Abstract
Aim
We report the incidence, causes, characteristics, and the outcome of traumatic corneal graft ruptures in a tertiary referral centre in the UK.
Method
A retrospective analysis of all graft ruptures secondary to trauma that were treated at our centre between 1999 and 2005 was undertaken. Statistical analysis of possible prognostic factors was undertaken using the Fisher's test.
Results
Nineteen eyes in 18 patients sustained eye trauma resulting in graft rupture (median age of 53 years; range 27–82; 15 men and four women). Seventeen cases were accidental and two were from violence. The median time interval between grafting and rupture was 8.3 months (range 3 days to 15 years). The 6-year incidence was 3.8%. All graft ruptures occurred at the host–graft junction and ranged from 45 to 270°. Iris prolapse/loss was noticed in 89% and lens loss in 53%. The most common posterior segment complication was vitreous loss (74%), followed by vitreous haemorrhage (32%) and retinal detachment (21%). Grafts with 180° or more of dehiscence were more likely to fail (P<0.001), had more extensive posterior segment damage, and a poorer visual outcome. Grafts without sutures had a more extensive dehiscence (P<0.01). Final visual acuity was worse than 6/60 in 58%.
Conclusions
The risk of traumatic corneal graft rupture is significant and is associated with a poor visual outcome. This fact needs to be clearly emphasised during preoperative counselling and protective measures encouraged.
Similar content being viewed by others
Introduction
Any globe is susceptible to rupture and will do so at its weakest point if subject to sufficient force. Postoperatively, corneal scars are unlikely to regain the original preinjury strength, and remain vulnerable to spontaneous and traumatic dehiscence.1, 2, 3, 4, 5, 6, 7, 8 Studies have reported the incidence and outcome of corneal traumatic graft ruptures in other countries.7, 8, 9, 10, 11, 12, 13, 14 However, this problem has not been adequately highlighted in the UK.15
In this paper, we report the incidence and outcome of traumatic graft ruptures in a tertiary referral centre in the UK. We have examined the causes of traumatic corneal graft ruptures and the long-term visual outcome in patients with ruptured corneal grafts on prolonged follow-up. This study represents the largest European series to date.
Patients and methods
A retrospective analysis was undertaken of patients with corneal graft ruptures treated at the Tennent Institute of Ophthalmology over a 6-year period from 1999 to 2005. In total, 19 eyes in 18 patients who had sustained graft ruptures required surgical repair. The approval of the local research committee was sought and obtained. All 19 eyes had their corneal graft at our Institute. During that time, one patient who had her graft performed elsewhere presented with a corneal graft rupture. This patient was excluded from our study. Not available are patients who had their corneal grafts at our institute, who had moved away and who may have presented elsewhere with corneal graft ruptures. The case notes of all patients were reviewed. No case was lost to follow-up and case notes were generally detailed in their descriptions of the injury and findings. Wherever possible, the best-corrected visual acuities were recorded. Between the years 1999 and 2005, 342 patients (178 men and 164 women) with ages ranging from 16 to 89 years (median 63 years) had corneal grafts performed in the department. This figure was used to calculate the ‘centre’ incidence of graft ruptures.
The statistical significance of various risk factors such as the original indication for grafting, sex of the patient, extent of the wound dehiscence, the time interval between trauma and grafting, and their influence on graft survival were determined using Fisher's exact test with a two-tailed P-value based on the method of summing small P-values.
Results
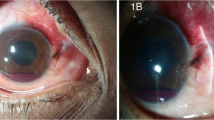
There were 14 male and 4 female patients, age ranging from 27 to 82 years (median 53 years). The indications for grafting were keratoconus (11 patients; two eyes in one patient), corneal scarring (3 patients), and Fuch's endothelial dystrophy (4 patients). Corneal grafts were performed using interrupted 10/0 nylon sutures (18 patients) and continuous 10/0 nylon sutures (one patient). At the time of trauma, sutures had been removed in five patients. The incidence of corneal graft rupture for that 5-year period was 3.8%. The six patients who had their grafts performed before 1999 were excluded in this calculation. The time interval between corneal grafting and traumatic rupture ranged between 3 days and 15 years (median of 8.3 months). Seventeen graft ruptures (89.5%) were purely accidental and occurred while undertaking routine day-to-day activities (Table 1). One patient who was a drug abuser lost both his eyes owing to assault on two separate occasions (Figure 1).
Two patients developed glaucoma with one requiring trabeculectomy. The retinal detachments all occurred at least 2 weeks after graft rupture.
