Abstract
Aims
To evaluate the efficacy of diode laser trabeculoplasty (DLT) and frequency doubled Nd : YAG laser trabeculoplasty (YLT) in primary open angle glaucoma (POAG).
Methods
A total of 52 eyes of 35 patients with POAG were included. In all, 25 eyes underwent DLT (Group I) and 27 eyes underwent YLT (Group II). IOP, gonioscopy and visual fields were evaluated before and 3, 6, and 9 months and 1 year after the laser. An IOP<21 mmHg without medications or a decrease in the number of glaucoma medications with no progression of disc and field changes was considered a success.
Results
The mean age of patients in Group I was 57.72±8.1 years and the patients in Group II had a mean age of 59.85±7.76 years. The mean prelaser IOP was 24.93±1.49 mmHg and 25.36±1.57 mmHg. The mean IOP after DLT at 12 months follow-up was 18.0±0.93 mmHg and after YLT was 18.6±1.52 mmHg. The reduction of IOP was statistically significant in both the groups at 3, 6, 9, and 12 months (P<0.001), however there was no significant difference between the two groups. Success rates in both groups were similar, 92% in Group I and 92.6% in Group II.
Conclusions
DLT and Fd YLT are equally effective in controlling IOP in eyes with POAG.
Similar content being viewed by others
Main
Intraocular pressure (IOP) has been recognized as the most significant risk factor associated with optic disc damage in primary open-angle glaucoma (POAG).1 Historically, the initial treatment for POAG has been reduction of IOP through the use of various topical and systemic medications.2 If medications fail to reduce IOP to the required target levels , then surgical intervention is usually warranted. The introduction of argon laser trabeculoplasty (ALT)3 has enabled the ophthalmologist to interpose this treatment between medication and surgery in the hope that the pressure lowering effect of the laser procedure will either postpone or obviate the need for surgery. With confirmation, that the pressure lowering effect is good, the concept of using ALT as the primary treatment for POAG has become popular.4, 5, 6, 7, 8
Coagulative laser treatment for retinal diseases has shifted to the diode and frequency doubled Nd : YAG lasers and these have almost replaced the use argon lasers in ophthalmic hospitals. The efficacy of ALT has been well proven4, 5, 6, 7, 8 but there are very few studies showing the efficacy of DLT and YLT.9, 10, 11, 12, 13 To our knowledge, there are no studies comparing the efficacy of DLT to YLT.
Materials and methods
Consecutive patients having POAG were examined. The criteria for selection of the patients included phakic patients, age between 40–70 years, IOP between 21–30 mmHg, with/ without topical antiglaucoma medications, Cup-disc ratio >0.5 : 1, polar notching or narrowing of neuroretinal rim, asymmetry of cup-disc ratio between two eyes, visual field defects and an open anterior chamber angle on gonioscopy. The exclusion criteria for this study were one-eyed patient, patients with IOP ≥30 mmHg on two topical antiglaucoma medications, advanced visual field damage, patients with other ocular diseases such as uveitis, corneal opacity, and diabetic retinopathy.
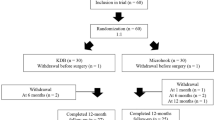
In total, 35 consecutive patients who satisfied the inclusion criteria were enrolled into the study after taking an informed consent. The study was approved by our institutional review board. In all, 17 patients had laser trabeculoplasty performed in both eyes, DLT in one eye and YLT in the other eye. In alternating patients, each type of laser was performed in the right eye and left eye, respectively. DLT was performed in the right eye in the first patient and YLT in the left eye, YLT was performed in the right eye and DLT in the left eye in the second patient and so on. In the remaining 18 patients, laser trabeculoplasty performed in one eye only, randomized to either DLT or YLT. A total of 52 eyes were treated and divided into two groups:
-
Group I — consisted of 25 POAG eyes that underwent DLT.
-
Group II — consisted of 27 POAG eyes that underwent YLT.
All patients were subjected to a detailed work-up before laser treatment. This included a record of the best corrected visual acuity, slitlamp biomicroscopy , applanation tonometery including a measurement of the diurnal fluctuation of IOP (07.00, 10.00, 13.00, 16.00, 19.00, and 22.00 hours), gonioscopy, fundus examination, and standard achromatic perimetry (30-2, Full Threshold, Humphrey field analyser). Patients were advised to continue their prelaser antiglaucoma medications, if they were already on medications. Oral acetazolamide (250 mg) was given to all patients and 1 drop of timolol 0.5% was instilled in the eye an hour before laser trabeculoplasty. Lignocaine 4% was used for topical anesthesia and a Ritch trabeculoplasty lens was applied using 2% methyl cellulose as a coupling medium. Laser trabeculoplasty was performed using the parameters below.
