Abstract
Aim
The mid-term appearance of the filtering bleb and surgical outcome following tunnel-trabeculectomy, in which protective measures were carried out to avoid contact between the mitomycin C (MMC) and the conjunctival flap, are presented.
Methods
In a retrospective study the records of 20 consecutive patients who had undergone tunnel-trabeculectomy ≥24 months earlier, using fornix-based conjunctival flap and MMC (0.4 mg/ml) application were evaluated. Inclusion criteria were patients in whom: (I) the MMC-socked sponge was applied without contact with the conjunctival flap; (II) during MMC washout, a second Weck cell sponge was held anterior to the conjunctival flap, to protect the flap from mitomycin contact during its back-flow. Excluded were five patients who either did not complete 24 months of follow-up (n=4) or underwent an intraocular surgery during that period (n=1).
Results
After 24–32 (26.9±2.2) months, the filtering bleb was completely vascularized and thick in 13/15 patients (86.7%), mostly vascularized with some para-limbal thick cysts in one and avascular and cystic in another. Mean intraocular pressure (IOP) dropped from a preoperative level of 25.3±7.0 mmHg with 3.5±0.9 hypotensive medications to 13.9±2.9 mmHg with 0.9±1.1 medications (P<0.0001, Wilcoxon test). Of the five excluded patients, the IOP ranged between 10 and 16 mmHg with 0–1 medications at the last examination, 1–15 months postoperatively.
Conclusion
In this pilot study, an intraoperative protection of the conjunctival flap from mitomycin contact was mostly associated with a vascularized and thick filtering bleb after mid-term follow-up. Further controlled prospective studies are required to confirm these observations.
Similar content being viewed by others
Introduction
Thin, elevated, or cystic blebs appear more frequently following standard trabeculectomy with intraoperative mitomycin C (MMC) application than without the use of antifibrosis agents.1, 2, 3, 4, 5 Such filtering blebs are at risk of late postoperative leakage, blebitis, and intraocular infection.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11 DeBry et al2 report that the incidence of a bleb leak or an infection after trabeculectomy with MMC continues at a fairly constant rate over time, 4.4% per patient-year. Parrish and Minckler12 state that the incidence of late-onset endophthalmitis following intraoperative MMC application is increasing over time (‘time-bomb’).
Thin, elevated, cystic filtering blebs following trabeculectomy with MMC are typically avascular.4, 8, 10 In this regard, Smith et al13 demonstrated that MMC could irreversibly damage the vascular endothelium. Hu et al3 report that the larger the avascular bleb area the more likely the bleb leaks, while Matsuo et al7 and associates found that avascular area was significantly more frequent in eyes with leak or oozing than in eyes without.
Regarding the site of MMC application, in a controlled study using sclerocorneal tunnel-trabeculectomy with scleral radial incisions, MMC-sponge (0.4 mg/ml) was applied for 5-min underneath and in contact with the conjunctival flap.11 Cystic blebs appeared during 3-years follow-up in 90% (18/20!) of eyes when a limbal-based conjunctival flap was performed, and in 29% (5/17) of eyes following fornix-based flap. The limbal-based cases have been associated with 20% incidence of bleb infections. The sclerocorneal tunnel approach, a modifications of Cairns trabeculectomy,14 gained popularity in recent years and several reports and modifications of it were reported.11, 15, 16, 17, 18, 19, 20
In the present study, protective measures were taken during fornix-based-flap tunnel-trabeculectomy (3-mm width),15 to prevent the internal wall of the flap from MMC touch both at time of its application and washout. As far as we are aware, based on Med-Line search, this has not previously reported. The surgical outcome and appearance of the filtering bleb ≥24 months post-surgery are presented.
Materials and methods
In a retrospective, interventional case series, the records of 20 consecutive patients who had undergone filtration surgery using fornix-based conjunctival flap and a 3-mm sclerocorneal tunnel approach with MMC (0.4 mg/ml) ≥24 months earlier were evaluated. Inclusion criteria for this study were: (I) consecutive patients who had undergone the filtration surgery in a superior quadrant with MMC application, without MMC-conjunctival touch; (II) patients in whom an intraoperative protection of the internal wall of the flap from MMC touch during MMC washout was carried out. Exclusion criteria were: (I) patients who did not complete at least 24 months of follow-up; (II) patients that had undergone additional ocular surgery during the follow-up period. The study was in adherence to the tenets of the Declaration of Helsinki. Informed consent was obtained from all patients.
