Abstract
Aims
To compare the efficacy of the high specificity Frequency Doubling Technology (FDT) Perimeter Screening Program (C-20-1) to standard threshold automated perimetry in the diagnosis of open-angle glaucoma.
Methods
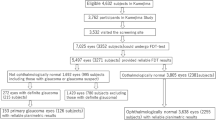
A total of 100 consecutively presenting patients attending a glaucoma clinic who volunteered for the study (approximately 30% of whom were attending for an initial visit) were examined with the FDT C-20-1 Screening Program and with the Humphrey Field Analyzer (HFA) SITA Fast algorithm and Program 24-2.
Results
Of the patients, 17 were excluded due to unreliable visual field results or non-glaucomatous ocular abnormalities. In all, 10 patients were diagnosed as normal, 54 with open-angle glaucoma, eight with ocular hypertension, and 11 as glaucoma suspects. Of the 54 glaucomatous patients, 45 exhibited high-tension glaucoma and nine normal tension glaucoma. Perimetry with the HFA gave a sensitivity of 81.5% for the combined category of glaucoma and glaucoma suspect and a specificity of 83.3% for the combined category of normal and ocular hypertension. Perimetry with the FDT gave a sensitivity of 74.5% and a specificity of 85.2% compared to that of the HFA.
Conclusion
In the detection of glaucoma, Program C-20-1 of the FDT perimeter exhibits high specificity. It exhibits low sensitivity for the detection of mild loss but high sensitivity for advanced field loss relative to Program 24-2 and the SITA Fast algorithm of the HFA.
Similar content being viewed by others
Introduction
Tests of magnocellular function may facilitate the early detection of glaucomatous damage either by isolating selective magnocellular death or because the magnocellular pathway provides a sensitive index of damage due to its sparse sampling, that is reduced redundancy, across the retina.1, 2, 3, 4, 5, 6
Complete isolation of the magnocellular pathway may not be possible. However, the frequency doubling illusion is thought to be mediated by a subset of the magnocellular cells, the My cells, which exhibit a non-linear response to contrast.7, 8, 9 In the illusion, a low spatial frequency sinusoidal grating undergoing rapid temporal frequency counterphase flicker appears to exhibit twice the spatial frequency.
Frequency doubling was originally applied to patients with glaucoma by Maddess and Henry3 and by Maddess et al.10 However, the commercially available Frequency Doubling Technology (FDT) perimeters (Carl Zeiss Meditec Inc, Dublin, CA and Welch Allyn, Skaneateles Falls, NY, USA) are a relatively new introduction in ophthalmic practice.4 The stimulus of the FDT perimeter is approximately 10° in diameter and comprises a 0.25 cycles per degree sine wave grating counterphased at 25 Hz, which is presented for a maximum of 720 ms at each of 17 locations out to an eccentricity of 20° (Programs C-20-1, C-20-5 and C-20) and can include an additional stimulus location above and below the horizontal midline, nasally, between 20° and 30° (Programs N-30-1 and N-30-5, and N-30). Programs C-20-1, C-20-5, N-30-1, and N-30-5 present the stimulus at suprathreshold levels while Programs C-20 and N-30 estimate the threshold response. The initial suprathreshold increment for Programs C-20-5 and N-30-5 was chosen to produce high sensitivity for the detection of glaucoma and that for Programs C-20-1 and N-30-1 high specificity.
The C-20 threshold algorithm of the FDT exhibits acceptable performance in the diagnosis of glaucoma compared to standard automated perimetry using the Full Threshold algorithm of the HFA.11, 12, 13, 14, 15, 16, 17, 18, 19, 20, 21 It also compares favourably with the faster thresholding algorithms of the Octopus Automated Perimeter,22, 23 namely Tendency Orientated Perimetry (TOP) and the Dynamic Strategy, and also with Short Wavelength Automated Perimetry18, 19, 24 and with High-Resolution Perimetry.25, 26
Fast screening techniques are necessary to reduce the number of false-positive referrals to glaucoma clinics, but the techniques also need to be able to detect the early stages of the disease. The Screening Program C-20-1 of the FDT has been evaluated with respect to Programs 24-2 or 30-2 and either the SITA Standard or Full Threshold algorithms of the HFA.11, 12, 27, 28, 29, 30 The HFA SITA Fast algorithm in conjunction with Program 24-2 is gaining popularity in some glaucoma clinics due to its shorter examination time compared to that with the HFA SITA Standard algorithm, which, for patients with glaucoma, takes approximately 6–8 min per eye for Program 30-2.31, 32, 33, 34 The SITA Fast algorithm and Program 24-2 typically takes 4–5 min per eye in patients with glaucoma35 while the C-20-1 screening program of the FDT takes in the region 1–2 min per eye.11, 22, 30, 35 To our knowledge, only two studies have compared the FDT suprathreshold Program C-20-1 with HFA Program 24-2 and the SITA Fast algorithm.22, 35 Allen et al35 evaluated these two techniques in a systematic screening program of 574 attendees to a convention. Only those who exhibited abnormality with the FDT (12%) were examined with the HFA. A low false-positive rate and a good positive predictive value were present compared to the HFA. Wadood and et al22 evaluated the sensitivity and specificity of the two techniques, and also that of the Octopus TOP strategy, in the better eye of 70 patients with moderate-to-advanced glaucoma, against the diagnosis based upon stereoscopic examination of the optic nerve head. The criterion for the FDT of one or more stimulus locations exhibiting abnormality generated the largest area (93.9%) for the Receiver Operator Curve and a sensitivity and specificity of 91.4% and 96.4%, respectively.
