Abstract
Purpose
To study a preferred technique of phacoemulsification in eyes with posterior polar cataract and report its outcome.
Methods
Under topical anesthesia, phacoemulsification was carried out after hydrodelination in 23 cases (38 eyes) with ages ranging from 19 to 65 years (mean=33.5 years). Hydrodissection was not performed.
Results
Mean duration of follow-up was 9.5 months. None of the eyes developed posterior capsule rupture, but seven eyes (18.4%) revealed posterior capsule plaque postoperatively, which needed neodymium : YAG laser capsulotomy. Mean visual acuity improved significantly after surgery (P=0.0001, paired t-test); In all, 34 eyes achieved a best-corrected visual acuity of 20/40 or more (89.4%). However, the postoperative visual acuity was less than 20/25 in 11 eyes (28.9%). The causes of the low acuity were amblyopia in eight eyes (21.0%) and macular degeneration due to retinitis pigmentosa in two others (5.2%).
Conclusion
Phacoemulsification is an effective and safe method to treat posterior polar cataract with gentle hydrodelination ‘hydrodissection free phacoemulsification technique’. This is especially true when great attention is paid to the ‘floppy’ posterior capsule. Although previous amblyopia might interfere with excellent surgical outcome in patients with a unilateral or highly asymmetric bilateral cataract, visual acuity improved significantly in most cases.
Similar content being viewed by others
Introduction
Posterior polar cataract is a common type of visually symptomatic congenital cataract. This dense white opacity is situated on the central posterior capsule and consists of characteristic circular plaque with concentric whorls. The opacity extends anteriorly into the posterior cortex and is thicker than the standard posterior subcapsular cataract.1, 2 Although sporadic cases of this type of cataract exist, it is usually inherited in an autosomal-dominant manner.3, 4, 5
Owing to the high rate of posterior capsule rupture, the management of posterior polar cataract has been a challenge even for the most skilled cataract surgeons. Osher et al6 reported a 26% incidence of capsule rupture in a series of 31 cases and Vasavada and Singh7 reported a 36% incidence in 22 cases.
Many surgeons have tried to modify the surgical technique to lower the complications associated with posterior cataract, Fine et al8 used minimal hydrodissection and hydrodelineation, nuclear aspiration from within the epinuclear shell, and gentle viscodissection of the epinucleus and cortex to avoid unnecessary pressure on the posterior capsule and to protect the region of greatest potential weakness throughout the procedure. Allen and Wood9 used viscodissection to gently dissect only the peripheral cortex from the capsule. Lee and Lee10 did not attempt hydrodissection, used low vacuum, low aspiration, low inflow parameters, and manual dry aspiration to remove the epinucleus and cortex.
We, therefore, conducted a prospective study to determine the efficacy and safety of ‘hydrodissection free phacoemulsification technique’ with attention to floppy posterior capsule to appraise a strategy to improve the result of surgical management of posterior polar cataract.
Materials and methods
A total of 23 patients with visually significant posterior polar cataract participated consecutively in a prospective study between December 2001 and December 2004. An attempt was made to separate visual impairment due to cataracts from that due to amblyopia. The presence of amblyopia was suspected in patients with unilateral or asymmetric opacities but confirmed after surgery in all amblyopic patients by visual acuity measurement.
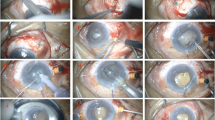
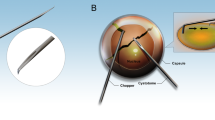
One surgeon performed all cataract surgeries. After topical anaesthesia, a 3.2 temporal single-plane clear corneal incision was made, and a dispersive viscoelastic was injected into the anterior chamber, while overfilling was avoided. Then, a 5.0 mm (but no larger) continuous curvilinear capsulorhexis was created with a bent needle. No hydrodissection was attempted and only careful, controlled hydrodelineation was performed with a small amount of fluid. Phacoemulsification was carried out with 45° phaco tip using low pulsed power and low vacuum (20–30% power and 40–65% vacuum). The epinucleus and cortex were removed using manual dry aspiration. The peripheral lens material was viscodissected and extracted first, leaving the central posterior material until last. When posterior plaque adhered to the capsule firmly, it was left alone for eventual neodymium : YAG laser capsulotomy. As a result of potential fragility, polishing the central portion of the posterior capsule was avoided. The lens capsule was then inflated with viscoelastic, and a foldable acrylic IOL was implanted in the capsular bag. The IOL used was from MA60BM, Alcon Surgical in 21 eyes and from Acreos fit, Bausch & Lomb in 17 others.
