implanted into the vitreous cavity after fluid–air exchange was completed (Figure 2). About 0.5 ml of physiological balanced solution (PBS) was then injected into capsule and inflated to support retina through a silicone tube–valve system subsequently fixed under the conjunctiva (Figures 1 b–e). The pressure of the capsule can be adjusted via the silicone tube–valve system by injecting or withdrawing fluid. The sclerotomies were closed with 10–0 Vicryl sutures.
The operation was concluded by subconjunctival injection of gentamycin and dexamethasone, and by application of compound tobramycin and atropine (1%) ointment.
Follow-up clinic examinations
The operated eyes were examined and assessed including corneal, lens opacities, and the fundus on days 1, 3, and 7, and weekly after surgery for 8 weeks with slit-lamp biomicroscopy and indirect ophthalmoscopy. The intraocular pressures (IOPs) were measured by Goldmann tonometry preoperatively at 3, 7, 14, 28 days, and 8 weeks postoperatively. B-scan ultrasonography (CineScan, BVI Inc., Chermont-ferrand, France; 10 MHz probe) was also performed to determine the positioning and flexibility of the artificial vitreous body at the end of the 8-week observation period.18
Electroretinography
Electroretinograms were obtained in rabbits at 8 weeks with a full-field dome method similar to clinical electroretinography (ERG)19 methods specified by the International Society for Clinical Electrophysiology of Vision (ISCEV) standard.20 The eyes were dilated with 0.5% tropicamide and dark-adapted for at least 30 min. Rabbits were anesthetized with a saline solution containing ketamine hydrochloride (30 mg/kg) and chlorpromazine hydrochloride (15 mg/kg). Corneal contact len electrodes were used with a reference electrode placed on the forehead, an ear-clip electrode as a ground connection. The recordings were performed using the Roland Ganzfeld system and PC-based signal acquisition and analysis software (Fa. Roland Consult, Brandeburg, Germany). The bright flash response was elicited using the ISCEV standard flash of 2.4 cds/m2. After light adaptation of 10 min with a steady background illumination of 10 cd/m2 photopic responses, the 30-Hz flicker ERG were recorded. The a- and b-wave amplitudes and the implicit times of the standard responses were determined.
Histology and light microscopy
Light microscopy was performed to evaluate the ocular response to the novel artificial vitreous body.21 Four rabbits in two groups at 8 weeks were killed and enucleated, and the eyes were immediately fixed in 4% neutral paraformaldehyde solution. After examination of the gross pathology, eyes were processed for routine paraffin embedding. Ten consecutive 6-mm-thick sections of each sample were made and stained with haematoxylin–eosin.
Statistical analysis
Data were reported as mean±SD. Group differences were statistically examined using one-way analysis of variance (ANOVA) with Tukey's honestly significant difference (HSD) post hoc test. Statistical significance was considered at a probability P<0.05.
Results
Cytotoxicity tests
The in vitro cytotoxicity of artificial vitreous material tests were carried on using the L929 mouse fibroblasts cell line. No changes in cell morphology, detachment, and membrane lysis were observed in culture with the tested materials and negative control. Apart from the expected difference between positive and negative controls, the absorbance values obtained from material extracts did not show a significant difference of the material extracts vs negative control (P>0.05). The extracts induced neither cell viability reduction nor inhibition of cell growth, resulting in no toxic effects.
The novel artificial vitreous body
The artificial vitreous body consists of a thin vitreous-like capsule with a tube–valve system to control IOP (Figures 1 f–h). The natural shape of vitreous capsule is similar to that of rabbit's vitreous so that the lens can rest on the patellar fossa when the capsule was filled with PBS. The 0.01-mm-thick capsule was thin and it has good flexibility in the vitreous cavity. The intracapsule pressure can be adjusted through the valve with a syringe.