A detailed preoperative evaluation, which included applanation tonometry, gonioscopy, and examination of the optic nerve head were carried out on each patient. The Humphrey Field Analyzer (Carl Zeiss Meditec, Dublin, CA, USA) was used for the visual field examination. Main outcome measures include the clinical morphology of the filtering bleb and its vascularization, and the surgical outcome. Hypotensive medications were prescribed according to the required target pressure. Complete surgical success was defined when last intraocular pressure (IOP) was ≤20 mmHg without hypotensive medication and at least 20% IOP reduction; qualified success was defined as last IOP ≤20 mmHg with hypotensive medication and surgical failure was defined when IOP was >20 mmHg with maximum tolerable medications. Bleb morphology was classified for its height, extent, vascularity, and Seidel testing, as previously described.21 In addition, classification was made for the thickness of the bleb wall, whether it was transparent (the bleb content and underlying sclera could be seen) or opaque.
Surgical technique
The scleral tunnel trabeculectomy using a 3-mm sclerostomy (‘mini-trabeculectomy’), has been previously described in detail.15 Briefly, the surgical procedure consists of a 3-mm fornix-based conjunctival flap. A Weck cell sponge, soaked with 0.4 mg/ml MMC was applied on both the scleral wound and the distal exposed bare sclera for 2 (in first-time surgery cases) or 3 min (in eyes with high-risk of postoperative scarring). The flap of conjunctiva-Tenon's capsule was pushed posteriorly by a Weck-cell sponge in order to avoid any contact between it and the MMC sponge (Figure 1).
After withdrawal of the MMC sponge, a Weck cell sponge was held anterior to the free conjunctiva, the site of the due filtering bleb (Figure 2). The scleral pocket was thoroughly irrigated with 20-ml of balanced salt solution (BSS). The crescent knife was reintroduced, a sclerocorneal pocket was completed, a viscoelastic substance was injected intracamerally, and a corneo-trabeculectomy was performed using a scleral punch. Peripheral iridectomy was followed by suturing the scleral wound with 1 or 2 sutures, slightly tighter in phakic eyes to prevent spontaneous flow and relatively loose in pseudophakic eyes to allow for guarded aqueous leak. The conjunctiva was closed at the limbus with one suture at each conjunctival edge.
From the first postoperative day, eyes were treated with steroid/antibiotic (dexamethazone/neomycin) drops, three to six times daily, depending on the bleb injection and the reaction in the anterior chamber. In case of marked congestion, cycloplegic eye drops were administered. Patients were followed-up daily during hospitalization, 1 week after surgery and frequently during the first postoperative month, until intraocular target pressure was achieved, the filtering bleb site was not hyperaemic and there were no signs of inflammation in the anterior chamber. Topical treatment was tapered off and discontinued after 4–6 weeks. Patients were then examined every 2–4 months. Subconjunctival injections of 5-mg 5-FU were typically administered 180° from the surgical site when there were signs of impending bleb scarring. Argon laser lysis of the scleral suture(s) was carried out when the IOP without hypotensive medications exceeded the target pressure. A modified needling of the filtering bleb associated with intrableb administration of 1-mg 5-FU followed by paracentesis via the bleb site was carried out when IOP remained elevated, as previously described.22
Statistical analysis
Comparison was made between the preoperative and last postoperative IOP of all eyes under study, using the Wilcoxon test. Comparison was also made between preoperative and last postoperative IOP in the first-surgery eyes (the current filtration surgery was the first trans-conjunctival ocular surgery) and between those IOPs at the eyes with high-risk of postoperative scarring, that is, eyes that had undergone a previous transconjunctival surgery.
Results
Surgical outcome
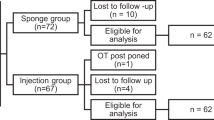
Of the 20 patients who underwent tunnel-trabeculectomy with intraoperative MMC ≥24 months earlier, 15 met the study criteria (Table 1): Seven underwent ocular surgery for the first time and eight had previously undergone intraocular operation. Excluded were the five remaining patients: discontinued follow-up (n=4) and cataract extraction before completion of 2-years of follow-up (n=1).