Best-corrected visual acuity at baseline and during follow-up was checked using the standard Snellen chart, and the result was converted to logarithm of the minimum angle of resolution (logMAR) to allow statistical analysis. The paired t-test was used to compare the mean preoperative and postoperative visual acuities. A P-value less than 0.05 was considered to be statistically significant.
Results
In total, 38 eyes of 23 patients were included in the study. Of them, 12 were male and 11 were female patients. Bilateral involvement was noted in 15 cases. Mean age at presentation was 33.5 years (from 19 to 65 years). Patients were followed for an average of 9.5 months, ranging from 2 to 20 months.
None of the eyes developed posterior capsule rupture; but in seven eyes (18.4%), the entire polar opacity could not be aspirated during surgery because portions of the opacity firmly adhered to the posterior capsule and were left alone for eventual neodymium : YAG laser capsulotomy.
Table 1 shows the mean preoperative and postoperative visual acuities. The mean visual acuity was significantly better after cataract surgery (P=0.0001, paired t-test). Figure 1 shows postoperative visual acuities at the end of the follow-up period. In all, 34 eyes achieved a best-corrected visual acuity of 20/40 or more (89.4%). A postoperative visual acuity of 20/25 was not achieved in 11 eyes (28.9%). The causes were pre-existing amblyopia in eight eyes (21.0%) and macular degeneration due to retinitis pigmentosa in two eyes (5.2%) of one of the patients. Of the 14 patients with unilateral or highly asymmetric bilateral cataract, seven (50%) had amblyopia, though there was no deep amblyopia (ie, best-corrected visual acuity <20/200).
Discussion
Surgical management of posterior polar cataracts is a special challenge to the cataract surgeon and it is known to predispose to posterior capsule rupture during cataract surgery.6, 7, 10, 11, 12, 13 The incidence of posterior capsule rupture has been reported to be 266–36%.7 In contrast to recent studies, which showed a low incidence of posterior capsule rupture (7.1% in Hayashi et al13 cases, 11.1% in Lee and Lee10 cases, and 16.7 % in Liu et al14 cases), posterior capsule rupture occurred in none of our cases. We believe that our success depended on three factors: first, using a modified surgical ‘hydrodissection free phacoemulsification’ technique, second, paying great attention to the floppy posterior capsule, and third, avoidance of directly dissecting the polar opacity from the posterior capsule during phacoemulsification.8, 13
When operating on eyes with posterior polar cataract, surgeons must be careful of posterior capsule rupture as the capsule underlying it tends to be unusually weak,6, 7, 11, 12, 13 and this weakness could predispose to posterior capsular rupture with only a minimal trauma. During phacoemulsification or aspiration surgery, we were careful in gently separating the polar opacity from the posterior capsule. We did not perform hydrodissection to avoid unnecessary pressure on the posterior capsule.7, 8, 10, 13 In contrast to some previous studies,6 we did not observe any defect in the posterior capsule, but a central thinning. Moreover, we added a new concept to the special situation calling ‘floppy posterior capsule’ in which the funnel-shaped posterior capsule is abnormally thin, loose, trembling and could be easily aspirated by the phaco tip if not kept away. Therefore, we performed hydrodelination to create a cushion and used low vacuum, low aspiration to ensure a more stable anterior chamber.10
The peripheral lens material was viscodissected and extracted first, leaving the central posterior material until last. In this way, the thin dangerous area was always covered until the final removal of the cortex.6, 7, 8, 9 Moreover, the epinucleus and cortex were removed using manual dry aspiration. This method seems gentle, controllable and there is no after-aspiration effect. However, one disadvantage is the increased surgical time.10
In seven cases, there was exceedingly tight adherence of the plaque to otherwise normal posterior capsule, which could not be easily separated. In these cases, the plaque was left behind for eventual neodymium : YAG laser capsulotomy.7, 8, 13
Even though retinal detachment was reported in some previous studies,13 none of our cases were complicated by retinal detachment. This might be due to lack of posterior capsule rupture in our cases. In most cases, visual acuity improved significantly and 89.4% achieved a best-corrected visual acuity of 20/40 or more. However, 28.9% of eyes did not achieve a postoperative visual acuity of 20/25. Most of these cases were patients who had amblyopia due to unilateral or highly asymmetric bilateral cataract. However, deep amblyopia was not observed. These results were consistant with the results of previous studies.7, 13 The association of retinitis pigmentosa and posterior polar cataract has been reported by SaebΦ15 and Yamada et al.5 Of course, one of our patients with bilateral cataract had retinitis pigmentosa; and his visual acuity did not reach more than 20/200 postoperatively.
