Abstract
Aims
To describe the value of monoclonal antibodies in the differential diagnosis of orbital lymphoproliferative disorders.
Methods
A total of 200 sequential cases of malignant lymphoma diagnosed at St Bartholomew's Hospital as part of the ocular lymphoma service at Moorfields Eye Hospital and the Institute of Ophthalmology have been examined. Cases were acquired between January 1998 and June 2005. Each case had detailed immunophenotypic analysis using a panel of monoclonal antibodies and was classified using the WHO classification of lymphoma. These cases are discussed in relation to earlier studies of orbital lymphoma reported by our group.
Results
Lymphomas fell into three main categories. Extranodal marginal zone lymphoma was the largest group with 151 cases, arising within the orbital soft tissue, conjunctiva and lacrimal gland. Cases arising in the conjunctiva and lacrimal gland showed a higher female predominance than those arising within the deeper soft tissue. A small number of cases were associated with organ specific autoimmunity, including thyroid eye disease complicating Graves’ disease. Follicular lymphoma and diffuse large B-cell lymphoma formed the next two groups, occurring with equal frequency. Many of the follicular lymphomas had evidence of disseminated disease on completion of staging. A miscellaneous group of T-cell and B-cell lymphomas formed a minority of cases during the study period.
Conclusion
Extranodal marginal zone lymphoma is the most frequent type of primary orbital and orbital adnexal lymphoma. Its major differential diagnosis is with orbital lymphoid hyperplasia, chronic dacryoadenitis, and follicular conjunctivitis. Systemic types of lymphoma may present within the orbit or involve the orbit secondarily.
Similar content being viewed by others
Introduction
Orbital lymphoma and lymphoma of the orbital adnexae are relatively rare lymphomas representing <1% of all lymphoma. In a recent series of cases reported by our group classified by the REAL scheme marginal zone lymphoma represented a major part.1 Owing to the limited phenotyping available in this series and often small size of the biopsies an indeterminate group termed ‘lymphoplasmacytoid’ accounted for a significant number of deeper orbital lymphomas. Since the publication of this study, the classification of lymphoma has moved towards the new WHO classification, which has retained many of the elements of REAL. Analysis of a more recent cohort of lymphomas with improved biopsy technique and phenotypic characterization should help to clarify the nature of this indeterminate group.
Materials and Methods
A total of 200 sequentially acquired cases of lymphoma sent for histopathological review at St Bartholomew's Hospital form the core of this study. The majority of these patients were diagnosed and treated as part of the ocular lymphoma service at Moorfields. Cases were acquired from January 1998 until June 2005. Thus, there is slight overlap with the earlier study. All cases were classified using the WHO scheme and subjected to analysis using a panel of monoclonal antibodies. All immunocytochemistry was performed on fixed and paraffin-embedded sections using standard methods and with heat-mediated antigen retrieval in a pressure cooker. Antibodies to CD3, CD5, CD10, CD20, CD21, CD23, bcl-2, and bcl-6 were used on most of the cases. In selected cases where the differential diagnosis was with a reactive disorder antibodies to Kappa and Lambda immunoglobulin light chains were used. Where the differential diagnosis included mantle cell lymphoma Cyclin-D1 protein stains were used.
Results
Out of 200 cases of lymphoma, 151 were extranodal marginal zone lymphomas (MZL), 19 follicular lymphoma (FL), 20 diffuse large B-cell lymphoma (DLBCL) and the rest a miscellaneous group. The latter comprised two Burkitt's lymphomas, 4T or NK cell lymphomas, two mantle cell lymphomas, one plasmacytoma/myeloma, and one post-transplant lymphoproliferative disorder. Two lymphomas (one Burkitt's and one DLBCL) arose in the setting of HIV infection. Although data was incomplete for all patients some of the MZL cases arose in the setting of Sjogren's syndrome and thyroid eye disease.
No lymphomas were classified as ‘lymphoplasmacytoid’ and all of the deep orbital tumours with lymphoplasmacytoid cytology had other features to support a diagnosis of MZL.
MZL had a typical ‘neutral’ phenotype CD20+, CD3−, CD5−, CD10−, CD21 weak and variable, CD23−, bcl-2+, bcl-6 —, and cyclin-D1- in the few cases where mantle cell lymphoma needed excluding. CD21 and CD23 revealed expanded and disrupted meshworks of follicular dendritic cells in all cases. Rarely reactive CD10+, bcl-2−, bcl-6+ follicle centres were trapped within the lymphomatous masses.
