Abstract
Purpose
To describe the retinal nerve fibre layer (RNFL) characteristics in patients suffering vigabatrin-associated visual field loss or behaviour consistent with field loss.
Methods
Eight patients with visual field loss attributed to vigabatrin use had their RNFL evaluated by scanning laser polarimetry.
Results
All eight patients managed to perform the test reliably. The mean length of vigabatrin treatment was 81 months with a mean cumulative dose of vigabatrin being 5.4 kg. All patients had significantly reduced RNFL parameters; mean TSNIT=36.5 μm, mean nerve fibre indicator=63.1, mean superior average=42.7 μm, and mean inferior average=39.2 μm. There was no correlation between cumulative dose or time on treatment and RNFL thickness.
Conclusion
Scanning laser polarimetry can be performed safely and reliably on patients with vigabatrin-associated field loss. RNFL thickness is reduced in these patients with vigabatrin-associated field loss. RNFL loss concentrates on the long nerve fibres, which explains the nasal pattern of field loss seen in these patients. This investigation shows promise in the screening of vigabatrin patients, especially in those patients that may not tolerate formal field testing well.
Similar content being viewed by others
Introduction
Vigabatrin (Sabril, Hoechst Marion Roussel/Aventis Ltd) is an inhibitor of γ-aminobutyric (GABA) transaminase and has been used as an effective second-line medication in the treatment of infantile seizures,1 seizures associated with tuberous sclerosis,2 and epilepsy of partial onset.3 Its action is to potentiate the effect of GABA—an inhibitory neurotransmitter—by preventing its inactivation.
The first reports of vigabatrin-associated field loss were published in 19974 and since then numerous reports have been published leaving no doubt as to the validity of this relationship, with bilateral field defects generally developing in 40–45% of patients.5, 6, 7 The typical visual field loss is unusual in that it is one of the few causes of bilateral nasal field loss with temporal sparing. Screening for field defects with vigabatrin use is essential; however, a high proportion of patients taking this medication are unable to perform reliable field examinations due to their age or associated learning difficulties.
The use of vigabatrin is now being limited to only the very severe cases with the Committee on the Safety of Medicines advocating its use only where all other combinations of anti-epileptic medication have proved ineffective (save for West's syndrome). Vigabatrin-associated field loss is now a well-recognised side effect of treatment, and guidelines issued by the Royal College of Ophthalmologists in 20008 advised that all patients should undergo formal visual field examination as a baseline before starting treatment, then at 6 monthly intervals for 3 years and later annually following this. The guidelines highlights the problems that are inherent with visual field testing of children and in adults with learning difficulties, common in this patient population due to their multiple seizures.
Field-specific visual-evoked potential (VEP) have been shown to be effective in testing for visual field loss.9 This investigation, although not relying on patient cooperation as much, is time consuming, can be daunting to patients, and requires a high level of operator expertise in order to be carried out effectively. Many papers have been written regarding the clinical signs that may be seen with vigabatrin-associated field loss and it has been previously postulated whether imaging of the retinal nerve fibre layer (RNFL) could be of help. Choi and Kim10 published a short report on RNFL photography in such a patient. Buncic et al11 described three paediatric cases in which the loss of RNFL could be seen clinically, although they do state that in the majority of cases that they examined, this RNFL loss could not be seen. Wild et al12 recently reported encouraging results of a prospective study investigating such patients using optical coherence tomography (OCT) and confocal scanning laser ophthalmoscopy of the RNFL.
The aim of this study was to investigate the RNFL in patients with known vigabatrin-associated field loss using the GDx VCC scanning laser polarimeter. A secondary aim was to investigate the possible practical use of scanning laser polarimetry in the screening of these patients.
Methods
Subjects
The study is a prospective case series. All eight subjects had a history of vigabatrin use for epilepsy over variable lengths of time. Patients were examined either to assess any progression of previously documented visual field loss or if the patient showed behaviour consistent with visual field loss and field testing was impossible due to learning difficulties. Vigabatrin dosage was assessed from the patient's medical notes. In three patients, the intra-ocular pressure (IOP) could not be measured, due to their learning difficulties; however, glaucomatous damage was ruled out by fundoscopy. The remaining five patients had normal IOP measurements with normal optic disc appearances. All subjects had no previous ocular surgery, trauma, or other ophthalmic disease. Standard automated visual perimetry was attempted on all patients. Scanning laser polarimetry was attempted on all patients. OCT was carried out in all patients to ensure no macula pathology. The statistics were performed using Microsoft Excel package and although they are mainly descriptive, correlation between dose and findings was performed.
