Abstract
Purpose
To test whether Heidelberg Retina Tomograph (HRT) is applicable to assess the optic nerve head (ONH) configuration of the atrophic phase of non-glaucomatous optic neuropathy when a default set of the reference plane is used.
Methods
Ten eyes with non-arteritic anterior ischaemic optic neuropathy (NAION), 17 eyes with Leber's hereditary optic neuropathy (LHON), 40 eyes with compressive optic neuropathy (CON) owing to chiasmal tumour, and 241 eyes of control individuals were examined with HRT using the default reference plane. The global values of HRT parameters were evaluated among the groups of patients and controls. The sectoral measurements of the eyes with LHON and CON were compared with controls. To eliminate the influence of disc size and age on HRT measurements, eyes with disc area- and age-matched normal controls were used for comparison with eyes with NAION and LHON.
Results
Cup parameters in eyes with NAION were similar to those in controls. The retinal nerve fibre layer (RNFL) thickness was significantly thinner in eyes with NAION than that of controls. The eyes with LHON had significantly larger cup parameters, smaller rim volume, and thinner mean RNFL thickness than controls. Eyes with CON had significantly larger rim area and smaller cup parameters but similar RNFL thickness compared with controls.
Conclusions
When the default reference plane is used, HRT can measure the ONH configuration in eyes with NAION and LHON as expected. However, caution must be made to interpret the parameters obtained from the eyes with CON.
Similar content being viewed by others
Introduction
Heidelberg Retina Tomograph (HRT) is a confocal scanning laser ophthalmoscope, which allows a three-dimensional topographic analysis of the optic nerve head (ONH), and has been widely exploited to quantitatively evaluate the morphological changes of the ONH in glaucoma. Its accuracy and reproducibility in measuring the ONH have been discussed essentially in the cases of glaucoma,1, 2, 3, 4 but not for the other optic neuropathies.
The purpose of this study is to test whether HRT with a default set of the reference plane is also applicable to non-glaucomatous optic neuropathies such as ischaemic, hereditary, and compressive optic neuropathy (CON).
Materials and methods
Enrolled were 67 eyes of 43 patients with optic neuropathy of various aetiologies, who regularly visited the Neuro-ophthalmology clinic in Kobe University Hospital between June 2003 and December 2005, which comprised 10 eyes of 10 patients with non-arteritic anterior ischaemic optic neuropathy (NAION), 17 eyes of nine patients with Leber's hereditary optic neuropathy (LHON) with a mitochondrial DNA mutation at nucleotide position 11 778, and 40 eyes of 24 patients with CON owing to chiasmal tumour. Six eyes with NAION had superior altitudinal hemianopia and four eyes had inferior altitudinal hemianopia. In those with CON, 16 patients had pituitary adenoma, two had craniopharyngioma, three had suprasellar meningioma, and three had Rathke's cleft cyst, all of which exhibited band atrophy of optic disc. Only the eyes with temporal hemianopia detected on Goldmann perimetry with I-1-e or stronger stimuli were eligible. All eyes were at the chronic stage of the diseases, that is; duration from the onset of disease to the entry of the current study was at least 6 months and, thus, they ophthalmoscopically exhibited optic atrophy in the affected eyes at the entry of this study. In addition to the above patients, 241 eyes of 241 individuals consisted of volunteers from the staff of the Kobe University Hospital and patients with minor refractive errors were also enrolled as control. Because distribution of age and disc size in the patients with NAION and LHON was different from whole controls, disc area- and age-matched normal controls were also separately constructed. Exclusion criteria were: myopia more than −6 dioptres (D), astigmatism more than 3D, intraocular pressure measurements over 21 mmHg, optic disc abnormality such as tilted disc, and any other posterior segment ocular pathologic factors.
All investigations were conducted in accordance with the ethical standards stated in the 1964 Declaration of Helsinki and with the approval of the Institutional Review Board of the Kobe University Graduate School of Medicine. Written informed consent was obtained from each participant. All the participants underwent imaging analyses with HRT (software version 3.04, Heidelberg Engineering GmbH, Heidelberg, Germany) essentially according to the technique described previously.1, 2, 3, 4, 5, 6 In brief, for each HRT imaging session three 15 × 15 degree images were obtained for each eye by one of the authors (ANK). After generating a mean topographic image, disc margin was delineated as a contour line by the same observer referring to an optic disc photograph. When mean topographies had a SD exceeding 30 μm, they were excluded. The reference plane was automatically set at the standard value of 50 μm below the contour line at the temporal sector of the disc margin between 350° and 356°. A variety of topographic parameters automatically calculated were used for global and sectoral analyses of the ONH. The correlations between age and each HRT parameter and between disc area and the remainders of HRT measurements were analysed in normal eyes.