It is important that new medical technologies are evaluated with respect to established investigative techniques and on cohorts with well-characterised disease. Frequently, comparison between studies can be difficult because of variations in the composition of the study cohort. For example, inclusion of patients with advanced disease inflates the sensitivity and specificity for detection of the disease. To gain a realistic assessment of clinical efficiency, it is important that evaluation is performed in cohorts that are representative of those in clinical practice.
We evaluated the use of FDT Program C-20-1 in patients attending a hospital-based glaucoma clinic. Efficacy was determined by comparison, firstly, with a consultant-based clinical diagnosis, based soley upon stereo examination of the optic disc, and secondly, with the SITA Fast algorithm and Program 24-2. We determined the ability of Program C-20-1 to localise the location and depth of focal loss using two different approaches (the number of locations at which the stimulus was not seen, and the summed Total and Pattern Deviation probability scores).
Methods
A total of 100 consecutive patients who volunteered for the study were recruited during their visit to the Glaucoma Clinic of the Cardiff Eye Unit, University Hospital of Wales, Cardiff. The patients were examined with HFA Program 24-2 and the SITA Fast algorithm as part of their routine clinical care and had volunteered to be examined, at the same appointment, with Program C-20-1 of the FDT. Patients were excluded from the study only if the distance visual acuity was worse than 6/12. The study had approval from the Bro Taf Local Research Ethics Committee and informed written consent was obtained from all patients.
Both eyes of each patient underwent perimetry; the right eye was examined before the left eye for each patient. The patients received the demonstration program of the FDT immediately prior to examination with Program C-20-1. The order of examination was randomised for the HFA and FDT. The interval between the examination of the two eyes of a patient for the given type of perimetry was approximately 1 min and the interval between the two types of perimetry was a minimum of 5 min. No rest periods were given during the examination of the given eye with either type of perimetry.
The clinical diagnosis was based upon stereoscopic examination of the optic disc and of the fundus, through a dilated pupil. The outcome from applanation tonometry, gonioscopy, and the perimetry with the HFA was used to qualify the type of glaucoma. Pachymetry was not undertaken.
Open-angle glaucoma was defined as an optic nerve head appearance characteristic of the disease (including increase in cup size, increase in cup disc ratio, disc asymmetry, changes in the lamina cribrosa, loss of neuroretinal rim, pallor, evidence of peripapillary atrophy, vessel changes or disc margin haemorrhage) either in the presence or in the absence of a visual field defect consistent with the disease. Ocular hypertension was defined as a normal optic nerve head and a normal visual field in the presence of a repeatable intraocular pressure (IOP) greater than 22 mmHg on two successive occasions. Glaucoma suspects were defined as an asymmetry of ≥0.2 in the vertical cup to disc ratio and no family history of glaucoma, or an asymmetry of ≥0.1 with a family history of glaucoma and normal visual fields and IOPs. Normality was defined as a normal optic nerve head and a normal visual field in each eye, an IOP of less than 21 mmHg in each eye, and no family history of glaucoma. Other diseases were categorised by the clinical characteristics specific to the given disease entity. All cases of non-glaucomatous abnormality were excluded from the subsequent analysis.
The HFA visual fields were separately classified by one of us (JMW), who has over 20 years of experience in interpreting visual fields derived by automated perimetry, and who was masked to the clinical diagnosis and to the results of the FDT perimeter. The degree of field loss was described using the system of Hodapp et al36 modified by Lalle37 for the SITA Fast algorithm and Program 24-2, which describes the severity of loss in terms of the Mean Deviation (MD) visual field index and in terms of the number, severity, and proximity to fixation, of the Pattern Deviation probability symbols. One eye of each patient was analysed. The designated eye was that deemed to exhibit the severest visual field loss with the HFA based upon the MD index. The visual field result from the FDT for the corresponding eye was deemed to be abnormal if one or more stimulus locations were abnormal at, or below, the 1% probability level.