Clinical examinations
In the two groups, there was slight conjunctival hyperaemia by day 7 after surgery. With the exception of cataract in two rabbits, no serious complications including corneal opacity, intraocular inflammation, and retinal haemorrhage or detachment, were observed over 8 weeks (Figure 3a). Compared with contralateral controls, the tonometric measurements showed no significant difference of IOP between the two groups (Figure 3b, P>0.05).
Clinic imaging studies for rabbit eyes after the novel artificial vitreous implantation. Anterior ocular segment and ocular fundus findings (a) of a rabbit eye showing neither corneal opacity, intraocular inflammation, or lens opacity nor vitreous opacity, retinal haemorrhage, or retinal detachment at the end of 8 weeks. (b) Changes of intraocular pressure (IOP) after artificial vitreous body implant during an 8-week observation period. No elevation of IOP was observed and there was no difference between the operated and contralateral control eyes (P>0.05). Each point shows mean±SD. (c and d) Axial B-scan ultrasonography showing control eye (c) and a capsule-like reflective signal within the vitreous cavity (d).
On B-scan ultrasonography, scattered and slightly reflective signals of capsule-like membrane were observed within the vitreous cavity as shown in Figure 3d. The capsule of novel vitreous with PBS was apparently in good contact with the inner retina and can support it well.
Electroretinograms
Compared with the preoperative values, the ERG recordings from both the experimental and control eyes (n=6) showed similar trend of decrease in the b-wave amplitudes after 8 weeks of treatment. However, there were no significant differences between the experimental and control eyes in terms of a- or b-wave amplitudes, or latency (P>0.05).
Histological findings
Gross examination of eye specimens showed the capsule of novel vitreous could evenly fill the vitreous cavity and support the retina effectively (Figure 4a). Histological studies of the retina showed good tissue integrity with no structural abnormality such as deformations, degeneration, or inflammation in the operated eyes in the two groups (Figures 4b and c). There were also no structural damages in other parts of the eye including the cornea and ciliary body.
Effects of the novel artificial vitreous body implant on the rabbit eyes at the end of 8-week treatment. (a) The capsule of novel vitreous can evenly fill the vitreous cavity and support the retina after being fixed in 4% neutral paraformaldehyde solution. (b and c), Histological sections (HE) showed no abnormality of the retina in the implantation eye (b) when compared to the control eye (c).
Discussion
In spite of much effort to replace the vitreous body of the eye, an ideal solution for permanent replacement of the vitreous body is yet to be found. The materials currently used as vitreous substitutes can only provide temporary relief, and the search for a better and more permanent vitreous substitute is still ongoing. Therefore, current research on artificial vitreous body focuses on finding a directly injectable material that has good biocompatibility.13, 22 However, severe ocular complications were observed which resulted from a direct contact of these injectable materials with the retina, ciliary body, and lens. Adding to the these problems, the concern of intraocular toxicity, inherent disorder of the fluid, and its difficulty to be completely removed have been inhibitory to the further development of these directly injectable materials in PPV surgery.
In this project, we have proposed a nontraditional strategy and devised a novel capsular artificial vitreous with pressure-control valve to replace the natural vitreous. PBS was then injected into the capsule through the valve and the pressure of capsule was adjusted accordingly. The design of valve resembles the glaucoma valves that function to adjust the IOP,23 since high IOP often occurs after PPV surgery. This novel pressure-control device may help to maintain a safe intraocular pressure.
The natural vitreous body is a transparent gel made up of approximately 98% of water with trace amount of collagen and it is surrounded by a very thin vitreous membrane. By analogy, the artificial vitreous body may be enclosed by a thin membrane. Our current device contains a membrane pocket and may be a good alternative of artificial vitreous substitute.
Intraocular balloons have been tried in the 1980s. The idea of the balloon was to prevent the silicone oil from leaking into the retina during surgery and to withdraw by puncturing the balloon after surgery.24 It acted as a tool to inject silicone oil during PPV surgery. However, this procedure has yet to gain popularity in ophthalmic surgery. This approach was very different from our proposed artificial vitreous body, which aims to provide a long-term intraocular implant.