For the global analysis, the following topographic parameters were evaluated among the groups of patients with optic neuropathies and normal subjects; disc area, cup area, rim area, cup/disc (C/D) area ratio, cup volume, rim volume, mean cup depth, maximum cup depth, mean retinal nerve fibre layer (RNFL) thickness, RNFL cross sectional area, height variation contour (HVC), and cup shape measure. For the sectoral analysis in eyes with LHON and CON, cup area, rim area, C/D area ratio, cup volume, rim volume, mean cup depth, mean RNFL thickness were compared with those of normal controls. The sectoral analysis was not conducted in eyes with NAION because of a small sample size. The measurements of disc area- and age-matched old, disc area- and age-matched young, and whole normal controls were used for comparisons with NAION, LHON, and CON eyes, respectively.
Statistical analysis
All calculations were performed using StatView Software version 5.0 (SAS Institute Inc.). The Pearson correlation test was used in assessing the correlation between age and each HRT parameter and between disc area and the remainders. ANOVA with Bonferroni/Dunn test was used to compare the characteristics of the subjects and global measurement of the disc area among the groups of patients and whole normal subjects. Mann–Whitney U-test was used for the global and sectoral ONH analysis. P<0.05 was judged significantly different.
Results
The descriptive data of the participants are summarized in Table 1. The patients with NAION were significantly older than whole normal controls (P<0.001), whereas the patients with LHON were significantly younger (P<0.001). There was no significant difference in age between the patients with NAION and disc area- and age-matched old controls and between the patients with LHON and disc area- and age-matched young controls (P=0.10, P=0.73, respectively). There is a significant difference in the refractive error between the patients with LHON and disc area- and age-matched young normal subjects (P=0.010).
The correlations between age and each HRT parameter and between disc area and the remainders in normal eyes are displayed in Table 2. There were significantly negative associations between age and the rim area, rim volume, HVC, mean RNFL thickness, and RNFL cross-sectional area. In contrast, the disc area had a significant correlation with all the parameters except for the HVC.
Table 3 summarizes the results of the global HRT parameter measurements. The disc area of the NAION eyes was significantly smaller than that of whole normal controls (P<0.01). Eyes with NAION had significantly thinner mean RNFL thickness and smaller RNFL cross-sectional area than disc area- and age-matched controls (P<0.05 in both). There was no significant difference in the other parameters.
In the eyes with LHON, the disc area tended to be larger than that of whole controls, although there was no statistical significance (P=0.12). The cup area and C/D area ratio were significantly larger and the rim area, rim volume, and HVC were significantly smaller in eyes with LHON compared with disc area- and age-matched controls (P<0.05, P<0.05, P<0.05, P<0.001, and P<0.001, respectively). There was no significant difference in the mean cup depth and maximum cup depth between the LHON eyes and controls. The LHON eyes had significantly thinner mean RNFL thickness and smaller RNFL cross-sectional area as compared with disc area- and age-matched controls (P<0.001 in both). The eyes with CON had significantly smaller cup volume than whole normal eyes (P<0.05). The mean and maximum cup depths were significantly shallower in the CON eyes (P<0.01 and P<0.001, respectively).
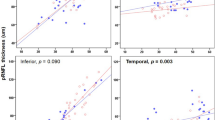
To investigate regional differences of disc morphology owing to LHON, sectoral measurements of the HRT parameters of eyes with LHON were compared with those of disc area- and age-matched controls (Table 4). The C/D area ratio, cup area, and cup volume of eyes with LHON were significantly larger than those of the normal eyes in the temporal, temporal superior, and temporal inferior sectors, while those of two groups were similar in the nasal, nasal superior, and nasal inferior sectors. Although the rim area in the LHON eyes was significantly smaller than controls only in the temporal, temporal superior, and temporal inferior segments, the rim volume was significantly smaller in all the sectors. The LHON eyes and controls had similar mean cup depth in all the segments. The mean RNFL thickness was significantly thinner in the eyes with LHON in all the sectors.