The field recorded with Program 24-2 of the HFA for the designated eye of each patient was then separately transformed based upon the Total and upon the Pattern Deviation probability scores at each location, respectively. The transformations were identical to that used by Asman and Heijl,38 which is the basis for the glaucoma hemifield test. A location exhibiting a probability value of P<0.05, P<0.02, P<0.01, or P<0.001 was assigned a corresponding value of 2, 5, 10, or 20, respectively.
The field recorded with Program C-20-1 of the FDT perimeter for the designated eye of each patient was evaluated in a similar manner based upon the three levels of abnormality. Mild relative loss (P≤0.01) was assigned a value of 10, moderate relative loss (P≤0.005) a value of 20, and severe loss an arbitrary value of 40.
Receiver operating characteristic (ROC) analysis and correlation coefficients were calculated using SPSS, Version 11. Spearman's rank correlation coefficient was calculated due to the non-Gaussian dispersion of the data.
Results
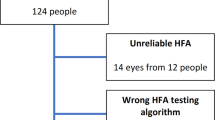
Of the 100 patients examined, 17 were excluded from the analysis; of these 17, six were due to non-glaucomatous ocular disease (including choroiditis, myopic degeneration, cerebral vascular accident, and advanced cataract), one due to tilted discs, and 10 due to a visual field examination in the designated eye deemed to be unreliable.
The majority of patients had previously attended the glaucoma clinic; however, approximately 30% were newly presenting patients. The mean age of the 83 patients was 67.3 years (SD 14.0 years). The analysis was based upon 42 right eyes and 41 left eyes.
Of the 83 eyes, 10 were deemed to be normal, 54 exhibited open-angle glaucoma, eight exhibited ocular hypertension, and 11 were deemed to be glaucoma suspects. Of the 54 patients with open-angle glaucoma, nine had normal tension glaucoma and 45 had high tension glaucoma. Table 1 summarises the characteristics of the fields from the HFA SITA Fast algorithm and Program 24-2, and from the FDT Program C-20-1, as a function of the clinical diagnosis. The HFA group mean MD for the open-angle glaucoma, glaucoma suspects, and ocular hypertensive patients was −7.60 (SD 8.21), −2.22 (SD 1.57), and −1.46 (SD 1.88) dB, respectively.
The outcome of the classification for Program 24-2 as a function of clinical diagnosis is shown in Table 2. The visual field classification in the designated eye comprised 27 patients exhibiting a normal visual field, 27 patients with mild, 11 with moderate, and 18 with severe glaucomatous visual field loss. Of the 27 eyes exhibiting a normal visual field, nine were from the patients with a normal clinical examination.
The outcome of the visual field examination with the HFA compared to that of the FDT as a function of clinical diagnosis is given in Table 3. The sensitivity and specificity as a function of clinical diagnosis is given in Table 4. The visual fields derived with the SITA Fast algorithm and Program 24-2 gave a sensitivity of 81.5% and a specificity of 83.3% compared to the clinical diagnosis for the combined category of glaucoma and glaucoma suspect against the combined category of normal and ocular hypertension. The sensitivity and the specificity improved to 88.9% and 90.0%, respectively, for the glaucoma category against the normal category, only. The visual fields derived with FDT Program C-20-1 exhibited a sensitivity and specificity of 66.2% and 83.3%, respectively, compared to the clinical diagnosis for the combined category of glaucoma and glaucoma suspect against the combined category of normal and ocular hypertension. The sensitivity improved to 74.1% if the glaucoma suspects and the patients with ocular hypertension were removed from the analysis.
The mean examination duration of all patients for the SITA Fast algorithm and Program 24-2 was 4.08 min (SD 1.14 min; range 159–453 s) compared with 1.11 min (SD 0.52 min; range 40–160 s) for Program C-20-1. The examination duration increased with increasing severity of visual field loss for both types of perimetric examination (Figure 1a and b). The examination duration with Program C-20-1 in the presence of a normal field was less than 60 s.
Using the criterion of one or more stimulus locations exhibiting abnormality at, or below, the 1% probability level, Program C-20-1 detected 85.2% of those normal fields recorded by the SITA Fast algorithm with Program 24-2, and detected 55.6%, 81.8%, and 100.0% of those with mild, moderate, and severe field loss, respectively. When the criterion was altered to two or more stimulus locations exhibiting abnormality at, or below, the 1% probability level, the corresponding figures were 92.6%, 51.9%, 63.6%, and 94.5%, respectively. If the criterion was altered to five or more stimulus locations exhibiting abnormality, then the FDT detected 92.6% of normal fields and 29.6%, 45.5%, and 61.1% of those with mild, moderate, and severe visual field loss, respectively. To achieve 100% specificity compared to the SITA Fast algorithm and Program 24-2, the criteria for failure with Program C-20-1 was six or more stimulus locations exhibiting abnormality.