With the Diode laser, spot size was 50 μm, for a 0.1 s duration and the power ranged from 700 to 1200 mw. For the frequency doubled Nd : YAG laser the spot size was 100 μm, for a 0.2 s duration and the power ranged from 800 to 1270 mw. Mild blanching was taken as the end point. The laser was aimed at the junction of the anterior nonpigmented and posterior pigmented part of the trabecular meshwork. In all eyes, 360 degrees treatment was performed with 100 spots in one sitting. Postlaser, 0.1% dexamethasone drops 6 h for 5 days, 500 mg sustained release acetazolamide BD for 3 days were added to any prelaser antiglaucoma medications.
After laser trabeculoplasty the patients were monitored for an immediate postlaser rise in IOP and the development of uveitis. Applanation tonometry and slit lamp examination was made at 2 and 4 hours after the procedure. The patients were reviewed at 24 hour, 1, 4 weeks, 3 months and then every 3 months for a minimum of 1 year. Best corrected visual acuity assessment, fundus examination, and gonioscopy were performed at each visit. Visual field recording and diurnal variation of IOP were repeated every 6 months.
Antiglaucoma medications were tapered off gradually if the IOP on follow-up was ≤16 mmHg. If a patient was on multiple drops, they were sequentially tapered. The IOP was recorded at 48 hours and at 2 weeks after stopping each drug. If at any time, the IOP rose above 21 mmHg, the drugs were restarted. An IOP of more than or equal to 21 mmHg on prelaser treatment was taken as a failure. IOP less than 21 mmHg with or without topical medications, less than prelaser, with no further progression of disc and field changes was taken as the criteria for success.
The data was analysed by standard statistical methods (SPSS 10). The student ‘t’ test was applied to compare data between the two groups for example — mean reduction of IOP, diurnal variation. χ2-test was used for analysing distribution among various sub-groups. A P-value of less than 0.05 was taken as significant.
Results
Laser trabeculoplasty was performed in 52 eyes of 35 patients of primary open angle glaucoma using diode laser or Frequency doubled Nd : YAG laser. There was no significant difference in the demographic parameters in the two groups. Group I consisted of 19 male patients and six female patients with a mean age of 57.72±8.1 years. Group II consisted of 22 males and 6 females with a mean age of 59.85±7.76 years .The mean cup disc ratio was 0.60±0.15 in group I, and 0.61±0.2 in group II. Visual field evaluation showed that MD and CPSD in I was −6.40±6.63 dB and 4.88±3.98 dB in group I while it was −8.65±9.9 dB and 5.51±3.3 dB in group II respectively (Table 1).
The prelaser mean IOP was 24.93±1.5 mmHg in group I (range 21–28 mmHg) and 25.36±1.6 mmHg in group II (range 22–29 mmHg). In group I, the mean IOP on follow up was 18.43±1.5 mmHg at 3 months, 18.83±1.5 mmHg at 6 months, 18.33±1.30 mmHg at 9 months, and 18.00±0.93 mmHg at 12 months. The actual IOP reduction was 6.50±1.15 mmHg at 3 months (26.1%), 6.09±0.97 mmHg at 6 months (24.4%), 6.33±0.92 mmHg at 9 months (25.4%) and 6.2±0.72 mmHg at 12 months (24.8%). In group II the mean IOP at 3, 6, 9, 12 months follow up was: 18.45±1.38, 18.9±1.6, 18.0±1.4 and 18.6±1.5 mmHg respectively. The actual IOP reduction was 6.89±1.0 mmHg at 3 months (26.6%), 6.5±0.9 mmHg at 6 months (25.6%), 7.2±0.9 mmHg at 9 months (28.4%), and 6.5±1.3 mmHg at 12 months (25.6%). There was a significant drop in IOP from baseline values in each group. There was no statistically significant difference in the reduction of IOP in between the two groups at all time periods (Table 2).
In group I, the mean prelaser diurnal fluctuation of IOP was 5.88±1.2 mmHg which reduced to 2.7±0.90 mmHg at 6 months and 2.8±1.7 mmHg at 12 months (P<0.001). In group II, the mean diurnal fluctuation of IOP was 5.59±1.3 mmHg before laser and 2.41±1.2 mmHg at 6 months and 2.56±1.5 mmHg at 12 months postlaser (P<0.001). There was a significant decrease in IOP fluctuation as compared to baseline values but there was no significant difference in the diurnal fluctuation changes in the two groups (Table 3).