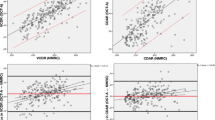
Sectoral analysis was also conducted in eyes with CON (Table 5). There was no significant difference in the cup area and RNFL thickness of all the segments between the CON eyes and controls. The rim area and rim volume in the temporal superior and temporal inferior sectors were significantly larger in the CON eyes than in the controls. The C/D area ratio in the temporal inferior sector and cup volume in the temporal, temporal superior, and temporal inferior sectors of the CON eyes was significantly smaller than those of normal eyes. The mean cup depth was significantly shallower in the CON eyes in the temporal, temporal superior, and temporal inferior sectors.
Discussion
The ONH assessment for three types of optic neuropathy with HRT in the present study demonstrated the following findings: (1) eyes with NAION had similar cup parameters to disc area- and age-matched controls, (2) some of the cup parameters were significantly larger in those with LHON than in controls as reported previously; (3) the cup parameters in eyes with CON were unexpectedly smaller, not larger, compared with controls; and (4) the RNFL parameters were reduced in eyes with NAION and LHON, but not in those with CON, compared with disc area- and age-matched controls.
It is widely known that an anatomically small optic nerve lacking physiological cup, so-called crowded disc, predispose patients to NAION.7, 8, 9, 10, 11, 12 Although most of the previous papers claimed that cupping did not develop in the patients with NAION unlike those with arteritic AION,9, 11, 13 this may be due to the underestimation of cupping in small discs with NAION. To overcome this issue, comparisons with disc area- and age-matched controls were made. As a result, the cup parameters were not different between the two groups, indicating that acquired excavation did not take place in the eyes with NAION. These findings were inconsistent with a previous study by Rath et al,14 where the C/D ratio was 1.1- to 1.2-fold larger in NAION discs compared with uninvolved fellow discs under the slit-lamp examination with a +90 D non-contact lens. However, the subjective assessment of the ONH by funduscopy does not readily distinguish the border of cupping from pale rim of the atrophic disc, which may have possibly led to the marginal overestimation of the cupping in their study. Recently, Danesh-Meyer et al15 evaluated the ONH configuration of involved eyes and normal fellow eyes in patients with unilateral NAION using HRT (version 1.01). They found that the mean value of C/D area ratio of the involved eyes and fellow eyes were 0.17±0.16 and 0.12±0.14, respectively, with a marginal, but significant difference. The reason of the discrepancy between their and our studies seems that the degree of the excavation after NAION in the small disc is too small, if any, for the HRT imaging procedure to consistently detect. Further accumulation of cases is needed to confirm whether NAION develops optic disc excavation or not.
A histological study demonstrated that RNFL thickness was decreased in eyes with NAION three decades ago.16 However, there was no study quantifying RNFL thinning in NAION until quite recently. Danesh-Meyer et al17 showed RNFL loss and structure–function correlation in NAION using scanning laser polarimetry (SLP). Others disclosed that RNFL thickness was reduced not only in the hemiretina corresponding to the altitudinal hemianopia but also in the sector corresponding to the relatively unaffected visual field in NAION using optical coherence tomography (OCT) and SLP.18 In the current study, HRT also detected RNFL thinning in eyes with NAION. Further studies with a larger sample size are necessary to investigate the sectoral alteration of RNFL thickness in eyes with NAION using HRT.
