Abstract
Purpose
Cystic fibrosis (CF) is the most frequent lethal autosomal recessive hereditary disorder. The disease affects all secretory epithelia, including the eye, and belongs to the group of ocular surface epithelial diseases, termed keratoconjunctivitis sicca or dry eye syndrome. The aim of this study was to evaluate goblet cell population and conjunctival epithelial morphology in patients with CF.
Methods
A total of 20 CF patients and 20 controls underwent conjunctival impression cytology.
Results
Impression cytology showed conjunctival squamous metaplasia and goblet cell loss in patients with CF.
Conclusion
Reduced goblet cell numbers and squamous metaplasia may be indicative of a higher degree of epithelial damage of conjunctival epithelial cells in CF patients, and the presence of neutrophils is a strong sign for an inflammatory background of this disease.
In view of the simple, noninvasive nature of impression cytology, this technique may prove to be an important tool for the diagnosis and monitoring of dry eye changes in CF patients.
Similar content being viewed by others
Introduction
Cystic fibrosis (CF) is the most frequent lethal autosomal recessive hereditary disorder in Caucasian populations and is caused by mutations in the CF transmembrane conductance regulator (CFTR) gene, whose product functions as a cyclic adenosine monophosphate-regulated chloride channel in epithelial membranes.1, 2 The absent or deficient expression of CFTR protein leads to the classic CF phenotype of raised sweat chloride, recurrent respiratory infection with bronchiectasis, and early-onset pancreatic insufficiency.3
It is presumed that the disease affects all secretory epithelia including the eye.4, 5 The pathogenesis of ocular changes in CF is still unknown. CF belongs to the group of ocular surface epithelial diseases, termed keratoconjunctivitis sicca (KCS) or dry eye syndrome.4, 6 The causes of dry eye are multifactorial and can be related to deficiencies in any one of the components of the ocular surface and tear film.7 An increased understanding of the changes at the ocular surface, including alterations at the cellular level in the conjunctiva, may help explain the pathogenesis of dry eye and the subsequent clinical appearance of this potentially blinding disorder.
Conjunctival impression cytology (CIC) is a relatively simple, practical, and noninvasive, or minimally invasive technique, allowing the collection of one to three layers of cells from the bulbar conjunctival surface.8, 9 This technique is rapid and convenient and is widely performed on subjects to confirm a variety of ocular surface diseases and to monitor changes in the conjunctival surface.10, 11
The aim of this investigation was to compare conjunctival modifications at a cellular level in impression cytology specimens from both CF patients and asymptomatic healthy individuals.
Materials and methods
Forty eyes of 20 patients with CF (9 males, 11 females) between 7 and 23 years of age (mean, 14.82 years) as well as 40 eyes of 20 normal subjects whose age ranged from 8 to 22 years (mean, 15.51 years; 10 males, 10 females) were recruited from the III Department of Pediatric Diseases, Medical University of Bialystok, Poland, during March 2005 through January 2006. Both groups were similar regarding age and gender characteristics. All CF patients received daily 8000 IU of vitamin A. From the time of examination, the patients were taking pancreatic enzyme supplements and oral ambroxol hydrochloride. Fifteen patients were chronically infected with pulmonary Pseudomonas aeruginosa and therefore on maintenance treatment with nebulized colistin sulphomethate. No patients were being treated with systemic or topical corticosteroids at the time of impression cytology. The studies were conducted according to the principles established in the Declaration of Helsinki. Informed consent was obtained from the patients or from their parents before impression cytology.
After topical anaesthesia with one drop of 0.04% oxybuprocaine, two filterstrips, 13 × 6.5 mm in size (polyethersulphone filters, 0.20-μm pores, Supor, Gelman Sciences, Ann Arbor, MI, USA), were applied onto the superior and superotemporal bulbar conjunctiva of both eyes without exerting any pressure.8, 12 After fixation in 96% ethanol, the specimens were stained with PAS, H&E, and using the methods of May–Grunwald–Giemsa and Feulgen. Next, the specimens were dehydrated with ascending grades of ethanol and with xylene, and finally coverslipped.
Conjunctival epithelial cells were analysed microscopically with regard to their shape, size, the nucleus-to-cytoplasm (N/C) ratio, and nuclear chromatin condensation. The specimens were assigned a grade of conjunctival epithelial squamous metaplasia according to an adaptation of Nelson's grading scheme used by Nelson10 and De Rojas et al.13
The mean goblet cell densities were counted in five randomly selected microscopic fields, each field of 0.785 mm2 of the analysed eye section area. The analysis of the preparations and their photographic documentation were performed with an Olympus B × 50 light microscope, with video circuit and a Pentium 120 PC with Lucia G (Nikon) software for microscope image analysis.