All graft ruptures occurred at the graft–host junction. Graft sutures were intact in 14 cases at the time of trauma. Of these cases, graft sutures were broken by trauma in 12 cases and loosened in two cases. Nine grafts remained clear (47.4%) and 10 failed (Table 2). Eight of the 10 failed grafts lost clarity owing to endothelial cell loss. The remaining two failed owing to late rejection. At the most recent follow-up, 11 grafts remained clear (57.9%). Various risk factors were analysed to see if they affected graft survival after rupture. No statistical significance was found when comparing sex, age, the original indication for grafting, or the time interval between grafting and trauma. All grafts with 180° or more of dehiscence lost clarity (P<0.01). In the five cases where sutures were removed before trauma, grafts had a more extensive dehiscence (P<0.01).
Visual acuities at most recent follow-up (best corrected) were worse than 6/60 in 11 patients, 6/60–6/24 in three patients (1/36 in one patient), and 6/18 or better in five patients (Table 2). Visual acuities were worse in 17 eyes, the same in one eye and better in one following rupture.
Discussion
Traumatic rupture of corneal grafts has a bad prognosis. At present in the United Kingdom, the extent of this problem has not been adequately highlighted. In a previous study that evaluated the success rate of keratoconus, Kirkness et al15 found four cases of rupture among 198 grafts analysed. However, this study did not highlight the outcome of trauma to corneal grafts. The only major European study was reported from Germany over 9 years ago by Rohrbach et al.16 The reported incidence of traumatic graft rupture in other countries varied from 0.6 to 5.8% (Table 3).
Corneal wounds almost never regain the original strength of the original graft even several years after meticulous repair.1, 2, 3, 4, 5, 6 Wound healing is slower in central corneal wounds compared to peripheral corneal wounds.17 During the first few days after corneal wound repair, the integrity of the corneal wound depends entirely on the suture material. Animal experiments suggest only 6.5% of the wound strength is regained in the first 7-day period.18 In human limbal wounds, no fibrovascular tissue is observed in the first 5 days and the wound depends completely on the corneal sutures for its strength for up to 14 days. Deposition and reorganisation of collagen is required for the wounds to acquire tensile strength and sutured limbal wounds take 6 months for the wounds to gain 70% of the original strength.17 However, spontaneous wound dehiscence of up to 7.2% has even been reported 24 months after surgery following suture removal.19 Factors that impair corneal wound healing following penetrating keratoplasty include the prolonged use of topical corticosteroids and the presence of a much larger wound that is more distant from the corneal limbus.
In our series and other reported studies, the first year after grafting was the most vulnerable period to traumatic dehiscence (Figure 2). The highest risk period for graft rupture was in the first postoperative month. This gradually declines over the next 18 months and this time is a moderate risk period.10 However, suture removal weakens the wound integrity and the second most important high-risk period is after removal of graft sutures. In our patients, the grafts with intact sutures tended to have a smaller degree of dehiscence. Corneal sutures may still play a role in maintaining the integrity of the host–graft junction even after several years and leaving the sutures may protect against dehiscence.
Traumatic graft rupture results in a wide range of injuries that include damage to the endothelium leading to graft failure, iris prolapse, extrusion of crystalline lens, vitreous loss at the time of injury, delayed retinal detachment, choroidal haemorrhage, and total disruption of intraocular contents. Retinal detachment and posterior segment complications were an important cause of total loss of vision.13 Grafts with a larger extent of dehiscence were associated with a higher likelihood of posterior segment damage and a poorer final visual outcome. Graft failure owing to primary endothelial damage with late failure is a common finding and the incidence may be as high as 77%.12, 20 In our study, the grafts with a larger degree of dehiscence were not only more likely to fail but were also more likely to have lost clarity at first presentation. The final visual outcomes in our patients were better than previously reported figures.9, 10, 12, 13, 16 Corneal sutures had not been removed in a larger proportion of our patients, and this could have limited the extent of the dehiscence with more trivial injuries. Rehany et al11 also found that intact sutures provided a degree of protection.
The risk of corneal graft rupture should be emphasised during preoperative counselling and should be reiterated during the follow-up. Many graft ruptures occur during normal daily activities that could be considered ‘low-risk activities’. In this study, we have identified the first year as the most vulnerable period as 53% of our graft ruptures occur during this period. Even trivial trauma can be devastating. Elder et al10 have recommended eye protection for 24 h for the first month after surgery and after suture removal. They also recommend that eye protection should be worn while awake for 6 months after grafting and also after suture removal. Eyewear should be worn forever during low-risk activities, and high-risk activities like boxing and contact sports should be avoided altogether.10 The extent of visual loss could have been reduced in our patients if protective eyewear had been in place. However, compliance with protective eyewear can be poor.11 Patients with learning difficulties may be at an increased risk of graft rupture. Patient 17 had learning difficulties and suffered corneal graft ruptures in both his eyes owing to physical violence on separate occasions.
