Abstract
Background
A number of authors have documented the decrease in the rate of glaucoma drainage surgery, felt to be owing to increased medical therapy options. There has also been an increase in cataract extraction. The aim of this study was, using the NHS Hospital Episode Statistics (HES), to attempt to confirm these trends and to examine the possibility that these trends are not necessarily independent.
Methods
The HES was accessed for the main glaucoma procedures between 1998 and 2004 and for cataract operations performed over the same time period. Diagnostic data were also extracted from the HES data for glaucoma. Figures for the changes in glaucoma medications were obtained from pharmaceutical data.
Results
Over the period that the data are available, trabeculectomy numbers have reduced by 51%, laser trabeculoplasty by 60%, and laser peripheral iridectomy (PI) by 30%. Cataract extractions have increased by 52%. Medical treatments, especially prostaglandin use, have increased. The number of admissions for acute glaucoma did not increase.
Conclusions
The figures indicated a decrease in glaucoma drainage surgery and an increase in cataract extraction—consistent with other studies. More surprisingly, there was no increase in diagnosis of angle closure glaucoma or laser PIs within the figures and we suggest this may in part be related to the increase in cataract extraction. We speculate that this may also partly be responsible for the reduction in trabeculectomies. Although the HES data are a potentially rich source of information, there are potential inaccuracies in the data, which means interpretations must be made with caution.
Similar content being viewed by others
Introduction
We have observed with others an apparent fall in the frequency of surgical interventions for glaucoma over recent years.1, 2, 3, 4, 5 This has been attributed by some to the introduction of a range of new medications for lowering intraocular pressure (IOP) but we hypothesise that there may have been additional influences—in particular that the increasing cataract surgical rate (which has nearly doubled in the last few years) may have had an impact on glaucoma surgery. This may be restricted to acute and chronic angle closure disease but may also influence open angle disease.
The purpose of this paper is to ascertain if there is any evidence for this hypothesis within NHS activity statistics. At the same time, we wish to try to determine whether these routinely collected data are sufficiently reliable to enable an examination of the possible relationship between cataract surgical activity and glaucoma episodes.
The UK Department of Health publishes a measure of NHS activity via their Hospital Episode Statistics (HES). HES is the national statistical data warehouse for England, representing the care provided by NHS hospitals and for NHS hospital patients treated elsewhere (eg within private hospitals). There is a large amount of data available within the HES—in the financial year 2003/2004, this involved over 13 million records detailing episodes of admitted patient treatment delivered by NHS hospitals in England. Clinical information on diagnosis and procedures is captured for in-patients and day cases, but not for outpatient attendances. The clinical data are identified and coded from medical records, following the discharge of a patient from an in-patient or day-case episode.
There are various categories of data available within the HES, but of particular interest is the data regarding the ‘Primary Diagnosis’ of all admissions and ‘Main Operations’ (defined by the HES as the first recorded performed during that admission). The diagnostic codes are taken from the International Classification of Diseases, tenth revision (ICD10) whereas the operative codes are from the Office of Population Censuses and Surveys tabular list of surgical operations and procedures, fourth revision (OPCS4).
HES records describe episodes (periods) of continuous admitted patient care under the same consultant. Within the broad categories of Primary Diagnosis and Main Operations, data can be accessed at different levels. Primary Diagnosis episodes are grouped by the less specific three-digit ICD10 codes and by a more detailed four-digit primary diagnosis. Similarly, for the Main Operations, episodes can either be accessed from the three-digit OPCS4 codes or more detailed four-digit code.
The HES database is assembled from records originally generated by the patient administration systems within over 300 separate NHS Trusts. The HES authors themselves admit that no matter how carefully the data are gathered, it is inevitable in such a complex undertaking that a few errors will occur. The data do however remain the largest data set of their kind in the UK (coverage and completeness of over 96% of England) and have been validated by a number of studies.6, 7
Methods
The HES was accessed and the episode statistics noted for the main glaucoma procedures (indicated in Table 1)—the data have only been collected in this format since 1998/99 and the latest data set are 2003/04. The number of cataract operations performed were also accessesed.