Despite previous reports of a high incidence of posterior capsule rupture in surgical management of posterior polar cataract by phacoemulsification, we found that ‘hydrodissection free phacoemulsification’ reduced the rate of posterior capsule rupture.We also recommend avoiding the ‘floppy’ posterior capsule during operation and leaving the posterior capsule to be opened by eventual neodymium : YAG laser capsulotomy, if necessary. In addition, we must consider preexisting amblyopia as it might interfere with excellent surgical outcome in patients with a unilateral or highly asymmetric bilateral cataract.
References
Eshagian J . Human posterior subcapsular cataracts. Trans Ophthalmol Soc UK 1982; 102: 364–368.
Duke-Elder S . Posterior polar cataract. In: Duke-Elder S (ed). System of Ophthalmology, Vol. 3, part 2: Normal and Abnormal Development, Congenital Deformities. Mosby: St Louis, MO, 1964, pp 723–726.
Tulloh CG . Hereditary posterior polar cataract with report of a pedigree. Br J Ophthalmol 1955; 39: 374–379.
Ionides A, Francis P, Berry V . Clinical and genetic hetrogeniety in autosomal dominant cataract. Br J Ophthalmol 1999; 83: 802–808.
Yamada K, Tomita H-A, Kanazawa S, Mera A, Amerniya T, Niikawa N . Genetically distinct autosomal dominant posterior polar cataract in a four-generation Japanese family. Am J Ophthalmol 2000; 129: 159–165.
Osher RH, Yu BC-Y, Koch DD . Posterior polar cataracts: a predisposition to intraoperative posterior capsule rupture. J Cataract Refract Surg 1990; 16: 157–162.
Vasavada A, Singh R . Phacoemulsification in eyes with posterior polar cataract. J Cataract Refract Surg 1999; 25: 238–245.
Fine H, Packer M, Hoffman RS . Management of posterior polar cataract. J Cataract Refract Surg 2003; 29: 16–19.
Allen D, Wood C . Minimizing risk to the capsule during surgery for posterior polar cataract. J Cataract Refract Surg 2002; 28: 742–744.
Lee MW, Lee YC . Phacoemulsification of posterior polar cataracts: a surgical challenge. Br J Ophthalmol 2003; 87: 1426–1427.
Hiles DA, Chotiner B . Vitreous loss following infantile cataract surgery. J Pediatr Ophthalmol 1977; 14: 193–199.
Skalka HW . Ultrasonic diagnosis of posterior lens rupture. Ophthalmic Surg 1977; 8: 72–76.
Hayashi K, Hayashi H, Nakao F . Outcomes of surgery for posterior polar cataract. J Cataract Refract Surg 2003; 29: 45–49.
Liu Y, Liu Y, Wu M . Phacoemulsification in eyes with posterior polar cataract and foldable intraocular lens implantation. Yan Ke Xue Bao 2003; 19: 92–94.
SaebΦ J . An investigation into the mode of heredity, congenital and juvenile cataracts. Br J of Ophthalmol 1949; 33: 601–629.
Acknowledgements
Ethic approval: The review board and ethical committee of Eye Research Center of Tehran University of Medical Sciences approved the trial.
Competing interests: There is no competing interest.
Informed consent: Written informed consent was obtained from all the patients after complete explanation.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Siatiri, H., Moghimi, S. Posterior polar cataract: minimizing risk of posterior capsule rupture. Eye 20, 814–816 (2006). https://doi.org/10.1038/sj.eye.6702023
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702023
Keywords
This article is cited by
-
Phacoemulsification with hydrodelineation and OVD-assisted hydrodissection in posterior polar cataract
BMC Ophthalmology (2018)
-
Surgical approaches to posterior polar cataract: a review
Eye (2012)
-
Phacoemulsification with Viscodissection in Posterior Polar Cataract: Minimizing Risk of Posterior Capsule Tear
Annals of Ophthalmology (2007)