In summary, the risk of traumatic corneal graft rupture is significant and carries a bad visual outcome. This should be clearly emphasised during preoperative counselling and patients should constantly be reminded of the risk. Eye protection during vulnerable periods may limit visual loss.
References
Artola A, Ayala MJ, Ruiz-Moreno JM, De La Hoz F, Alio JL . Rupture of radial keratotomy incisions by blunt trauma 6 years after combined photorefractive keratectomy/radial keratotomy. J Refract Surg 2003; 19(4): 460–462.
Behl S, Kothari K . Rupture of a radial keratotomy incision after 11 years during clear corneal phacoemulsification. J Cataract Refract Surg 2001; 27(7): 1132–1134.
Bloom HR, Sands J, Schneider D . Corneal rupture from blunt trauma 22 months after radial keratotomy. Refract Corneal Surg 1990; 6(3): 197–199.
Budak K, Friedman NJ, Koch DD . Dehiscence of a radial keratotomy incision during clear corneal cataract surgery. J Cataract Refract Surg 1998; 24(2): 278–280.
Hurvitz LM . Late clear corneal wound failure after trivial trauma. J Cataract Refract Surg 1999; 25(2): 283–284.
Lee BL, Manche EE, Glasgow BJ . Rupture of radial and arcuate keratotomy scars by blunt trauma 91 months after incisional keratotomy. Am J Ophthalmol 1995; 120(1): 108–110.
Raber IM, Arentsen JJ, Laibson PR . Traumatic wound dehiscence after penetrating keratoplasty. Arch Ophthalmol 1980; 98(8): 1407–1409.
Maheshwari S, Saswade M, Thool A . Traumatic wound dehiscence 14 years following penetrating keratoplasty. Indian J Ophthalmol 2003; 51(3): 259–260.
Agrawal V, Wagh M, Krishnamachary M, Rao GN, Gupta S . Traumatic wound dehiscence after penetrating keratoplasty. Cornea 1995; 14(6): 601–603.
Elder MJ, Stack RR . Globe rupture following penetrating keratoplasty: how often, why, and what can we do to prevent it? Cornea 2004; 23(8): 776–780.
Rehany U, Rumelt S . Ocular trauma following penetrating keratoplasty: incidence, outcome, and postoperative recommendations. Arch Ophthalmol 1998; 116(10): 1282–1286.
Tseng SH, Lin SC, Chen FK . Traumatic wound dehiscence after penetrating keratoplasty: clinical features and outcome in 21 cases. Cornea 1999; 18(5): 553–558.
Oshry T, Lifihitz T . Traumatic wound dehiscence after corneal graft. Ophthalmic Surg Lasers 2001; 32(6): 470–473.
Bowman RJ, Yorston D, Aitchison TC, McIntyre B, Kirkness CM . Traumatic wound rupture after penetrating keratoplasty in Africa. Br J Ophthalmol 1999; 83(5): 530–534.
Kirkness CM, Ficker LA, Steele AD, Rice NS . The success of penetrating keratoplasty for keratoconus. Eye 1990; 4(Part 5): 673–688.
Schlote T, Rohrbach M . Traumatic glaucoma—a survey. Klin Monatsbl Augenheilkd 2005; 222(10): 772–782.
Gasset AR, Dohlman CH . The tensile strength of corneal wounds. Arch Ophthalmol 1968; 79(5): 595–602.
Gliedman ML, Karlson KE . Wound healing and wound strength of sutured limbal wounds. Am J Ophthalmol 1955; 39(6): 859–866.
Abou-Jaoude ES, Brooks M, Katz DG, Van Meter WS . Spontaneous wound dehiscence after removal of single continuous penetrating keratoplasty suture. Ophthalmology 2002; 109(7): 1291–1296 (discussion 1297).
Watson AP, Simcock PR, Ridgway AE . Endothelial cell loss due to repeated traumatic wound dehiscence after penetrating keratoplasty. Cornea 1987; 6(3): 216–218.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests: None declared.
Rights and permissions
About this article
Cite this article
Lam, F., Rahman, M. & Ramaesh, K. Traumatic wound dehiscence after penetrating keratoplasty—a cause for concern. Eye 21, 1146–1150 (2007). https://doi.org/10.1038/sj.eye.6702407
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702407