One of the problems with some of the HES data set is the presence of a number of different data sets for essentially the same operation (eg C71.1 ‘Extracapsular extraction of lens, Simple linear extraction of lens’ whereas C71.2 is ‘Extracapsular extraction of lens, Phakoemulsification of lens’ and C71.9 Extracapsular extraction of lens, Unspecified’). For this reason, we took ‘Prosthesis of lens (C75)’ as an estimate of the numbers of cataracts performed that year. This seemed reasonable as it is likely that there would only be a small number of cataract extractions without an intraocular lens (IOL) being implanted and conversely, relatively few patients now undergo secondary IOL insertions. Further, when looking at the three-digit ‘Primary Diagnosis’ data for cataract, the numbers are similar to those given for IOL implantation.
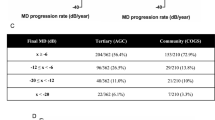
We also looked at the data within the ‘Primary Diagnosis’ category. The three-digit entry for glaucoma (H40–H42) is shown in Table 3. When the four-digit entries are examined, there are a number of categories for glaucoma—many of which could overlap. The category that is likely to be most diagnostically accurate is that for the total number of admissions for primary angle closure glaucoma (PACG) and these are also shown in Table 3.
The HES do not contain data in relation to medical treatment or prescriptions and as these represent an essential treatment tool within glaucoma practice we felt it was also important to look at any changes over the last 5 years. We were kindly provided by Pfizer® pharmaceuticals drug data extracted from their own analysis of the glaucoma medications market.
Results
The data extracted from the HES (except medical treatment) can all be accessed at http://www.hesonline.nhs.uk.8 Table 1 represents the overall changes in medical and surgical treatments from 1998 to 2004. The last two rows in Table 1 summarise the changes over this time. Table 2 compares the change in the total number of prescriptions for glaucoma with the changes in the use of topical prostaglandins from 1998 to 2004. Finally, Table 3 is extracted from the Primary Diagnosis data and indicates the changes in ‘admissions’ for glaucoma (three-digit) and those for PACG (four-digit) and for the number of emergency admissions for PACG.
It can be seen in Table 1 that there is an obvious increase in the prescription of glaucoma medications from 1998 to 2004. The lower row shows this increase to be 18%, with Table 2 indicating that coincident with this is a huge increase in the number of prostaglandins prescribed (793%). In 1998, prostaglandins were less than 10% of all medications prescribed but by 2004 were nearly 50%.
Table 1 also shows that the number of trabeculectomies has decreased year on year from 8622 in 1998–1999 to 4206 in 2003–2004. This represents a drop of 51%. Similarly, laser procedures for glaucoma decreased over the same time period with a drop of over 30% for laser peripheral iridectomy (although interestingly surgical peripheral iridectomy (PIs) have remained constant) and laser trabeculoplasty reducing by 60%. Cyclodiode laser has increased by 80% between 1998 and 2004—although this does in fact only represent an actual increase in procedures of 500 cases.
Although not shown in the table, tube surgery numbers changed only slightly between 1998 and 2004 with an increase from 112 in 1998 to a maximum of 210 in 2002–2003 and dropping to 161 in 2003–2004.
Table 1 indicates the large increase in the numbers of cataract extracted and lens implantation over the time period. Whereas there were 191 540 operations performed in 1998–1999 by 2003–2004, this had increased by nearly 100 000 to 291477—an increase of over 50%.
Table 3 is from a different data set within the HES dealing with diagnosis and admissions. From this, it can be seen that the number of patients admitted with angle closure has remained roughly constant over the period the data are available for.
Discussion
It has been recognised for some years that the number of trabeculectomies being performed1, 2, 3, 4, 5 has been steadily decreasing and this is shown by the HES data. This is in contrast to the exponential increase in use of prostaglandins over the last 8 years, which might support the suggestion of a causal relationship between the two observations.
The increase in the cataract surgical rate is well documented by the data. A number of factors may explain this:
-
increasing demand of an ageing population with greater health expectations;
-
an improved safety profile allowing earlier surgery to be considered;9
-
an increased number of ophthalmologists in the UK; and
-
government targets to reduce waiting times for cataract surgery.
As far as laser surgery is concerned, there appears to have been a steady decrease in laser trabeculoplasty. There has also been a steady increase in the number of cyclodiodes being performed—this presumably reflects their ease of use and efficacy in reducing the IOP, especially in eyes resistant to other therapies. The increase in numbers may also reflect the fact that the IOP-lowering effect may be temporary and the laser needs repeating. It is important to treat the laser figures with care. Many lasers are carried out as outpatient procedures (YAG laser PIs, laser trabeculoplasty, and sometimes cyclodiode laser) and it is possible that not all these procedures are coded.
