Abstract
Aims
To study risk factors for presumed infectious endophthalmitis complicating cataract surgery in the United Kingdom.
Methods
Two hundred and fourteen clinically diagnosed patients with presumed infectious endophthalmitis were compared with 445 control patients throughout the United Kingdom in a prospective case–control study. The cases were identified through the British Ophthalmological Surveillance Unit reporting card system. Control patients undergoing cataract surgery from 13 ‘control centres’ throughout the United Kingdom were selected randomly. Risk factors were identified by univariate and multivariate logistic regression analyses. Pertinent variables relating to the cataract extraction procedure, antimicrobial prophylaxis, ophthalmic and medical history were analysed with regard to postoperative infection.
Results
Statistically significant risk factors in the multivariate model included inpatient cataract surgery (P=0.001), surgery in dedicated eye theatres (P<0.001), consultant grade surgeon (compared to registrar) (P=0.001), posterior capsule tear during cataract surgery (P=0.001). The use of face masks by the scrub nurse and surgeon during cataract surgery (P<0.001) and the administration of subconjunctival antibiotics at the end of surgery (P<0.001) were protective against postoperative infection.
Conclusions
In order to minimise the risk of postoperative endophthalmitis we would recommend the wearing of face masks by the surgeon and scrub nurse during cataract surgery and subconjunctival antibiotics at the end of surgery.
Similar content being viewed by others
Introduction
Endophthalmitis still remains one of the most dreaded complications of modern cataract surgery despite refinements in surgical technique and the use of prophylactic antibiotics. Owing to the relatively low incidence, it has been difficult to clearly identify those factors that lead to the development of endophthalmitis. Risk factors which have been identified by previous case–control studies include immunosuppressive treatment, wound abnormalities, intraoperative communication with the vitreous cavity, the use of intraocular lenses (IOL) without a heparinised surface and the use of lenses with polypropylene haptics.1, 2 These studies were conducted in America and Sweden at a time (between 1988 and 1993) when the majority of cataract extractions were performed by the extracapsular technique rather than by phacoemulsification.
This study investigated potential risk factors for endophthalmitis following modern cataract surgery in the UK, including the surgical technique employed, surgery with multiple use equipment, type of IOL implanted, intraoperative, and postoperative complications. Prophylactic methods to prevent endophthalmitis were also evaluated.
Methods
Cases
Information on 214 new cases of acute presumed infectious endophthalmitis (PIE) were identified prospectively by nationwide active surveillance through the British Ophthalmological Surveillance Unit (BOSU) reporting card system.3, 4
Case notification was requested for the 12-month study period between October 1999 and September 2000 inclusive. Acute-onset endophthalmitis was defined as any patient with a clinical diagnosis of PIE occurring within 6 weeks of cataract surgery. All combined procedures, cases of previous intraocular surgery and trauma were excluded. Detailed information pertaining to potential systemic, ophthalmic and operative risk factors, and also perioperative antimicrobial prophylaxis was collected from the reporting ophthalmologist using a standard questionnaire.4
Controls
Information on 445 control patients undergoing cataract surgery was prospectively collected using a standard format. ‘Control centres’ were selected by a clustered, stratified random sampling procedure. To ensure geographical spread of control centres, the UK was divided into nine regions. Within each region, hospitals were selected by applying computer-generated random numbers to a list of hospitals with the probability of selection proportional to the number of consultants per hospital. Twenty ‘control centres’ (approximately 10% of total UK units) in total were selected. Thirteen control centres agreed to participate in the study, from the following regions in the UK; Anglia and Oxford (one), North Thames (one), South Thames (one), South and West (three), North and West (two), Northern and Yorkshire (two), Trent and West Midlands (two), and Scotland (one).
Forty controls were selected from each of the 13 control centres by systematic sampling from a chronological list of patients who had cataract surgery performed between March 2000 and August 2000 inclusive. Seventy-five controls were excluded because they were incorrectly identified as having previous cataract surgery or because of incomplete case notes. The case notes were reviewed at least 6 months after cataract surgery to ensure that endophthalmitis had not developed during this postoperative time period. All combined procedures, cases of previous intraocular surgery, and trauma were excluded.
Data collection
Case data were obtained by the collection of completed questionnaires from reporting ophthalmologists throughout the UK. The information from the case notes of control patients was transferred directly onto a standard proforma by the study investigators.