The statistical analysis of the results was performed using Wilcoxon's sum rank test. A level of P⩽0.05 was considered statistically significant.
Results
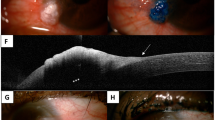
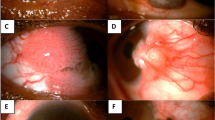
The average grade of squamous metaplasia in control subjects was 0.52±0.13 and in patients with CF it was 2.01±0.25 (P=0.00013) (Figures 1 and 2). There no was no individual with grade 2 or 3 squamous metaplasia among the controls.
The average goblet cell densities were significantly lower in patients with CF (97±55.93) when compared with those of the control group (320±104.30) (P<0.001).
In four patients (eight eyes) with CF, we found the presence of inflammatory cells such as mainly neutrophils (Figure 3).
Discussion
In this study, we investigated the morphological changes in conjunctival epithelial cells in CF patients. We performed CIC to find clues for dry eye. Impression cytology provided useful information about the nature of the ocular changes in CF patients, which was characterized by goblet cell loss and squamous metaplasia similar to other dry eye disorders.14, 15, 16 Squamous metaplasia is a transition from a non-keratinized, stratified (secretory or non-secretory) epithelium (such as conjunctival or corneal) to a non-secretory keratinized epithelium. During squamous metaplasia of the conjunctival epithelium, there is a continuous spectrum of changes, with an early decrease and eventual loss of goblet cells and progressive morphological changes of non-goblet epithelial cells such as increased stratification and keratinization. Round blue cells with N/C ratios of 1/1 transform into more elongated and flattened (squamoid) cells with metachromatic changes of the cytoplasm (pinkish colour), and N/C ratios increasing up to 1/8 and becoming pyknotic.8 As noted, these changes occur mainly in dry eye-related conditions.14, 15, 16, 17
In our patients, we also found the presence of inflammatory cells. It is known that impression cytology has made an important contribution to the understanding of dry eye as an immune-based inflammatory condition.18 Pflugfelder et al19 showed that over 60% of the inflammatory cells seen in the inferior fornix of Sjögren's syndrome patients were T lymphocytes. Conjunctival epithelium from dry eyes harvested by impression cytology has been shown to overexpress inflammatory markers such as HLA-DR, ICAM-1, the low-affinity receptor for IgE CD23, CD40-CD440L, or Fas and APO2.7 levels by immunocytochemistry and flow cytometry.12, 20, 21, 22, 23, 24, 25 Several previous studies have shown higher levels of ICAM-1 and many proinflammatory cytokines in the conjunctival epithelium from Sjögren's syndrome patients, analysed by immunofluorescence, RT-PCR, and ELISA.19, 26, 27
In summary, our findings of less goblet cell numbers and squamous metaplasia may be indicative of a higher degree of epithelial damage of conjunctival epithelial cells in CF patients, and the presence of neutrophils is a strong indicator of an inflammatory aetiology for this disease.
In view of the simple, noninvasive nature of impression cytology, this technique may prove to be an important tool for the diagnosis and monitoring of dry eye changes in patients with CF.
References
Riodan JR, Rommens JM, Kerem B . Identification of the cystic fibrosis gene: cloning and characterization of complementary DNA. Science 1989; 245: 1066–1073.
Zielinski J, Rozmahel R, Bozon D . Genomic DNA sequence of the cystic fibrosis transmembrane conductance regulator. Genomics 1991; 10: 241–248.
Welsh MJ, Anderson MP, Rich DP . Cystic fibrosis, CFTR and abnormal electrolyte transport. In: Davis PB (ed). Lung Biology in Health and Disease. M Dekker: New York, 1993 pp 29–32.
Castagna I, Roszkowska AM, Fama F, Sinicropi S, Ferreri G . The eye in cystic fibrosis. Eur J Ophthalmol 2001; 11: 9–14.
Turner HC, Bernstein A, Candia OA . Presence of CFTR in the conjunctival epithelium. Curr Eye Res 2002; 24: 182–187.
Mrugacz M, Minarowska A, Bakunowicz-Łazarczyk A, ywalewska N . Dry eye syndrome in children with cystic fibrosis. Med Wieku Rozwoj 2004; 8: 865–870.
Baudouin C . The pathology of dry eye. Surv Ophthalmol 2001; 45: 211–220.