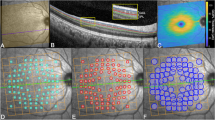
The GDx VCC (Carl Zeiss Meditec) is a commercially available scanning laser polarimeter, which gives an objective measurement of RNFL thickness with the actual measurements being taken in less than one second, working best on undilated pupils. A normative database compares the patient's measurements to those of normal patients of the same age, sex, and race. The GDx printout (version 5.5.0) concentrates on parameters which have been shown to be the most helpful in determining RNFL loss; TSNIT average (95% CI in healthy individuals 53.4–56.1 μm); superior average (95% CI in healthy individuals 65–68.4 μm); inferior average (95% CI in healthy individuals 59.4–63.6 μm); and nerve fibre indicator (NFI) a support vector machine-derived algorithm indicating the degree of RNFL loss ranging from 0 to 100 (95% CI in healthy individuals 19.2–23.1).13 All these parameters were analysed.
Results
Eight patients were identified who had taken vigabatrin in the treatment of epilepsy (Table 1). No distinction was made between the types of seizure that was being treated.
Five patients were male and the average age was 33 (range 22–61). All patients had discontinued vigabatrin at the time of testing. The mean length of vigabatrin treatment was 81 months (range 18–154) and the mean cumulative dose of vigabatrin was 5.4 kg (range 0.6–11.2). The visual acuities ranged from 6/6 to 6/18. OCT measurements in all cases were within normal ranges. In three of the eight cases, visual field testing was not possible due to patient non-cooperation.
Clinical examination in all patients was normal save for loss of the normal RNFL sheen.
Specifically there was no optic atrophy or disc cupping seen.
All patients could perform the test quickly and with good scan quality. All patients had abnormal GDx VCC results (Table 2).
The mean TSNIT average was 36.5 μm (range 28.3–46.6; SD 5.9), the mean NFI was 63.1 (range 24–87; SD 19.2). The most striking changes were with mean superior average of 42.7 μm (range 35.7–58.9; SD 6.1) and mean inferior average of 39.2 μm (range 20.4–53.5; SD 10.0). There was no correlation between cumulative dose and any of the GDx parameters (NFI, Pearson's rank coefficient r=−0.05; TSNIT average, r=−0.01; superior average, r=−0.06; inferior average, r=0.09) or between months on treatment and any parameter (NFI, r=0.01; TSNIT average, r=−0.01; superior average, r=−0.16; inferior average, r=0.04).
Discussion
Our results show that scanning laser polarimetry detects RNFL thinning in patients who have been exposed to vigabatrin in the treatment of epilepsy. All of the parameters that give an indication of RNFL loss are altered with the layer thickness parameters (TSNIT average, superior average, inferior average) being reduced from that seen in the normal population and the NFI increased as would be expected. Although a control group was not used specifically as part of the study, the normal values detailed above are gained from the normal population and can act as a control.
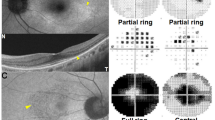
The pattern of RNFL loss is remarkably consistent in our patients with the long nerve fibres being primarily affected (Figure 1). This explains the nasal pattern of visual loss that is reported. Interestingly there was no clinical evidence of disc cupping, pallor or atrophy in our patients with clinical examination revealing normal optic discs in all patients in contrast to previous case reports.11, 12 It may be that optic atrophy is seen only in late stage disease and our patients may go on to develop optic pallor in the future; however, we do have a wide range of treatment times (up to 13 years) so one would expect any recognisable optic atrophy to be evident. The pattern of RNFL loss seen is in complete agreement with previous papers detailing RNFL loss in vigabatrin-associated field loss.
Vigabatrin-associated field defect development is multi-factorial and the reason for its development is not clear. Vigabatrin is an inhibitor of GABA transaminase and it reaches much higher concentrations in the retina than in the brain.14 Rod photoreceptors do not have any GABA receptors unlike cones, ganglion, amacrine, and bipolar cells, and recent animal testing suggests that vigabatrin causes irreversible death of cone photoreceptors and ganglion cells with secondary atrophy of the RNFL.15 If this does prove to be the mechanism of damage, then RNFL assessment would provide a screening tool that would reveal damage before visual field damage would be evident through formal field testing.
The main reason that we chose to investigate these patients, who were already under our care, in this manner, is because the detection of vigabatrin-associated field loss currently relies on standard visual field testing. All current methods of field testing require significant cooperation of the patient. The development and use of reliable tests, which could be easily performed in patients either with learning problems, cognitive dysfunction, or in childhood is essential. In this context, the use of scanning laser polarimetry may be a promising diagnostic alternative. All our patients managed to perform the scan easily, unlike the visual field testing in which three patients failed. Other screening tools, standard ERG or field-specific VEP techniques, can be used in laboratory settings but are not practical for clinical use without a large increase in resources. We are aware that our series only contains few patients and that before advocating its widespread acceptance much more work needs to be performed. Similar reports utilising various RNFL imaging techniques10, 11, 12 show similar characteristics; however, we feel that a purely objective test, as found with the GDx or OCT,12 provides a more rigorous basis for deciding a patients future treatment plans.