Complete success was found in six (40%) eyes and qualified success in nine eyes (Table 1). The mean IOP (n=15) dropped from a preoperative level of 25.3±7.0 mmHg with 3.5±0.9 hypotensive medications to 13.9±2.9 mmHg (45.1% drop) with 0.9±1.1 medication at the last examination, prescribed according to the required target pressure (P<0.0001). Of the patients' subgroups, that is, the first-surgery group and the high-risk group, the mean IOP of the seven first-surgery eyes dropped in 40% (from preoperative level of 26.0±9.0 to 15.6±2.4 mmHg; P=0.03), while in the eight high-risk eyes IOP dropped in 49.6% (from 24.6±5.2 to 12.4±2.4 mmHg; P<0.001). Figure 3 describes the IOP changes along with the number of hypotensive medications of the two subgroups during the various time intervals (±2–4 weeks).
Appearance of the filtering blebs
During the first postoperative phase, leakage from the wound site (Seidel test) was not detected in any of the eyes. The anterior chamber depth was within normal depth or somewhat shallow, with temporary touch between the peripheral cornea and the iris in three eyes (two of which in the first-surgery group). At 3 months postoperatively, 14 eyes presented with diffuse, thick and vascularized, most commonly noncongested blebs. At that time, the filtering bleb in the remaining eye (No. 4) was avascular in a large part of its wall, and elevated. Gradual, slow flattening of the diffuse blebs could be detected during follow-up in most eyes, finding that was often associated with gradual tendency towards an increase in IOP, and the need for hypotensive treatment in some eyes. The filtering bleb in eye No. 4 remained elevated and became progressively transparent. At the last examination the diffuse filtering blebs were thick and vascularized in 13 (86.7%) eyes (Figure 4a, b), in which two were flat (No. 9 and 11, Table 1). In another eye (No. 10) it was diffuse and mostly vascularized although with some thick microcysts, that is, cysts through which the bleb content or underlying sclera could not be seen (Figure 4c). In the remaining eye (No. 4), avascular, cystic, elevated, transparent bleb was evident. In all eyes but one (no. 11), microcysts could be detected within the bleb walls.
(a and b): Vascularized, thick, relatively shallow and diffuse filtering blebs following first-time filtration surgery with MMC. (c) Following a second filtration surgery (patient 10). Most of the filtering bleb is vascularized except in an area adjacent to the limbus, where few thick cysts are apparent (arrows).
Postoperative complications
Early postoperative side effects (Table 1) included IOP spikes of ≥30 mmHg in two eyes (13.3%), both in the initial surgery group, on days 3 and 7, respectively. These eyes were treated efficaciously by digital massage, argon laser suture-lysis, and subconjunctival injections of 5-FU. Early interventions included one to four injections of 5 mg 5-FU in eight eyes (53.3%), 180° away from the surgical site. In four eyes (26.6%), two in each subgroup, 5-FU-needling (1 mg 5-FU/0.1 ml) at the bleb site was carried out. Argon laser lysis of the scleral suture(s) was performed in four eyes (26.6%), two in each subgroup. None of the blebs leaked during the follow-up period.
Late postoperative complications (n=15) included one patient (No. 4) who underwent cataract extraction 24 months after the filtering operation. Examination at the last visit revealed improved BCVA in one patient (No. 9) from 3-m count fingers to 20/200, and reduced BCVA in one (No. 8) due to wet age-related macular degeneration. All other patients remained with the preoperative BCVA±1-Snellen's line difference.
Patients that were excluded from the study
Of the five patients who did not complete 24 months of follow-up, two had undergone initial surgery and three had a previous intraocular operation. At their last examination the filtering bleb was mildly congested (one eye, 1 month postoperatively), diffusely vascularized (three eyes, after 4, 8, and 15 months) or partially vascularized (one eye, 12 months postoperatively). Their IOP (and hypotensive medications) at the last examination were 10 (0), 15 (0), 14 (1), 12 (1), and 16 (0).
Discussion
At 24–32 months following tunnel-trabeculectomy with MMC and the use of protective measures to prevent MMC contact with the internal wall of the conjunctival flap, the filtering blebs were diffusely vascular and thick in 13/15 (86.7%) eyes, mostly vascularized with localized ischemic cysts in one eye and avascular and cystic in another eye. No bleb-related infection occurred during follow-up.