It is interesting to note that in the early development of breast implants in plastic surgery, similar to the current clinical vitreous substitute, directly injectable materials were used. In fact, the hydrophilic polyacrylamide gel (PAAG) was directly injected into the breast, and this procedure was practiced widely in China and Eastern Europe in the 1990s.25, 26 Such procedure in breast implants was analogous to the use of silicone oil to replace the vitreous. It was gradually realized that the injected PAAG induced severe complications including inflammation and infection, multiple indurations, haematoma, painful masses, and mastalagia.25, 26 Nowadays, direct injection of PAAG has been forbidden and replaced by capsule-like implants where the fluid substitute is contained in a thin elastic capsule.27, 28, 29 This approach of implant has shown good clinical success. In case of complications, the implant can be removed completely without leaving behind residual fluid substitute. Apparently, the development of artificial vitreous and breast substitute shared a similar path and both have suffered setbacks from injecting fluid substitute directly into the organ. Therefore, similar lesson may be learnt and the use of a capsule-type implant may be a good replacement of the vitreous.
Clearly, it is crucial to select the suitable material for manufacturing the capsule. Ideally the material should be nontoxic and inert, thin and transparent, with good water and oxygen permeability, high compatibility, and good elasticity. These are the important properties of the capsule for a long-term vitreous body replacement. Newly modified silicone rubber elastomers are available which has been promising for breast implant.28, 30 In a similar way, the elastomer material of the capsule was tailor-made for vitreous implant, and it has shown good oxygen permeability, good mechanical and optical properties (Shore A hardness: 37.4°, tensile intensity: >5.86 MPa, elongation ratio: >1200%, tear intensity: 34 kN/m, transmittances: >93%, and Hazes: <1%), and good biocompatibility (such as skin irritation test, sensitization tests, febrile responses, acute systemic toxicity test, subcutaneous implantation test, and haemolysis test) according to the International Organization for Standardization (ISO) guidelines (data not shown).
The novel vitreous system has a number of advantages: (1) it is safe and easy to implant through a 1.5 mm scleral incision; (2) it is removable; (3) it can support the retina by slightly inflating (Figure 4a); and (4) it can modulate the IOP through the tube–valve system.
Although further improvements can be made on the manufacturing of the device (such as improving and miniaturizing the whole artificial vitreous system, further enhancing the hydrophilic property, and biocompatibility of the materials), the present study proposed a new paradigm for artificial vitreous replacement that do not have the disadvantages of current directly injected vitreous substitutes. Although the material apparently induced no obvious ocular damages in the 8-week treatment period according to cytotoxicity tests, ERG, and histological studies, long-term safety for intraocular implantation should be further evaluated. Further studies are in progress to ascertain its biocompatibility during a longer time observation and compare its toxicity, feasibility, and effectiveness with current artificial vitreous substitutes in mammalian animal eyes. Because our study is a novel idea, many questions will remain in this article and need to be resolved in the future.
In conclusion, this approach may provide a new research strategy in the vitreous replacement technology. The novel artificial vitreous body device can effectively support retina, control IOP, and has good biocompatibility. It may be a good alternative to injecting artificial vitreous although its tamponade properties and usefulness have to be proven in complex vitreoretinal diseases.
References
Lakhanpal V, Schocket SS, Elman MJ, Dogra MR . Intraoperative massive suprachoroidal hemorrhage during pars plana vitrectomy. Ophthalmology 1990; 97 (9): 1114–1119.
Recchia FM, Ruby AJ, Carvalho Recchia CA . Pars plana vitrectomy with removal of the internal limiting membrane in the treatment of persistent diabetic macular edema. Am J Ophthalmol 2005; 139 (3): 447–454.