The following variables were studied:
Preoperative data
Age, sex, history of diabetes, immunosuppression or systemic steroid use, and history of glaucoma.
Operative data
Surgeon grade (consultant, associate specialist, staff grade, registrar, senior house officer) daycase or in-patient surgery, surgery in dedicated or nondedicated eye theatres, type of anaesthesia, surgical technique, single use or reusable phaco needle and tubing, type of IOL, intraoperative and 1st day postoperative complications.
Prophylactic methods employed
Preoperative topical and systemic antibiotics, povidone iodine eyelid prep prior to surgery, operative antibiotics (in the irrigating solution or into the capsular bag), and topical or subconjunctival antibiotics/steroid at the end of surgery.
Patient details that may not have been routinely documented in the case notes, such as blepharitis and lacrimal drainage problems were not included in the proformas. The controls for this study were shared with another BOSU case–control study of ‘suprachoroidal haemorrhage complicating cataract surgery’.5 Two study investigators (SK and RL) visited the 13 control centres to retrieve data from the patient notes. The two investigators compared independently retrieved data from a single pilot centre to ensure standardisation of the data retrieval from the cases notes. Data collected from this centre was found to have 98.5% concordance.
Information from the cases and controls were subsequently transferred onto a database for analysis.
Data analysis
All statistical analyses were carried out using the computer package SPSS for windows. Univariate logistic regression analyses were performed to investigate the relationship between status (case or control) and each potential individual risk factor. Any variable whose univariate test had a P-value of 0.25 or less was included in the multivariate logistic modelling. A P-value of 0.25 was chosen to allow the introduction of potentially important variables into the final model as the use of a more traditional level (such as 0.05) often fails to identify variables known to be important.6
To maximise the degrees of freedom, variables with more than 15% missing data and those present in small numbers (<2%) were excluded from the multivariate analysis.6 Using a combination of forward and backward stepwise procedures, with probabilities of entry and removal of 0.05, respectively, a final multivariate model was obtained.
Results
Through the BOSU monthly reporting card system, partial or complete data were available on 214 patients presenting with PIE following cataract surgery (see previous publication for details regarding the presentation, management and outcome of cases of PIE).4 Data from 445 controls was collected from the 13 control centres. The mean age was 73.5 years for the cases (range 7–94) and 75 years for the controls (range 27–99).
Univariate analysis
Univariate analyses for discrete variables are presented in Table 1.
Strong risk factors for the occurrence of PIE included; inpatient cataract surgery (P=0.001), surgery performed in dedicated eye theatres (P<0.001), consultant grade of surgeon (P=0.003), and posterior capsule tear during cataract surgery (P<0.001).
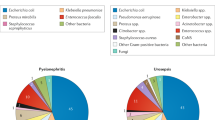
The use of face masks by surgeon and scrub nurse (P<0.001) and the use of subconjunctival antibiotics at the end of cataract surgery (P<0.001) were protective against the development of infection. Gentamicin and cefuroxime were the most commonly used subconjunctival antibiotics (Table 2).
A history of immunosuppression, conversion from phaco to ECCE, intraoperative and postoperative antibiotics, although significant in the univariate analysis were excluded from the multivariate analysis as they occurred in too small numbers for the controls (<2.0% of controls). The type of IOL haptic material was also excluded from the multivariate analysis as this variable was poorly documented in the data collection forms for the cases (data present in 151/214 (70.6%) cases).
Multivariate analysis
Risk factors chosen from the univariate analyses for inclusion in the multivariate analysis were: age, glaucoma, daycase surgery, dedicated theatre, surgeon grade, use of facemasks, preoperative antibiotic use, operated eye, surgical incision, single or multiuse phaco needle, IOL optic material, posterior capsule tear, use of antibiotics and steroids at the end of surgery.
Multivariate logistic regression modelling identified the following statistically significant risk factors for PIE following cataract surgery (Table 3): inpatient cataract surgery, surgery in dedicated eye theatres, consultant grade surgeon (compared to registrar), and posterior capsule tears during cataract surgery. The administration of subconjunctival antibiotics at the end of cataract surgery and the use of face masks by the surgeon and scrub nurse in theatre were protective against infection.
The use of subconjunctival steroids at the end of cataract surgery was significant in the univariate (P<0.001) but not in the multivariate analysis. The variable subconjunctival steroid was positively correlated (Kendall's τ=0.35, P<0.001) with the subconjunctival antibiotic variable and when both variables are entered into the logistic regression model the subconjunctival steroid variable is no longer significant (P=0.18).