Tube surgery did increase from 1998 to 2004 (by 49). Although the percentage changes are relatively large, the overall numbers are small and unlikely to account for the decrease in the number of trabeculectomies being performed.
If the figures are reasonably accurate there is an apparent reduction in the number of peripheral iridotomies being performed (30% between 1998 and 2004). This is perhaps surprising, as with an ageing population10 it may be expected that more iridectomies would be needed as anterior chamber depth reduces with age and as the lens grows bigger.11 In keeping with this, from the diagnostic section of the HES data, the number of patients presenting with acute angle closure glaucoma has stayed almost the same between 1998 and 2004. A possible common explanation for these findings is the increase in cataract extractions. Most patients presenting with ACAG have lens-related disease and it may be that because of the increase in cataract extraction and at a younger age, patients who would have gone on to suffer ACAG do not because their lens has already been extracted.
To add weight to this argument, the HES data with regard to cataract extraction contain the age ranges of patients undergoing the surgery. Despite the fact that there are an increasing number of the general population in the older age groups, the average age of those undergoing cataract surgery has remained unchanged from 1998 to 2004 at 75 years of age. This could suggest that the increased recruitment to the older age group (75+) is balanced by an increasing number of operations being performed in those under 75.
To extrapolate this further, it is also possible that the reduction in the number of trabeculectomies being performed is partly related to the increase in the number of cataract extractions. If a patient who was developing chronic angle closure had a cataract extraction (either for visual or pressure reasons), this may be enough to prevent a continued increase in pressure and therefore avoid trabeculectomy. Even patients who are labelled ‘openangle’ glaucoma can have a degree of angle narrowing (or indeed develop it as the years go by) and some of them may inadvertently be ‘saved’ from drainage surgery by removal of a coexisting cataract. Previous authors have illustrated the decline in trabeculectomy surgery rates by comparing the numbers to the increase in cataract surgery. We suggest that it is possible these trends may not be independent variables and that the vast increase in the rate of cataract surgery may partly be responsible for the decline in the rate of trabeculectomies (as well as the introduction of new medications also shown).
It is of course important to look for flaws/biases in the data that may give alternative explanations for the results discussed:
-
Changes in the methods of collecting and classifying the data. This is explicitly stated in the foreword to the HES data. ‘Fluctuations can occur for a number of reasons, for example, organisational changes, reviews of best practice within the medical community, the adoption of new coding schemes, and data quality problems that are often year specific. These variations can lead to false assumptions about trends’. However, there is no evidence that the codings or diagnostic categories have changed during the period that the data are available.
-
The data itself is only as good as the accuracy of input. The variations in the diagnostic data for all glaucomas shown by the HES are a good example of the care that needs to be taken when attempting to interpret the data. Generally speaking, the absolute numbers represented within the HES data are probably of less use than the trends in treatment changes that they indicate. As discussed above, certain procedures, for example, YAG PI, may be performed but are not always coded. There have been a number of attempts to validate the HES data, which has resulted in questioning of the data. These studies have shown a variation in coding of the data at an individual department/hospital level7, 12 and it is important to bear in mind when analysing any study that utilises HES statistics that this variation can account for some (or all) of the results. The large amount of data and its geographical coverage are potentially very useful but there needs to be continuing assessment of accuracy to ensure questions regarding the validity of conclusions drawn from the data can be answered.
-
Changes in therapies for conditions that are not classified by the HES. There have been some changes over the study period such as deep sclerectomy and viscocanolostomy, but as the numbers of these being performed in the UK are still relatively small, it is unlikely they had a major contribution to the reduction in trabeculectomy numbers. It is however possible that they did have some contribution.
-
Similarly, the popularity of phacotrabeculectomy may have had some influence on the data and it is difficult to know how they were classified. If phacotrabs were classified as both procedures (trabeculectomy and cataract extraction) or as trabeculectomy alone, this would not change the findings (apart from slightly fewer cataracts with the latter). If however phacotrabs were classified as cataracts and not trabs, this would make the overall number of trabs appear less. Presumably however, this misclassification would be consistent throughout the data period and, unless the number of phacotrabs increased markedly between 1998 and 2004 (which from our experience they have not), the relative decrease in the number of trabeculectomies would be maintained.