Calonge M, Diebold Y, Saez V, Enriquez de Salamanca A, Garcia-Vazquez C, Corrales RM et al. Impression cytology of the ocular surface: a review. Exp Eye Res 2004; 78: 457–472.
McKelvie P . Ocular surface impression cytology. Adv Anat Pathol 2003; 10: 328–337.
Nelson JD . Impression cytology. Cornea 1988; 7: 71–81.
Inatomi T, Spurr-Michaud S, Tisdale AS, Gipson IK . Human corneal and conjunctival epithelia express MUC1 mucin. Invest Ophthalmol Vis Sci 1995; 36: 1818–1827.
Baudouin C, Brignole F, Becquet F, Pisella PJ, Goguel A . Flow cytometry in impression cytology specimens. A new method for evaluation of conjunctival inflammation. Invest Ophthalmol Vis Sci 1997; 38: 1458–1464.
De Rojas MV, Rodriquez MT, Ces Blanco JA, Salorio MS . Impression cytology in patients with keratoconjunctivitis sicca. Cytopathology 1993; 4: 347–355.
Adams AD, Dilly PN, Kirkenss CM . Monitoring ocular disease by impression cytology. Eye 1998; 2: 506–516.
Murube J, Rivas L . Impression cytology on conjunctiva and cornea in dry eye patients establishes a correlation between squamous metaplasia and dry eye clinical severity. Eur J Ophthalmol 2003; 13: 115–127.
Tseng SCG . Staging of conjunctival squamous metaplasia by impression cytology. Ophthalmology 1985; 92: 728–733.
Albietz JM . Conjunctival histologic findings of dry eye and non-dry eye contact lens wearing subjects. CLAO J 2001; 27: 35–40.
Stern ME, Beuerman RW, Fox RI, Gao J, Mircheff AK, Pflugfelder SC . The pathology of dry eye: the interaction between the ocular surface and lacrimal glands. Cornea 1998; 17: 584–589.
Pflugfelder SC, Jones D, Ji Z, Afonso A, Monroy D . Altered cytokine balance in the tear fluid and conjunctiva of patients with Sjögren's syndrome keratoconjunctivitis sicca. Curr Eye Res 1999; 19: 210–211.
Baudouin C, Haouat N, Brignole F, Bayle J, Gastaud P . Immunopathological findings in conjunctival cells using immunofluorescence staining of impression cytology specimens. Br J Ophthalmol 1992; 76: 545–5498.
Mrugacz M, Zywalewska N . HLA-DR antigen expression on conjunctival epithelial cells in patients with dry eye. Klin Oczna 2005; 107: 278–279.
Bourcier T, De Saint-Jean M, Brignole F, Goguel A, Baudouin C . Expression of CD40 and CD40 ligand in the human conjunctival epithelium. Invest Ophthalmol Vis Sci 2000; 41: 120–126.
Pisella PJ, Brignole F, Debbasch C, Pharm D, Lozato PA, Creuzot-Garcher C et al. Flow cytometric analysis of conjunctival epithelium in ocular rosacea and keratoconjunctivitis sicca. Ophthalmology 2000; 107: 1841–1849.
Brignole F, Pisella PJ, Goldshild M, De Saint Jean M, Goguel A, Baudouin C . Flow cytometric analysis of inflammatory markers in conjunctival epithelial cells of patients with dry eyes. Invest Ophthalmol Vis Sci 2000; 41: 1356–1363.
Brignole F, Pisella PJ, Goldshild M, De Saint Brignole F, Pisella PJ, De Saint Jean M et al. Flow cytometric analysis of inflammatory markers in KCS: 6-month treatment with topical cyclosporin A. Invest Ophthalmol Vis Sci 2001; 42: 90–95.
Jones DT, Monroy D, Ji Z, Atherton SS, Pflugfelder SC . Sjögren's syndrome: cytokine and Epstein–Barr viral gene expression within the conjunctival epithelium. Invest Ophthalmol Vis Sci 1994; 35: 3493–3504.
Solomon A, Dilek D, Liu Z, Xie Y, Macri A, Pflugfelder SC . Pro- and anti-inflammatory forms of interleukin-1 in the tear fluid and conjunctiva in patients with dry-eye disease. Invest Ophthalmol Vis Sci 2001; 42: 2283–2292.
Acknowledgements
This work was supported by a grant from the Ministry of Science and Higher Education (no. N406 051 31/1894).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Mrugacz, M., Kasacka, I., Bakunowicz-Lazarczyk, A. et al. Impression cytology of the conjunctival epithelial cells in patients with cystic fibrosis. Eye 22, 1137–1140 (2008). https://doi.org/10.1038/sj.eye.6702867
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702867