In comparison with earlier studies using fornix-based approach, the incidence of cystic blebs emergence following MMC-trabeculectomy seems to be higher when the flap was not-at-all or less protected: In our earlier study on mini-trabeculectomy, protection of MMC (0.4 mg/ml, 3 min) from touch with the conjunctival flap during its application, although without bleb protection during MMC washout, was carried out (same surgeon, AO). After mean of 22.1±6.6 months' follow-up the filtering blebs were diffusely ischemic and relatively thin in 25% of eyes, while additional eye was complicated by blebitis and endophthalmitis. Altogether, six of 21(28.6%) filtering blebs could be considered at risk of late bleb-related complications. Low and partially (number of eyes is not available) or diffusely vascularized blebs were apparent in the other eyes, but these missing data preclude statistical comparison between the studies. In the study of Wells et al,11 in which the MMC-sponge was wrapped by the fornix-based conjunctival flap, 29% of blebs became cystic during 3-years of follow-up. In the study of Casson et al6, 3 years after standard trabeculectomy using a fornix-based flap, in which the MMC-sponge (0.2 mg/ml, 2 min) was held in touch with the Tenon's capsule, cystic blebs were apparent in 47% (10/21) of eyes. Anand et al23 recently report on MMC augmented glaucoma surgery (trabeculectomy, combined phaco-trabeculectomy, or nonpenetrating deep sclerectomy; n=125). A fornix-based conjunctival flap was used in the trabeculectomy group, and MMC sponges (usually, 0.2 mg/ml for 2 min) were applied on the area of the planned scleral flap as well as subconjunctivally (using two to four more sponges). Most eyes developed bleb avascularity within the first year after surgery. In the eyes with avascular blebs, the probability of developing transconjunctival aqueous oozing with leak or without point leak was 12 and 81% at 12 months and 26 and 95% at 24 months.
However, when Wells et al used the limbal-based approach, including the wrapping of the MMC-sponge, 90% of blebs became cystic.11 In that regard, the filtering bleb tends to become similar or more elevated and cystic following standard trabeculectomy using the limbal-based approach than fornix-based flap one even without the use of antimetabolites; that occurs also following standard trabeculectomy and postoperative subconjunctival 5-fluorouracil (5-FU) injections.24, 25, 26
The aforementioned observations following surgery with MMC could be maybe explained as follows:15 since a connective tissue such the conjunctiva continuously changes throughout life, coupled with resolution and production of collagen, including an expression of the tissue metalloproteinases, an intraoperative mechanical injury to the substantia propria, especially when coupled with MMC toxicity to its vasculature,13 might reduce its potency to keep long-term tissue balance and reproduction of collagen, thus becoming progressively thinner.
Thus, the substantia propria of the limbal-based flap could be prone to both further intraoperative MMC contact as well as a mechanical injury than the fornix-based flap. As the substantia propria in the limbal-based flap is exposed to the surgical site, further mechanical injury might occur during pulling of the conjunctival flap, cleaning, or irrigating it from surgical debris, long irrigating during MMC washout (often by 20 ml of BSS), etc. A combination of mechanical tissue injury and MMC-conjunctival touch during its application and/or washout, before injury heals, together with an irreversible flap vasculature toxicity by the MMC, could be harmful to the conjunctiva. In contrast, during the fornix-based approach, the conjunctiva is pushed posteriorly. Its epithelial side rather than the substantia propria faces the surgical field, while the underlying substantia propria is less likely to be injured during the operation.
Relevant to our hypothesis, we assumed that in the fornix-based approach, backwards jets or flow of BSS-MMC towards the inner wall of the flap during MMC washout could touch the inner flap wall and thus irreversibly injure its tissue and vasculature. When BSS is irrigated through the sclerostomy towards the scleral pocket while the fornix-based flap is not protected from back-flow, conjunctival flap elevation and movements resulting from the fluid-jet may be clearly seen. Therefore, protective measures were taken to prevent the conjunctival flap from contact with MMC during application and irrigation. The tendency for relatively low incidence of mid-term vascularized vs ischemic, cystic bleb appearance between the current study and the older series with fornix-based flaps may probably be explained, at least in part, by that dual protective approach from MMC touch and the further awareness of avoiding the internal wall of the due filtering bleb from mechanical injury. It is possible that bleb protection was not complete or suffices in the two eyes in which thin bleb (patient 4) or some thick para-limbal cysts (patient 10) emerged during follow-up. A prospective controlled study with a larger series is required to verify that issue. Of interest is that Jones et al27 are cautious in protecting the conjunctival edges intraoperatively. The antimetabolite sponge is applied under the conjunctival flap, and specially designed clamps are used to protect the conjunctival edges from touch with that sponge. In this way, healing of the edges is not inhibited postoperatively. In the present study, a Weck cell sponge was used to protect both the conjunctival edges and the substantia propria.