Regarding LHON, previous investigators reported that optic disc excavation also occurred in the atrophic stage of LHON.19, 20, 21, 22, 23, 24, 25 Ortiz et al21 studied the optic disc appearance of seven patients with LHON with stereoscopic fundus photography. They described that all the patients showed increased disc cupping with C/D ratios of 0.7–0.9 and that six of them displayed the shallow cupping. Mashima et al20 evaluated the ONH morphology of LHON, normal-tension glaucoma (NTG), and normal eyes using HRT (version 2.01). They reported that the LHON eyes also showed enlarged optic disc cupping but mean and maximum cup depth of LHON eyes were significantly shallower than those of NTG and similar to those of normal eyes. In the current study, the mean and maximum cup depth in LHON were similar to those of control eyes while other parameters showed significant difference. On the other hand, loss of retinal ganglion cells and RNFL has been demonstrated in LHON.26, 27, 28, 29, 30 Barboni et al26 showed severely decreased RNFL thickness in the temporal, superior, and inferior quadrants with a relative sparing in the nasal quadrant using OCT in the atrophic phase of LHON. According to their study, the reduction rate of RNFL thickness in the temporal quadrant was about 40%. In the current study, the average reduction rate of the mean RNFL thickness was 28% (0.18±0.04 mm in LHON vs 0.25±0.07 mm in disc area- and age-matched controls). The sectoral analyses disclosed that the mean RNFL thickness as well as the rim volume was significantly reduced in all the sectors. Nevertheless, the C/D area ratio, cup area, and cup volume were enlarged only in the temporal three sectors, but not in the nasal three in the eyes with LHON. Such an asymmetric enlargement of the optic excavation despite the diffuse thinning of the RNFL may reflect the spatial characteristics, with which the temporal side of the optic disc is more prone to be excavated. Alternatively, as pointed out by Barboni et al,26 the temporal RNFL was more severely damaged and lost than the nasal in eyes with LHON, but HRT could not accurately measure reduction of the RNFL thickness for yet undefined reasons.
The global parameters of HRT showed that the optic disc with CON had significantly smaller and shallower cup than normal subjects. These results are quite contrary to several previous reports showing the optic disc excavation in eyes with CON.24, 31, 32, 33, 34, 35 The descending optic atrophy leading to axonal loss and secondary collapse of glial tissue, which presumably resulted in enlarged disc cupping, was reported in a case with CON caused by an intracranial aneurysm.35 An additional contradictory finding in this study regarding the HRT parameters was that the RNFL was not reduced in the CON eyes. All the patients with CON due to the chiasmal tumours included in the current study had temporal hemianopia and band atrophy of disc, which is characterized by the temporal and nasal pallor with sparing of the superior and inferior quadrants of the disc, owing to the retrograde axonal degeneration of the retinal ganglion cells located nasal to the fovea. We have recently reported on the assessment of RNFL thickness in 34 patients with band atrophy using OCT.36 Although RNFL thickness was significantly decreased in all quadrants of the peripapillary areas, the reduction was predominant in the temporal and nasal quadrants. From these prior findings, it is likely to be said that HRT falsely measured the optic disc configuration in eyes with CON. One possible reason is the following. HRT automatically determines the reference plane 50 μm below the mean retinal surface at the temporal sector of the contour line between 350 and 356 degree, which is located on the papillomacular bundle, because RNFL thickness of this location is assumed to be 50 μm without considerable individual variation.5, 6 Cup area is defined as the area beneath this reference plane. In glaucoma, RNFL thickness of this specific location is supposed to be preserved until the advanced stage.37 Therefore, glaucomatous changes of ONH can be evaluated properly based on this reference level. However, in eyes with band atrophy of the disc, in which the temporal rim height is decreased with relative sparing of the superior and inferior rim height, the reference plane is depressed due to the temporal rim thinning. Such an inadequate referencing may cause the underestimation of the cup parameters as well as the overestimation of the rim parameters in eyes with CON. Further studies are necessary to confirm our hypothesis.
In conclusions, the ONH configuration determined by HRT was quite different among the three types of optic neuropathy. When a default set of the reference plane is used, caution must be made to interpret the HRT parameters obtained from the eyes with band atrophy due to CON.
References
Miglior S, Casula M, Guareschi M, Marchetti I, Iester M, Orzalesi N . Clinical ability of Heidelberg Retina Tomograph examination to detect glaucomatous visual field changes. Ophthalmology 2001; 108: 1621–1627.
Miglior S, Albé E, Guareschi M, Rossetti L, Orzalesi N . Intraobserver and interobserver reproducibility in the evaluation of optic disc stereometric parameters by Heidelberg Retina Tomograph. Ophthalmology 2002; 109: 1072–1077.
Wollstein G, Garway-Heath DF, Fontana L, Hitchings RA . Identifying early glaucomatous changes. Ophthalmology 2000; 107: 2272–2277.