Discussion
This study utilised a case–control methodology, which is an efficient design for evaluating risk factors for a rare occurrence, such as endophthalmitis, because of its relative speed and reduced cost compared to other study designs. The univariate analysis highlighted risk factors that may have been important and subsequent multivariate logistic regression models allowed further identification of the most important independently acting risk factors. Risk factors with poor representation in the medical records (IOL haptics) or which occurred infrequently (history of immunosuppression, conversion from phaco to ECCE, use of intraoperative and postoperative antibiotics) could not be entered into a multivariate model.
A history of immunosuppression in this study (patients with leukaemia, lymphoma, and myelodysplasia) was significant in the univariate analysis (odds ratio 7.53 (95% CI, 1.55–36.55)), but was only present in 2/445 (0.4%) controls. Despite exclusion from the multivariate analysis our results suggest that preoperative immunosuppression may still have clinical importance. A retrospective case–control study by Montan et al2 concluded that preoperative immunosuppressive treatment was a significant risk factor for endophthalmitis after cataract surgery.
The use of intraoperative antibiotics did not have a protective effect and was significantly associated with postoperative PIE in the univariate analysis (odds ratio 7.28, 95% CI 2.34–22.60), but this variable occurred in too small numbers (4/445 (0.9%) controls) for further analysis. The evidence regarding the use of antibiotics in the irrigating solution during cataract surgery is conflicting.5, 6, 7 For this study a surprisingly high percentage of cases receiving intraoperative antibiotics (75%) showed bacterial growth from the ocular samples taken at the time of treatment for endophthalmitis. Unfortunately, we were unable to speculate on the effectiveness of the intraoperative antibiotics as the antibiotic sensitivity data on the organisms cultured was not retrieved. In a recent evidence-based update of bacterial endophthalmitis prophylaxis for cataract surgery,8 irrigating solution antibiotics received a low clinical recommendation as the evidence supporting their use was weak.
Potentially important risk factors that were not significantly associated with PIE included a history of diabetes, silicone IOLs and multiuse phaco needles and phaco tubing. The use of preoperative povidone iodine surgical prep and preoperative antibiotics did not have a significant protective effect against the development of infection in this study. The omission of preoperative povidone iodine would have been difficult to identify as a risk factor as the majority of surgeons (93–95% of cases and controls) used povidone iodine surgical prep for the eyelids prior to surgery. Preoperative povidone iodine received a high clinical recommendation in a recent evidence-based update of prophylaxis for cataract surgery.7
The multivariate analysis revealed significantly increased risks for PIE to be associated with in-patient cataract surgery, surgery in dedicated eye theatres, lack of face mask use in theatre, consultant grade surgeon, posterior capsule tear during cataract surgery, and the nonadministration of subconjunctival antibiotics at the end of cataract surgery.
Javitt et al8 conducted a retrospective analysis of medicare records in America and identified reduced rehospitalisations for the treatment of endophthalmitis following a change from inpatient to outpatient cataract surgery. One possible explanation is that inpatients for cataract surgery are generally older with more medical disorders and may be more susceptible to postoperative infections than daycase patients.9 Daycase cataract surgery patients may also be exposed to fewer or different pathogens compared with inpatients.
The association of dedicated eye theatres and PIE was surprising as dedicated eye theatres would be expected to have ‘cleaner’ environments compared to eye theatres which share with other surgical specialities. This study, however, did not account for the operating environment in different theatres such as the type of theatre ventilation system employed, the number and movement of staff in theatre and differing theatre protocols, which may have been relevant.10 More inpatients (71%) were operated in dedicated eye theatres compared to nondedicated eye theatres (29%), which may have been significant as inpatients had an increased risk of PIE. We were unable to analyse some of these potential confounding factors as they were not measured in our study.
Consultants performing cataract surgery were associated with a significantly higher risk of postoperative PIE than registrar grade surgeons. As consultants are usually the most experienced ophthalmic surgeons they will perform more of the technically difficult cataract procedures compared to registrars. These difficult procedures may be associated with a higher risk of intraoperative and thus postoperative complications.