Tanner V, Minihan M, Williamson TH . Management of inferior retinal breaks during pars plana vitrectomy for retinal detachment. Br J Ophthalmol 2001; 85 (4): 480–482.
Azen SP, Scott IU, Flynn Jr HW, Lai MY, Topping TM, Benati L et al. Silicone oil in the repair of complex retinal detachments. A prospective observational multicenter study. Ophthalmology 1998; 105 (9): 1587–1597.
Scott IU, Flynn Jr HW, Murray TG, Smiddy WE, Davis JL, Feuer WJ . Outcomes of complex retinal detachment repair using 1000- vs 5000-centistoke silicone oil. Arch Ophthalmol 2005; 123 (4): 473–478.
The Silicone Study Group. Vitrectomy with silicone oil or sulfur hexafluoride gas in eyes with severe proliferative vitreoretinopathy: results of a randomized clinical trial. Silicone Study Report 1. Arch Ophthalmol 1992; 110 (6): 770–779.
Stefansson E, Anderson Jr MM, Landers III MB, Tiedeman JS, McCuen II BW . Refractive changes from use of silicone oil in vitreous surgery. Retina 1988; 8 (1): 20–23.
Bhisitkul RB, Gonzalez VH . ‘Heavy oil’ for intraocular tamponade in retinal detachment surgery. Br J Ophthalmol 2005; 89 (6): 649–650.
Chirila TV, Tahija S, Hong Y, ijayasekaran S, Constable IJ . Synthetic polymers as materials for artificial vitreous body: review and recent advances. J Biomater Appl 1994; 9 (2): 121–137.
Hong Y, Chirila TV, Fitton JH, Ziegelaar BW, Constable IJ . Effects of crosslinked poly (1-vinyl-2-pyrrolidinone) gels on cell growth in static cell cultures. Biomed Mater Eng 1997; 7 (1): 35–47.
Hong Y, Chirila TV, Vijayasekaran S, Shen W, Lou X, Dalton PD . Biodegradation in vitro and retention in the rabbit eye of crosslinked poly (1-vinyl-2-pyrrolidinone) hydrogel as a vitreous substitute. J Biomed Mater Res 1998; 39 (4): 650–659.
Maruoka S, Matsuura T, Kawasaki K, Okamoto M, Yoshiaki H, Kodama M et al. Biocompatibility of polyvinylalcohol gel as a vitreous substitute. Curr Eye Res 2006; 31 (7–8): 599–606.
Colthurst MJ, Williams RL, Hiscott PS, Grierson I . Biomaterials used in the posterior segment of the eye. Biomaterials 2000; 21 (7): 649–665.
Mou SS, Tu M, Tang SQ, Zhou CR . Improvement of blood compatibility of silicone rubber by the addition of hydroxyapatite. J Mater Sci Lett 2003; 22: 343–344.
Fini M, Cigada A, Rondelli G, Chiesa R, Giardino R, Giavaresi G et al. In vitro and in vivo behaviour of Ca- and P-enriched anodized titanium. Biomaterials 1999; 20 (17): 1587–1594.
Ramires PA, Miccoli MA, Panzarini E, Dini L, Protopapa C . In vitro and in vivo biocompatibility evaluation of a polyalkylimide hydrogel for soft tissue augmentation. J Biomed Mater Res Part B: Appl Biomater 2005; 72 (2): 230–238.
Chin HS, Park TS, Moon YS, Oh JH . Difference in clearance of intravitreal triamcinolone acetonide between vitrectomized and nonvitrectomized eyes. Retina 2005; 25 (5): 556–560.
Oliveira LB, Meyer CH, Kumar J, Tatebayashi M, Toth CA, Wong F et al. RGD peptide-assisted vitrectomy to facilitate induction of a posterior vitreous detachment: a new principle in pharmacological vitreolysis. Curr Eye Res 2002; 25 (6): 333–340.