Yücel YH, Gupta N, Kalichman MW, Mizisin AP, Hare W, de Souza Lima M et al. Relationship of optic disc topography to optic nerve fiber number in glaucoma. Arch Ophthalmol 1998; 116: 493–497.
Burk ROW, Vihanninjoki K, Bartke T, Tuulonen A, Airaksinen PJ, Völcker H-E et al. Development of the standard reference plane for the Heidelberg Retina Tomograph. Graefe's Arch Clin Exp Ophthalmol 2000; 238: 375–384.
Vihanninjoki K, Burk ROW, Teesalu P, Tuulonen A, Airaksinen J . Optic disc biomorphometry with the Heidelberg Retina Tomograph at different reference levels. Acta Ophthalmol Scand 2002; 80: 47–53.
Beck RW, Savino PJ, Repka MX, Schatz NJ, Sergott RC . Optic disc structure in anterior ischemic optic neuropathy. Ophthalmology 1984; 91: 1334–1337.
Beck RW, Servais GE, Hayreh SS . Anterior ischemic optic neuropathy IX. Cup-to-disc ratio and its role in pathogenesis. Ophthalmology 1987; 94: 1503–1508.
Danesh-Meyer HV, Savino PJ, Sergott RC . The prevalence of cupping in end-stage arteritic and nonarteritic anterior ischemic optic neuropathy. Ophthalmology 2001; 108: 593–598.
Doro S, Lessell S . Cup-disc ratio and ischemic optic neuropathy. Arch Ophthalmol 1985; 103: 1143–1144.
Jonas JB, Xu L . Optic disc morphology in eyes after nonarteritic anterior ischemic optic neuropathy. Invest Ophthalmol Vis Sci 1993; 34: 2260–2265.
Tesser RA, Niendolf ER, Levin LA . The morphology of an infarct in nonarteritic anterior ischemic optic neuropathy. Ophthalmology 2003; 110: 2031–2035.
Hatreh SS . Pathogenesis of cupping of the optic disc. Br J Ophthalmol 1974; 58: 863–875.
Rath E, Rehany U, Linn S, Rumelt S . Correlation between optic disc atrophy and aetiology: anterior ischemic optic neuropathy vs optic neuritis. Eye 2003; 17: 1019–1024.
Danesh-Meyer HV, Savino PJ, Spaeth GL, Gamble GG . Comparison of arteritic and nonarteritic anterior ischemic optic neuropathies with the Heidelberg Retina Tomograph. Ophthalmology 2005; 112: 1104–1112.
Henkind P, Charles NC, Pearson J . Histopathology of ischemic optic neuropathy. Am J Ophthalmol 1970; 69: 78–90.
Danesh-Meyer HV, Carroll SC, Ku JYF, Hsiang J, Gaskin B, Gamble GG et al. Correlation of retinal nerve fiber layer measured by scanning laser polarimeter to visual field in ischemic optic neuropathy. Arch Ophthalmol 2006; 124: 1720–1726.
Deleon-Ortega J, Carroll KE, Arthur SN, Girkin CA . Correlations between retinal nerve fiber layer and visual field in eyes with nonarteritic anterior ischemic optic neuropathy. Am J Ophthalmol 2007; 143: 288–294.
Lauer SA, Ackerman J, Sunness J, Bluth EM, Kim CK . Leber's optic atrophy with myopia masquerading as glaucoma: case report. Ann Ophthalmol 1985; 17: 146–148.
Mashima Y, Kimura I, Yamamoto Y, Ohde H, Ohtake Y, Tanimo T et al. Optic disc excavation in the atrophic stage of Leber's hereditary optic neuropathy: comparison with normal tension glaucoma. Graefe's Arch Clin Exp Ophthalmol 2003; 241: 75–80.
Ortiz RG, Newman NJ, Manoukian SV, Diesenhouse MC, Lott MT, Wallace DC . Optic disc cupping and electrocardiographic abnormalities in an American pedigree with Leber's hereditary optic neuropathy. Am J Ophthalmol 1992; 113: 561–566.
Radius RL, Maumenee AE . Optic atrophy and glaucomatous cupping. Am J Ophthalmol 1978; 85: 145–153.