With only eight patients we can draw no conclusions from the lack of correlation between cumulative dose and any of the GDx parameters; however, even with much larger studies there is variable evidence to suggest a dose-dependant relationship between the vigabatrin and subsequent field loss.16, 17 What is consistent though is that the field loss seems to occur in the first 2 or 3 years of therapy and then remains static. From our results we cannot give any indication of which level of NFI would give an indication of damage from a single scan; however, these preliminary tests do show that scanning laser polarimetry may also have a role in the future monitoring of these patients. It is likely that subtle defects will be found on polarimetry before the development of dense field loss, thus avoiding this complication that compounds the life style of these vulnerable patients.
Conclusion
This is the first reported case series showing that scanning laser polarimetry can be performed safely and reliably on patients with vigabatrin-associated field loss. It can be used in patients that cannot tolerate formal field testing. The nerve fibre layer loss concentrates on the long fibres, which explains the nasal pattern of field loss seen in these patients. We advocate the further investigation of the use of scanning laser polarimetry in the screening of patients taking vigabatrin.
References
Uldall P, Alving J, Gram L, Hogenhaven H . Vigabatrin in childhood epilepsy: a 5 year follow up study. Neuropediatrics 1995; 26: 253–256.
Curatolo P . Vigabatrin for refractory partial seizures in children with tuberous sclerosis. Neuropediatrics 1994; 25: 55.
Guberman A, Bruni J . The Canadian Vigabatrin Study Group. Long term open multicentre, add-on trial of vigabatrin in adult resistant partial epilepsy. Seizure 2000; 9: 112–118.
Eke T, Talbot JF, Lawden MC . Severe persistent visual field constriction associated with vigabatrin. BMJ 1997; 314: 180–181.
Lawden MC, Eke T, Degg C, Harding GFA, Wild JM . Visual field defects associated with vigabatrin therapy. J Neurol Neurosurg Psychiatry 1999; 67: 716–722.
Daneshvar H, Racette L, Coupland SG, Kertes PJ, Guberman A, Zakon D . Symptomatic and asymptomatic visual loss in patients taking vigabatrin. Ophthalmology 1999; 106: 1792–1798.
Wild JM, Martinez C, Reinshagen G, Harding GFA . Characteristics of a unique visual field defect attributed to vigabatrin. Epilepsia 1999; 40: 1784–1794.
Royal College of Ophthalmologists. Ocular Side Effects of Vigabatrin (Sabril) Information and Guidelines for Screening. Royal College of Ophthalmologists, 2000.
Spencer EL, Harding GF . Examining visual field defects in the paediatric population exposed to vigabatrin. Doc Ophthalmol 2003; 107: 281–287.
Choi HJ, Kim DM . Visual field constriction associated with vigabatrin: retinal nerve fiber layer photographic correlation. J Neurol Neurosurg Psychiatry 2004; 75: 1395.
Buncic JR, Westall CA, Panton CM, Munn JR, MacKeen LD, Logan WJ . Characteristic retinal atrophy with secondary “inverse” optic atrophy identifies vigabatrin toxicity in children. Ophthalmology 2004; 111: 1935–1942.
Wild JM, Robson CR, Jones AL, Cunliffe IA, Smith PEM . Detecting vigabatrin toxicity by imaging of the retinal nerve fiber layer. Invest Ophthalmol Vis Sci 2006; 47 (3): 917–924.
Reus NJ, Lemij HG . Diagnostic accuracy of the GDx VCC for glaucoma. Ophthalmology 2004; 111: 1860–1865.
Sills GJ, Butler E, Forrest G, Ratnaraj N, Patsalos PN, Brodie MJ . Vigabatrin, but not gabapentin or topiramate produces concentration related effects on enzymes and intermediates of the GABA shunt in rat brain and retina. Epilepsia 2003; 44: 886–892.
Duboc A, Hanoteau N, Simonutti M, Rudolf G, Nehlig A, Sahel JA et al. Vigabatrin, the GABA-transaminase inhibitor, damages cone photoreceptors in rats. Ann Neurol 2004; 55 (5): 695–705.
Manuchehri K, Goodman S, Siviter L, Nightingale S . A Controlled study of vigabatrin and visual abnormalities. Br J Ophthalmol 2000; 84 (5): 499–505.
Kinirons P, Cavalleri GL, O'Rourke D, Doherty CP, Reid I, Logan P et al. Vigabatrin retinopathy in an Irish cohort: lack of correlation of dose. Epilepsia 2006; 47 (2): 311–317.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Durnian, J., Clearkin, L. Retinal nerve fibre layer characteristics with vigabatrin-associated visual field loss—could scanning laser polarimetry aid diagnosis?. Eye 22, 559–563 (2008). https://doi.org/10.1038/sj.eye.6702794
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702794
Keywords
This article is cited by
-
Evaluation of inner retinal layers with optic coherence tomography in vigabatrin-exposed patients
Neurological Sciences (2017)