MZL arose in three principle sites; deep orbital soft tissue (115), conjunctiva (27), lacrimal gland (8). One exceptional case arose in the conjunctiva and anterior chamber. The median age at diagnosis was 75 with a range of 25–93. The male to female ratio differed by site; deep orbit M:F, 1:1.3: lacrimal and conjunctival combined, M:F, 1:2.2.
Although data is still incomplete marginal zone cases, showed similar rates and patterns of relapse to those described in our earlier series, involving regional nodes, skin, contralateral orbit, and other mucosal sites, including salivary gland and breast. One case showed an unusual late relapse around the cauda equina.
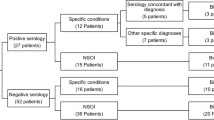
The major differential diagnosis for MZL was with florid follicular conjunctivitis, orbital lymphoid hyperplasia and chronic dacryoadenitis. All such cases were subjected to immunoglobulin light chain staining to confirm or refute the diagnosis of lymphoma.
FL and mantle cell lymphoma, in-keeping with their principally systemic disease distribution often had disease elsewhere at presentation or relapsed in the bone marrow, lymph nodes or bowel (mantle cell cases only). Just over half of the follicular cases were stage 1 at presentation. One case had an unusual and subtle presentation as a small conjunctival nodule.
DLBCL cases were localized at presentation and had similar variable phenotypes to other nonorbital cases: CD3-, CD5 rare+, CD10 ∼50%+, CD20+, CD21 variable, CD23 variable, bcl-2+, bcl-6+.
Rare types had phenotypes and immunoarchitecture as described in the literature.
Discussion
This study has expanded the findings of our earlier study of orbital lymphoma. Importantly the ‘lymphoplasmacytoid’ group has been abolished in favour of MZL. Furthermore, it was noted in that earlier study that these deeper orbital tumours had a higher rate of dissemination and relapse. Cytogenetic studies have also firmly placed orbital MZL in the greater family of MZL. Ye et al2 described t(11;18) translocations in a proportion of orbital MZL, a translocation first described in gastric MZL. More recently the t(14;18) involving the MALT 1 gene has been described by a number of groups.3, 4 As yet it is unclear as to the prognostic significance of these translocations in orbital MZL.
This study helps to reinforce the role of autoimmunity in the aetiology of some orbital and adnexal MZL. The higher prevalence of females with lymphoma in organ specific sites reinforces this view.
The distinction of orbital MZL from inflammatory mimics rests on good quality biopsy material, high-quality analysis of the immunoarchitecture and light chain studies when required. Clonal analysis by PCR has a role to play in only a minority of cases. The high frequency of somatic mutation in MZL and the difficulty of extracting good quality DNA from paraffin-embedded soft tissue biopsies produces a high false negative rate. Furthermore, the detection of a weak clone in an inflammatory disorder is a well-recognized hazard.
Other types of lymphoma clearly do arise within or directly infiltrate into the orbit from the neighbouring nasal sinuses. In most regards they differ little from their systemic counterparts in terms of morphology, phenotype, and clinical behaviour.
References
Jenkins C, Rose GE, Bunce C, Wright JE, Cree IA, Plowman N et al. Histological features of ocular adnexal lymphoma (REAL classification) and their association with patient morbidity and survival. Br J Ophthalmol 2000; 84: 907–913.
Ye H, Liu H, Attygalle A, Wotherspoon AC, Nicholson AG, Charlotte F et al. Variable frequencies of t(11;18)(q21;q21) in MALT lymphomas of different sites: significant association with CagA strains of H pylori in gastric MALT lymphoma. Blood 2003; 102: 1012–1018.
Sanchez-Izquierdo D, Buchonnet G, Siebert R, Gascoyne RD, Climent J, Karran L et al. MALT1 is deregulated by both chromosomal translocation and amplification in B-cell non-Hodgkin lymphoma. Blood 2003; 101: 4539–4546.
Streubel B, Lamprecht A, Dierlamm J, Cerroni L, Stolte M, Ott G et al. t(14;18)(q32;q21) involving IgH and MALT1 is a frequent chromosomal aberration in MALT lymphoma. Blood 2003; 101: 2335–2339.
Acknowledgements
I thank Prof P Luthert, and Dr G Meligonis at the Institute of Ophthalmology for their close working relationship. The contribution of other members of the ocular lymphoma service should also be recognized; Mr G Rose, Dr N Plowman and others who I have undoubtedly failed to recall.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Norton, A. Monoclonal antibodies in the diagnosis of lymphoproliferative diseases of the orbit and orbital adnexae. Eye 20, 1186–1188 (2006). https://doi.org/10.1038/sj.eye.6702478
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702478
This article is cited by
-
Non-Hodgkin-Lymphom der Tränendrüse
Der Ophthalmologe (2008)