The wearing of face masks by the operating surgeon and scrub nurse is not thought to be effective in the prevention of contamination of the surgical field and is not universally undertaken in ophthalmic operating theatres. Schiff11 performed an uncontrolled experiment demonstrating that the number of bacterial colonies on blood agar plates, placed 30 cm from a person's mouth, increased in relationship to the volume at which the person spoke. He found that wearing a surgical mask with an overlapping hood reduced the levels of bacterial growth. Alwitry et al12 conducted a prospective randomised study comparing bacterial culture rates for masked and unmasked surgeons during cataract surgery. The group wearing a face mask showed significantly fewer bacterial counts from blood agar plates placed adjacent to the patient's head in the operative field. They hypothesised an increased risk of endophthalmitis with an increased bacterial load in the operative field. In a critical review of the evidence for and against the use of face masks in the operating theatre, Romney13 concluded that there was little convincing evidence to support discontinuing the wearing of surgical face masks.
Intraoperative communication with the vitreous cavity was found to be a significant risk factor for postoperative endophthalmitis. In vitro experiments have demonstrated that the vitreous is a better culture medium than the aqueous. Maylath and Leopold14 injected bacteria into the vitreous cavity of rabbits to produce endophthalmitis even though similar injections into the anterior chamber were rapidly cleared. Beyer et al15, 16 performed experiments in monkeys and showed that an intact posterior lens capsule had a significant barrier effect against the development of endophthalmitis when bacteria were introduced into the anterior chamber.
The administration of subconjunctival antibiotics at the end of surgery had a protective effect against the development of PIE. Lehmann et al17 demonstrated an association between nonadministration of subconjunctival cefuroxime and subsequent endophthalmitis, although the number of cases in this study was relatively small. Subconjunctival cefuroxime achieves therapeutic levels in the anterior chamber within 12–24 min of administration and maintains clinically significant levels for up to 12 h.17, 18 Postoperative therapeutic antibiotic levels within the anterior chamber will help to counteract the potential bacterial load in the eye as bacteria are present in the anterior chamber at the end of cataract surgery in 13–43% of patients.19, 20, 21
There are some limitations to this study. Case ascertainment was questionnaire-based and dependent on voluntary reporting by ophthalmologists throughout the UK. The case data provided would have therefore been subject to human errors in recording and reporting. Interpretation of the results of the study should also take account that the average response rate to BOSU over the 12-month study period was around 70%.3
In conclusion, the routine use of face masks during cataract surgery and subconjunctival antibiotics at the end of surgery are easily modifiable changes in clinical practice and should be strongly encouraged in the light of our results. Additional antibiotic prophylaxis to prevent infectious endophthalmitis should also be considered in patients who have posterior capsule rupture during cataract surgery.
References
Menikoff JA, Speaker MG, Marmor M, Raskin EM . A case–control study of risk factors for postoperative endophthalmitis. Ophthalmology 1991; 98(12): 1761–1768.
Montan PG, Koranyi G, Setterquist HE, Stridh A, Philipson BT, Wiklund K . Endophthalmitis after cataract surgery: risk factors relating to technique and events of the operation and patient history: a retrospective case–control study. Ophthalmology 1998; 105(12): 2171–2177.
Foot B, Stanford M, Rahi J, Thompson J . The British Ophthalmological Surveillance Unit: an evaluation of the first 3 years. Eye 2003; 16: 1–7.
Kamalarajah S, Silvestri G, Sharma NK, Khan A, Foot B, Ling R et al. Surveillance of endophthalmitis following cataract surgery in the UK. Eye 2004; 18: 580–587.
Ling R, Kamalarajah S, Cole M, James C, Shaw S . Suprachoroidal haemorrhage complicating cataract surgery in the UK: a case–control study of risk factors. Br J Ophthalmol 2004; 88(4): 474–477.
Hosmer DW, Lemeshow S . Applied Logistic Regression, 2nd ed. Wiley: New York, 2000.
Ciulla TA, Starr MB, Masket S . Bacterial endophthalmitis prophylaxis for cataract surgery. Ophthalmology 2002; 109: 13–26.
Javitt JC, Vitale S, Canner JK, Street DA, Krakauer H, McBean AM et al. National outcomes of cataract extraction. Endophthalmitis following inpatient surgery. Arch Ophthalmol 1991; 109(8): 1085–1089.
Desai P, Reidy A, Minassian DC . Profile of patients presenting for cataract surgery in the UK: national data collection. Br J Ophthalmol 1999; 83: 893–896.