Sadun F, Negri AM, Carelli V, Salomao SR, Berezovsky A, Andrade R et al. Ophthalmologic findings in a large pedigree of 11778/haplogroup J Leber hereditary optic neuropathy. Am J Ophthalmol 2004; 137: 271–277.
Trobe JD, Glaser JS, Cassady JC . Optic atrophy. Differential diagnosis by fundus observation alone. Arch Ophthalmol 1980; 98: 1040–1045.
Weiner NC, Newman NJ, Lessell S, Johns DR, Lott MT, Wallace DC . Atypical Leber's hereditary optic neuropathy with molecular confirmation. Arch Neurol 1993; 50: 470–473.
Barboni P, Savini G, Valentino ML, Montagna P, Cortelli P, Negri AMD et al. Retinal nerve fiber layer evaluation by optical coherence tomography in Leber's hereditary optic neuropathy. Ophthalmology 2005; 112: 120–126.
Carelli V, Ross-Cisneros FN, Sadun AA . Optic nerve degeneration and mitochondrial dysfunction: genetic and acquired optic neuropathies. Neurochem Int 2002; 40: 573–584.
Carelli V, Ross-Cisneros FN, Sadun AA . Mitochondrial dysfunction as a cause of optic neuropathies. Prog Rerin Eye Res 2004; 23: 53–89.
Sadun AA, Kashima Y, Wurdeman AE, Dao J, Heller K, Sherman J . Morphological findings in the visual system in a case of Leber's hereditary optic neuropathy. Clin Neurosci 1994; 2: 165–2172.
Sadun AA, Win PH, Ross-Csineros FN, Walker SO, Carelli V . Leber's hereditary optic neuropathy differentially affects smaller axons in the optic nerve. Trans Am Ophthalmol Soc 2000; 98: 223–232.
Bianchi-Marzoli S, Rizzo III JF, Brancato R, Lessell S . Quantitative analysis of optic disc cupping in compressive optic neuropathy. Ophthalmology 1995; 102: 436–440.
Kalenak JW, Kosmorsky GS, Hassenbusch SJ . Compression of the intracranial optic nerve mimicking unilateral normal-pressure glaucoma. J Clin Neuro-ophthalmol 1992; 12: 230–235.
Kupersmith MJ, Krohn D . Cupping of the optic disc with compressive lesions of the anterior visual pathway. Ann Ophthalmol 1984; 16: 948–953.
Manor RS . Documented optic disc cupping in compressive optic neuropathy. Ophthalmology 1995; 102: 1577–1578.
Portney GL, Roth AM . Optic cupping caused by an intracranial aneurysm. Am J Ophthalmol 1977; 84: 98–103.
Kanamori A, Nakamura M, Matsui N, Nagai A, Nakanishi Y, Kusuhara S et al. Optical coherence tomography detects characteristic retinal nerve fiber layer thickness corresponding to band atrophy of the optic discs. Ophthalmology 2004; 111: 2278–2283.
Jonas JB, Fernández MC, Stürmer J . Pattern of glaucomatous neuroretinal rim loss. Ophthalmology 1993; 100: 63–68.
Acknowledgements
This study was supported in part by Grant-in-Aid No. 16390499 (AN, MN), and No. 17591835 (MN) from the Ministry of Education, Culture, Sports, Science and Technology of the Japanese Government, by Uehera Memorial Foundation (MN), and by Suda Memorial Foundation for Glaucoma Research (MN). MN is a recipient of the 12th ROHTO award for Ophthalmic Research.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was partly presented at International Neuro-Ophthalmology Society Meeting 2004 in GenevaConflict of interest: None
Rights and permissions
About this article
Cite this article
Nagai-Kusuhara, A., Nakamura, M., Kanamori, A. et al. Evaluation of optic nerve head configuration in various types of optic neuropathy with Heidelberg Retina Tomograph. Eye 22, 1154–1160 (2008). https://doi.org/10.1038/sj.eye.6702871
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702871
Keywords
This article is cited by
-
The optic nerve head in acquired optic neuropathies
Nature Reviews Neurology (2010)
-
The optic nerve head in hereditary optic neuropathies
Nature Reviews Neurology (2009)
-
Phosphodiesterase type 5 inhibitors, visual changes, and nonarteritic anterior ischemic optic neuropathy: Is there a link?
Current Urology Reports (2007)