-
Other changes in the data that may have an influence, for example, the increase in cyclodiodes is also unlikely to explain the drop in trabeculectomies—although it can temporarily reduce IOP, it is unlikely to replace drainage surgery in the long-term.
As mentioned above, the HES is a rich source of data but has potential flaws. The strength of the data is its size and it is the largest database of NHS activity available. Although we cannot draw any definitive conclusions because of possible inconsistencies in data collection, our observations of the data are interesting and should at least be an incentive to improving the quality of routinely collected information on hospital activity.
Within this current study, it is important to realise that the data relating to the prostaglandin use are from company data and are therefore from a source different from that of the HES data. Again, the trends within the data are probably more important than the actual numbers.
Conclusion
Within the cautions described, the observed figures are broadly in agreement with other studies indicating a decreasing number of trabeculectomies being performed as compared to a big increase in cataract surgery.
The decrease in trabeculectomy rate may be due to a number of factors—including a greater choice of more effective medications, earlier diagnosis, or other changes we are not aware of. It is also possible that the increase in the number of cataract extractions is partly responsible for the decrease in trabeculectomy surgery. This concept is given credence from the fact there has been a minimal change in patients attending with PACG but there has been no increase in the number of PIs.
Finally, although the HES data are a potentially rich source of information, it is important to recognise the limitations of data sets represented in this paper and to be careful in the conclusions drawn. This vast set of data can only be made more accurate by the involvement of clinicians in the coding process.7
References
Paikal D, Yu F, Coleman AL . Trends in glaucoma surgery incidence and reimbursement for physician services in the Medicare population from 1995 to 1998. Ophthalmology 2002; 109(7): 1372–1376.
Bateman DN, Clark R, Azuara-Blanco A, Bain M, Forrest J . The impact of new drugs on management of glaucoma in Scotland: observational study. BMJ 2001; 323: 1401–1402.
Walland MJ . Glaucoma treatment in Australia: changing patterns of therapy 1994–2003. Clin Exp Ophthalmol 2004; 32(6): 590–596.
Long VW, O'Brien CJ . Trends in ophthalmic surgery in Ireland. Ir J Med Sci 2005; 174(2): 36–39.
van der Valk R, Schouten JS, Webers CA, Beckers HJ, van Amelsvoort LG, Schouten HJ et al. The impact of a nationwide introduction of new drugs and a treatment protocol for glaucoma on the number of glaucoma surgeries. J Glaucoma 2005; 14(3): 239–242.
Lakhani A, Coles J, Eayres D, Spence C, Rachet B . Creative use of existing clinical and health outcomes data to assess NHS performance in England: Part 1—performance indicators closely linked to clinical care. BMJ 2005; 330: 1426–1431.
Williams JG, Mann RY . Hospital episode statistics: time for clinicians to get involved? Clin Med 2002; 2(1): 34–37.
Hospital Episode Statistics (HES). http://www.hesonline.nhs.uk, accessed 15 March 2006.
Jampel RS . The effect of technology on the indications for cataract surgery. Doc Ophthalmol 1999; 98(1): 95–103.
UK Government National Statistics. Distribution of population by age. Found at:http://www.statistics.gov.uk/cci/nugget.asp?ID=949, accessed 15 March 2006.
Bourne RR, Alsbirk PH . Anterior chamber depth measurement by optical pachymetry: systematic difference using the Haag–Streit attachments. Br J Ophthalmol 2006; 90(2): 142–145.
Croft GP, Williams JG . The RCP information laboratory (iLab): breaking the cycle of poor data quality. Clin Med 2005; 5(1): 47–49.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fraser, S., Wormald, R. Hospital Episode Statistics and changing trends in glaucoma surgery. Eye 22, 3–7 (2008). https://doi.org/10.1038/sj.eye.6702458
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702458
Keywords
This article is cited by
-
Trabeculectomy training in England: are we safe at training? Two year surgical outcomes
Eye (2018)
-
Does the intraocular pressure-lowering effect of prostaglandin analogues continue over the long term?
International Ophthalmology (2017)
-
Global rates of glaucoma surgery
Graefe's Archive for Clinical and Experimental Ophthalmology (2013)
-
Surveillance of late-onset bleb leak, blebitis and bleb-related endophthalmitis — a UK incidence study
Graefe's Archive for Clinical and Experimental Ophthalmology (2012)
-
Changes in intraocular pressure and anterior segment morphometry after uneventful phacoemulsification cataract surgery
Eye (2010)