Humphreys H, Taylor EW . Operating theatre ventilation standards and the risk of postoperative infection. J Hospital Infect 2002; 50: 85–90.
Schiff FS . The shouting surgeon as a possible source of endophthalmitis. Ophthalmic Surg 1990; 21(6): 438–440.
Alwitry A, Jackson E, Chen H, Holden R . The use of surgical facemasks during cataract surgery: is it necessary. Br J Ophthalmol 2002; 86: 975–977.
Romney MG . Surgical face masks in the operating theatre: re-examining the evidence. J Hospital Infect 2001; 47: 251–256.
Maylath FR, Leopold IH . Study of experimental intraocular infection. Am J Ophthalmol 1955; 40: 86–101.
Beyer TL, Vogler G, Sharma D, O’Donnell Jr FE . Protective barrier effect of the posterior lens capsule in exogenous bacterial endophthalmitis—an experimental primate study. Invest Ophthalmol Vis Sci 1984; 25(1): 108–112.
Beyer TL, O’Donnell FE, Goncalves V, Singh R . Role of the posterior capsule in the prevention of postoperative bacterial endophthalmitis: experimental primate studies and clinical implications. Br J Ophthalmol 1985; 69(11): 841–846.
Lehmann OJ, Roberts CJ, Ikram K, Campbell MJ, McGill JI . Association between nonadministration of subconjunctival cefuroxime and postoperative endophthalmitis. J Cataract Refract Surg 1997; 23(6): 889–893.
Jenkins CDG, Tuft SJ, Sheraidah G, McHugh DA, Buckley RJ . Comparative intraocular penetration of topical and injected cefuroxime. Br J Ophthalmol 1996; 80: 685–688.
Dickey JB, Thompson KD, Jay WM . Anterior chamber aspirate cultures after uncomplicated cataract surgery. Am J Ophthalmol 1991; 112(3): 278–282.
Manners TD, Chitkara DK, Marsh PJ, Stoddart MG . Anterior chamber aspirate cultures in small incision cataract surgery. Br J Ophthalmol 1995; 79(10): 878–880.
Mistlberger A, Ruckhofer J, Raithel E, Muller M, Alzner E, Egger SF et al. Anterior chamber contamination during cataract surgery with intraocular lens implantation. J Cataract Refract Surg 1997; 23(7): 1064–1069.
Acknowledgements
We gratefully acknowledge the data contribution to this study of approximately 200 ophthalmologists throughout the UK. In addition, we thank the control centers for providing data on the controls: Wycombe General Hospital, Central Middlesex Hospital, St George's Hospital, Bristol Eye Hospital, Musgrove park Hospital-Taunton, Royal United Hospital-Bath, Southport and Formby District General Hospital, Furness General Hospital, West Cumberland Hospital, Leeds General Infirmary, Alexandra Hospital-Redditch, Coventry and Warwickshire Hospital, and Princess Alexandra Eye Pavilion-Edinburgh. We are very grateful for the support of the British Ophthalmological Surveillance Unit. This project was also supported by the British Medical Association Middlemore award 1999 and the John William Clarke award 2000.
Author information
Authors and Affiliations
Corresponding author
Additional information
Presented at the Royal College of Ophthalmologists meeting, Birmingham, May 2003
Conflict of interest: Nil.
Ethics approval: Approval from the Local Ethics Committee, Belfast and the South West Multicentre Research Ethics Committee.
Rights and permissions
About this article
Cite this article
Kamalarajah, S., Ling, R., Silvestri, G. et al. Presumed infectious endophthalmitis following cataract surgery in the UK: a case–control study of risk factors. Eye 21, 580–586 (2007). https://doi.org/10.1038/sj.eye.6702368
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702368
Keywords
This article is cited by
-
Behind the mask: extended use of surgical masks is not associated with increased risk of surgical site infection
Pediatric Surgery International (2022)
-
Endophthalmitis following intravitreal anti-vascular endothelial growth factor (VEGF) injection: a comprehensive review
International Journal of Retina and Vitreous (2015)
-
Pathogenic conjunctival bacteria associated with systemic co-morbidities of patients undergoing cataract surgery
Eye (2013)
-
Reply to Bhavsar et al
Eye (2013)
-
Post-intravitreal anti-VEGF endophthalmitis in the United Kingdom: incidence, features, risk factors, and outcomes
Eye (2012)