Susanna et al5 report intraoperative treatment in primary trabeculectomies using 0.25 mg/ml MMC for 3 min on 15 eyes. The MMC Weck cell was applied over the episclera, without conjunctival and Tenon's capsule touch. At 12 months postoperatively, the mean IOP was 14.9 mm Hg with or without hypotensive medications, and the filtering bleb was elevated, thin and avascular in 12 eyes (80%). It was concluded that the mode of application was ineffective in eliminating the development of thin, avascular blebs in eyes that undergo primary trabeculectomy using limbal-based flaps. However, that was a limbal-based approach, and the injury to the exposed substantia propria during surgical manipulation followed the injury during MMC washout, could probably be critical.
Another theory on the progression of the filtering bleb to become cystic is the creation of a fibrotic ring, or ‘a ring of steel’,27 that develops between the ischemic site of the filtering bleb and the vascularized site, which is usually located distal to the ischemic one. According to the hypothesis, the ‘ring of steel’ prevents a further distal aqueous flow. The ischemic site is therefore exposed to an increased intra-bleb pressure, which might cause progressive bleb thinning and leakage. However, if this is the case, the IOP should also be high. However, the IOP in eyes with high cystic MMC-blebs is commonly normal or in the low teens, and an increased IOP does not precede, as a rule, the oozing or leaking event.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11
During the first postoperative phase, leakage from the wound site (Seidel test) was not detected in any of the eyes in the current study. This is similar to others that use the tunnel approach,15, 16, 17, 18, 19, 20 but in contrast to studies in which the standard trabeculectomy was used with a fornix-based conjunctival flap.17, 24, 25, 26 The difference may be attributed to the tunnel approach, lack of scleral radial incisions and the short and tight closure of the conjunctival flap, as previously discussed.15
This pilot study provides information regarding the association of protection of the inner wall of the fornix-based conjunctival flap from MMC contact during tunnel-trabeculectomy with a vascularized, thick bleb after 24–32 months of follow-up. Further controlled prospective studies are required to consolidate the association of protective measures from MMC touch on the prevention of late thin, avascular, cystic bleb formation and its consequences.
References
Bindlish R, Condon GP, Schlosser JD et al. Efficacy and safety of mitomycin-C in primary trabeculectomy: Five-year follow-up. Ophthalmology 2002; 109: 1336–1341.
DeBry PW, Perkins TW, Heatley G et al. Incidence of late-onset bleb-related complications following trabeculectomy with mitomycin. Arch Ophthalmol 2002; 120: 297–300.
Hu CY, Matsuo H, Tomita G et al. Clinical characteristics and leakage of functioning blebs after trabeculectomy with mitomycin-C in primary glaucoma patients. Ophthalmology 2003; 110: 345–352.
Jampel HD, Quigley HA, Kerrigan-Baumrind LA et al. Risk factors for late-onset infection following glaucoma filtration surgery. Arch Ophthalmol 2001; 119: 1001–1008.
Susanna Jr R, Costa VP, Malta RF et al. Intraoperative mitomycin-C without conjunctival and Tenon's capsule touch in primary trabeculectomy. Ophthalmology 2001; 108: 1039–1042.
Casson R, Rahman R, Salmon JF . Long term results and complications of trabeculectomy augmented with low dose mitomycin C in patients at risk for filtration failure. Br J Ophthalmol 2001; 85: 686–688.
Matsuo H, Tomidokoro A, Suzuki Y et al. Late-onset transconjunctival oozing and point leak of aqueous humor from filtering bleb after trabeculectomy. Am J Ophthalmol 2002; 133: 456–462.
Kim YY, Sexton RM, Shin DH et al. Outcome of primary phakic trabeculectomies without versus with 0.5- to 1-minute versus 3- to 5-minute mitomycin C. Am J Ophthalmol 1998; 126: 755–762.