In group I, an immediate postlaser IOP rise was seen in five eyes (20%) ranging from 2 to 4 mmHg. Mild iritis was seen in 2 eyes. New peripheral anterior synechiae (PAS) were seen in four eyes (16%) occupying between 2 and 4 clock hours. In group II, an immediate postlaser IOP rise was seen in six eyes (22.2%), ranging from 3 to 5 mmHg, mild iritis was seen in three eyes and PAS formation was seen in six eyes (22.2%) occupying between 2 and 3 clock hours.
All eyes were on medication before laser treatment. In group I, eight eyes (32%) were on one drug, 16 eyes (64%) were on two drugs and one eye (4%) was on three drugs while in group II, 11 eyes (40.7%) were on one drug and 16 eyes (59.26%) were on two drugs at the start of the study. At the final follow up in group I, seven eyes (28%) were on no drugs, 17 eyes (68%) on one drug, one eye (4%) on two drugs and none on three drugs, while in group II, 11 eyes (40.7%) were off medication, 15 eyes (55.55%) were on one drug and one eye (3.7) was on two drugs.
The success rate in group I was 92% and in group II was 92.6%, respectively, at the conclusion of the study with both laser treatments being equally effective in controlling the IOP.
Discussion
The glaucoma laser trial8 suggested that laser therapy is atleast as efficacious as medical therapy. Many different types of laser have been used to perform a trabeculoplasty and have been found efficacious. Although there are a few studies on DLT9, 10, 11, 12 and YLT,13 there are no studies comparing DLT with YLT.
In the present study, there was a lowering of 6.2±0.72 mmHg in the IOP at 12 months with DLT and 6.5±0.9 mmHg with YLT. This leads to reduction in the number of medications with 96% of eyes being on one or no medications in both the groups. Mean IOP reduction with ALT in a similar population was reported to be 6.4±2.0 mmHg at 12 months.4 McHugh et al9 carried out a pilot study to examine the efficacy of diode laser trabeculoplasty in the treatment of POAG and ocular hypertension in 20 eyes resulting in a mean IOP drop of 10.2 mmHg at 2 weeks and 9.5 mmHg at 6 months. Moriarty et al10 reported a mean IOP reduction of 8.4±2.6 mmHg at 12 months and 7.9±3.63 mmHg at 24 months after DLT, while Chung et al12 reported a drop in IOP from 21.2±1.2 to 16.3±1.2 mmHg at 1 year after DLT.
The success rate was 92% with DLT and 92.6% with YLT in the current study after 1 year. Chung et al12 showed >80% success rate for DLT at 12 months follow up which declined to 50% at end of 5 years. In Glaucoma laser trial8 the success rate was 70% with ALT and timolol at two years of follow up. A success rate of 75% was reported with ALT alone as a primary therapy at 1 year in a similar population earlier with all patients being controlled with ALT combined with one or two topical medications.4
Diurnal fluctuation of IOP was reduced from 5.8±1.2 to 2.8±1.7 mmHg at 12 months with DLT and from 5.5±1.3 to 2.56±1.5 mmHg in the YLT group. A previous study of ALT in the same population found the diurnal fluctuation to decrease from 7.9±1.4 to 3.5±1.4 mmHg at 1 year.4 Effects of frequency-doubled Nd : YAG laser trabeculoplasty (YLT) on diurnal IOP variations in POAG were studied by Guzey et al,13 12 weeks after YLT, significant IOP reductions were observed: 36.4% in the mean IOP, 29.7% in the mean peak IOP and 50% in the mean pressure range. Greenidge et al14 reported a beneficial effect of ALT on diurnal curve, although pressure spikes were not totally eliminated. The mean peak pressure, was found to decrease by 25%. It was observed that although at end of follow-up, all cases were controlled with addition of one, two or three topical drugs, the diurnal variation was reduced significantly, even in those patients in whom drugs had to be added. Large fluctuations in diurnal IOP are a significant risk factor in the progression of glaucoma15 and so a reduction in diurnal variation would be beneficial, even in those patients in whom medications are to be added.
The low incidence of IOP spikes seen in our study could be attributed to the pre-laser medication given. Brancato et al11 found IOP spikes of less than 5 mmHg in their patients post-DLT. The Glaucoma laser trial reported a post-treatment rise of IOP in 34% of eyes in the laser first group with no prelaser treatment.8
In our study, mild iritis was seen in two eyes of group I, and three eyes of group II. This was controlled with topical steroids. Moriarty et al16 found a mild cellular anterior chamber reaction in 4 eyes post-DLT, but this did not need antiinflammatory treatment.