Kjellstrom U, Kjellstrom S, Bruun A, Andreasson S, Ponjavic V . Retinal function in rabbits does not improve 4–5 months after terminating treatment with vigabatrin. Doc Ophthalmol 2006; 112 (1): 35–41.
Marmor MF, Holder GE, Seeliger MW, Yamamoto S . International Society for Clinical Electrophysiology of Vision. Standard for clinical electroretinography (2004 update). Doc Ophthalmol 2004; 108 (2): 107–114.
Tahara YR, Sakamoto TR, Oshima YR, Ishibashi TR, Inomata HR, Murata TR et al. The antidepressant hypericin inhibits progression of experimental proliferative vitreoretinopathy. Curr Eye Res 1999; 19 (4): 323–329.
Soman N, Banerjee R . Artificial vitreous replacements. Biomed Mater Eng 2003; 13 (1): 59–74.
Nouri-Mahdavi K, Caprioli J . Evaluation of the hypertensive phase after insertion of the Ahmed Glaucoma Valve. Am J Ophthalmol 2003; 136 (6): 1001–1008.
Gnad H, Paroussis P, Skorpik C . An intraocular balloon for silicone oil implantation. Graefe's Arch Clin Exp Ophthalmol 1986; 224 (1): 18–20.
Cheng NX, Wang YL, Wang JH, Zhang XM, Zhong H . Complications of breast augmentation with injected hydrophilic polyacrylamide gel. Aesth Plast Surg 2002; 26 (5): 375–382.
Qiao Q, Wang X, Sun J, Zhao R, Liu Z, Wang Y et al. Management for postoperative complications of breast augmentation by injected polyacrylamide hydrogel. Aesth Plast Surg 2005; 29 (3): 156–162.
Benediktsson K, Perbeck L . Capsular contracture around saline-filled and textured subcutaneously-placed implants in irradiated and non-irradiated breast cancer patients: five years of monitoring of a prospective trial. J Plast Reconstr Aesthet Surg 2006; 59 (1): 27–34.
Bingham HG, Copeland EM, Hackett R, Caffee HH . Breast cancer in a patient with silicone breast implants after 13 years. Ann Plast Surg 1988; 20 (3): 236–237.
Glatt BS, Afifi G, Noone RB . Long-term follow-up of a sponge breast implant and review of the literature. Ann Plast Surg 1999; 42 (2): 196–201.
Brown MH, Shenker R, Silver SA . Cohesive silicone gel breast implants in aesthetic and reconstructive breast surgery. Plast Reconstr Surg 2005; 116 (3): 768–781.
Acknowledgements
This study was supported by the Science and Technology Foundation of Guang Dong Province of China (2003C32715, 06104574) and the Science and Technology Foundation of Guang Zhou City of China (2006Z2-E0141).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Gao, Q., Mou, S., Ge, J. et al. A new strategy to replace the natural vitreous by a novel capsular artificial vitreous body with pressure-control valve. Eye 22, 461–468 (2008). https://doi.org/10.1038/sj.eye.6702875
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702875
Keywords
This article is cited by
-
A pilot clinical study of complex rhegmatogenous retinal detachment treatment via foldable capsular buckle scleral buckling
BMC Ophthalmology (2023)
-
Foldable capsular vitreous body indications, complications, and outcomes: a systematic review
Graefe's Archive for Clinical and Experimental Ophthalmology (2023)
-
Clinical Efficacy and Safety of Foldable Capsular Vitreous Body Implant Surgery in 22 Cases of Silicone Oil-dependent Eyes
Current Medical Science (2023)
-
Study on the efficacy and safety of foldable capsular vitreous body in the severe retinal detachment eyes
BMC Ophthalmology (2022)
-
Comparison of Viscoelastic Substance Injection Versus Air Filling in the Anterior Chamber During Foldable Capsular Vitreous Body (FCVB) Implant Surgery: A Prospective Randomized Controlled Trial
Advances in Therapy (2021)