Greenfield DS, Liebmann JM, Jee J, Ritch R . Late-onset bleb leaks after glaucoma filtering surgery. Arch Ophthalmol 1998; 116: 443–447.
Mochizuki K, Jikihara S, Ando Y et al. Incidence of delayed onset infection after trabeculectomy with adjunctive mitomycin C or 5-fluorouracil treatment. Br J Ophthalmol 1997; 81: 877–883.
Wells AP, Cordeiro MF, Bunce C, Khaw PT . Cystic bleb formation and related complications in limbus- versus fornix-based conjunctival flaps in pediatric and young adult trabeculectomy with mitomycin C. Ophthalmology 2003; 110: 2192–2197.
Parrish R, Minckler D . ‘Late endophthalmitis’ – filtering surgery time bomb? Ophthalmology 1996; 103: 1167–1168.
Smith S, D'Amore PA, Dreyer EB . Comparative toxicity of mitomycin C and 5-fluorouracil in vitro. Am J Ophthalmol 1994; 118: 332–337.
Cairns DE . Trabeculectomy – a preliminary report of a new method. Am J Ophthalmol 1968; 66: 673–679.
Ophir A, Pikkel J . Mini-trabeculectomy in eyes with high-risk of scarring – mid-term follow-up. Am J Ophthalmol 2001; 131: 131–138.
Lai JS, Lam DS . Trabeculectomy using a sutureless scleral tunnel technique: a preliminary study. J Glaucoma 1999; 8: 188–192.
Gherghel D, Orgul S, Prunte C, Flammer J . Trabeculectomy with a scleral tunnel technique combined with mitomycin C. In: Orgul S, Flammer J (eds). Pharmaco-therapy in glaucoma. Verlag Hans Huber: Bern, 2000, pp 243–250.
Vuori ML, Viitanen T . ‘Scleral tunnel incision’- trabeculectomy with one releasable suture. Acta Ophthalmol scand 2001; 79: 310–314.
Wang KH, Zhang CH, Wang GJ . Trabeculectomy with crescent tunnel knife under surface anesthesia for glaucoma: report of 41 cases. Di Yi Jun Yi Da Xue Xue Bao (China) 2003; 23: 560–561.
Kano K, Kuwayama Y, Mizunoya H . Clinical results of fornix-based trabeculectomy with a scleral tunnel. Nippon Ganka Gakkai Zasshi (Japan) 2005; 109: 75–82.
Cantor LB, Mantravadi A, WuDunn D, Swamynathan K, Cortes A . Morphologic classification of filtering blebs after glaucoma filtration surgery: The Indiana Bleb Appearance Grading Scale. J Glaucoma 2003; 12: 266–271.
Ophir A, Wasserman D . 5-Fluorouracil-needling and paracentesis through the failing filtering bleb. Ophthalmic Surg Lasers 2002; 33: 109–116.
Anand N, Arora S, Clowes M . mitomycin C augmented glaucoma surgery: evolution of filtering bleb avascularity, transconjunctival oozing and leaks. Br J Ophthalmol 2006; 90: 192–197.
Traverso CE, Tomey KF, Antonios S . Limbal- vs fornix-based conjunctival trabeculectomy flaps. Am J Ophthalmol 1987; 104: 28–32.
Brinckler P, Kessing SV . Limbus-based versus fornix-based conjunctival flap in glaucoma filtering surgery. Acta Ophthalmol (Copenhagen) 1992; 70: 641–644.
el Sayyad F, el-Rashood A, Helal M et al. Fornix-based versus limbal-based conjunctival flaps in initial trabeculectomy with postoperative 5-fluorouracil: four-year follow-up findings. J Glaucoma 1999; 8: 124–128.
Jones E, Clarke J, Khaw PT . Recent advances in trabeculectomy technique. Curr Opin Ophthalmol 2005; 16: 107–113.
Author information
Authors and Affiliations
Corresponding author
Additional information
We declare that we have no financial or proprietary interest in any material, product or company mentioned in this paper.
Rights and permissions
About this article
Cite this article
Ophir, A., Karatas, M. Protection of the conjunctival flap from contact with mitomycin C during tunnel-trabeculectomy. Eye 21, 1395–1402 (2007). https://doi.org/10.1038/sj.eye.6702462
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702462