PAS were seen in 16% eyes after DLT and 22% eyes after YLT. No PAS have been reported in prior studies on DLT.9, 10 The Glaucoma laser trial reported an incidence of PAS formation to be 46% in eyes that received primary therapy.8 An incidence of 22% of PAS was found post-ALT in a study by Rouhiainen et al.17
In conclusion diode laser trabeculoplasty and frequency doubled Nd : YAG trabeculoplsty appear to be equally efficacious in lowering the IOP and reducing the diurnal fluctuation of IOP in eyes with POAG over a 12 month period. They also appear to be atleast as effective as ALT in the medium term. A longer follow-up is required to establish their long term efficacy in the management of POAG.
References
Sommer A . Intraocular pressure and glaucoma. Am J Ophthalmol 1989; 107: 186–188.
Shultz JS . Initial treatment of glaucoma: surgery or medication – Chop or drop. Surv Ophthalmol 1993; 37: 293–299.
Wise JB, Witter SL . Argon laser therapy for open-angle glaucoma: a pilot study. Arch Ophthalmol 1979; 97: 319–322.
Agarwal HC, Sihota R, Das C, Dada T . ALT as primary and secondary therapy in OAG in Indian eyes. Br J Ophthalmol 2002; 86: 733–736.
Odberg T, Sandvik L . The medium and long-term efficacy of primary argon laser trabeculoplasty in avoiding topical medication in open angle glaucoma. Acta Ophthalmol Scand 1999; 77(2): 176–181.
Sharma A, Gupta A . Primary argon laser trabeculoplasty vs pilocarpine 2% in primary open angle glaucoma: two years follow-up study. Indian J Ophthalmol 1997; 45(2): 109–113.
Shingleton BJ, Richter CU, Dharma SK, Tong L, Bellows AR, Hutchinson BT et al. Long-term efficacy of argon laser- trabeculoplasty. A 10-year follow up. Ophthalmology 1993; 100: 1324–1329.
The Glaucoma Laser Trial (GLT). Results of argon laser trabeculoplasty vs topical medicines. The Glaucoma Laser Trial Research Group. Ophthalmology 1990; 97(11): 1403–1413.
McHugh D, Marshall J, Ffytche TJ, Hamilton AMP . Diode laser trabeculoplasty for primary open angle glaucoma and ocular hypertension. Br J Ophthalmol 1990; 74: 743–747.
Moriarty AP, Mchugh JD, Ffytche TJ, Hamilton AMP . Long-term follow-up of diode laser trabeculoplasty for primary open-angle glaucoma and ocular hypertension. Ophthalmology 1993; 100(11): 1614–1618.
Brancato R, Roberto C . Diode Laser compared with argon laser for trabeculoplasty. Am J Ophthalmol 1991; 112: 50–55.
Chung PV, Schuman JS, Netland PA, Muhammad RA, Jacobs DS . Five-year results of a randomized prospective clinical trial of diode vs argon laser trabeculoplasty for open angle glaucoma. Am J Ophthalmol 1998; 126(2): 185–190.
Guzey M, Arslan O, Tamcelik N, Satici A . Effects of frequency-doubled Nd : YAG laser trabeculoplasty on diurnal intraocular pressure variations in primary open-angle glaucoma. Ophthalmologica 1999; 213(4): 214–218.
Greenidge KC, Spaeth GI, Silva F . Effect of argon laser trabeculoplasty on the glaucomatous diurnal curve. Ophthalmology 1983; 90: 800–803.
Asrani S, Zeimer R, Wilensky J, Gieser D, Vitale S, Lindenmuth K . Large diurnal fluctuations in intraocular pressure are an independent risk factor in patients with glaucoma. J Glaucoma 2000; 9(2): 134–142.
Moriarty AP, Mchugh JD, Spalton DJ . Comparison of the anterior chamber inflammatory response to diode and argon laser trabeculoplasty using a laser flare meter. Ophthalmology 1993; 100(8): 1263–1267.
Rouhainen HJ, Terasvitra ME, Tuovinen EJ . Peripheral anterior synechiae formation after trabeculoplasty. Arch Ophthalmol 1988; 106: 189–191.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Agarwal, H., Poovali, S., Sihota, R. et al. Comparative evaluation of diode laser trabeculoplasty vs frequency doubled Nd : YAG laser trabeculoplasty in primary open angle glaucoma. Eye 20, 1352–1356 (2006). https://doi.org/10.1038/sj.eye.6702108
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702108