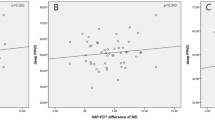
The probability score obtained with the FDT for the 17 stimulus locations correlated moderately with the MD of the SITA Fast Program 24-2 (ρ = 0.71; P≤0.001), The Pattern Standard Deviation (ρ = 0.63; P≤0.001), the Total Deviation probability score (ρ = 0.77; P≤0.001), and the Pattern Deviation probability score (ρ = 0.70; P≤0.01). However, the FDT probability score for each quadrant correlated less strongly with the equivalent HFA Total Deviation probability quadrant score: superior nasal ρ = 0.57; superior temporal ρ = 0.56; inferior temporal ρ = 0.70; inferior nasal ρ = 0.61 (P<0.001 in each case).
The ROC for the number of stimulus locations displaying abnormality and for the probability scores with the FDT compared to the severity classification of the visual fields derived by the SITA Fast algorithm yielded, in both cases, areas of 82.7% (P≤0.002).
Discussion
The principle findings of this study are two-fold. Firstly, perimetry undertaken with the HFA SITA Fast algorithm and Program 24-2 exhibits only moderate sensitivity and specificity compared to the clinical diagnosis, based upon stereoscopic examination of the optic disc, in the discrimination between normal and glaucomatous eyes exhibiting a diverse range of glaucomatous damage. Secondly, FDT Program C-20-1 yields an equivalent specificity to that of the SITA Fast algorithm and Program 24-2, but a reduced sensitivity, particularly for mild visual field loss.
The high specificity of the FDT is in agreement with other studies.2, 12, 22, 29, 30 Quigley2 reported a sensitivity of 91% and a specificity of 94% using a criterion of two or more stimulus locations exhibiting abnormality for Program C-20-1 compared to the HFA Full Threshold algorithm and Program 24-2 with abnormality designated in terms of the Glaucoma Hemifield Test. The specificity with Program C-20-1 in the current study was similar (93%) to that of Quigley,2 but the sensitivity was lower (68%) compared to the outcome with Program 24-2 when the identical criterion for abnormality was used.
The only study that has compared the performance of Program C-20-1 with the SITA Fast algorithm and Program 24-2 in a cohort of patients with glaucoma is that of Wadood et al22 who based their diagnosis of glaucoma solely on optic disc appearance. They found that the ROC area for the FDT was largest (93.9%) when abnormality was defined as one or more stimulus locations exhibiting abnormality. This area corresponded to a sensitivity and a specificity of 91% and 96%, respectively. These values are higher than those of the current study (74% and 90%), which were also based on optic disc appearance. In addition, it should be noted that the glaucomatous field loss was more advanced in the patients of Quigley2 and of Wadood and associates.22 The group mean MD was −14.2 dB (SD 8.6) and −10.34 dB (SD 6.5), respectively, in these latter two studies compared to −7.60 dB (SD 8.21) in the current study.
The degree of damage in the cohort under study will critically influence the diagnostic accuracy of the given test. Abnormality for the FDT, defined as one or more stimulus locations exhibiting abnormality, generated a specificity of 85% and sensitivities of 56%, 82%, and 100% for mild, moderate, and severe visual field loss, respectively. These latter values are similar to those of Trible et al12 who reported a 95% specificity and sensitivities of 39%, 86%, and 100% relative to the clinical diagnosis for mild, moderate and severe glaucomatous visual field loss, respectively.
The equivalent specificities and lower sensitivity than the SITA Fast algorithm and Program 24-2 are likely to be due, in part, to the larger size and lower spatial resolution of the FDT stimulus. The lower sensitivity and equivalent specificity to the SITA Fast algorithm and Program 24-2 would mitigate against the use of the FDT Program 20-1 in the community. However, the reduced sensitivity of the FDT has to be placed in the context of a notably longer examination duration of SITA Fast and Program 24-2. It will be of interest as to whether the smaller 5° stimulus, in conjunction with the 55 stimulus locations, of the corresponding Program 24-2-1 in the second-generation FDT, the Humphrey Matrix, will yield a higher sensitivity and specificity.
All individuals with normal fields completed Program C-20-1 in 59 s or less (mean (SD) 43.84 s (3.34)). These values lie between those previously reported.22, 29, 35 The mean examination durations for all individuals was 1.09 min and 4.10 min for Program C-20-1 and the SITA FAST algorithm with Program 24-2, respectively, which is similar to other studies.22, 35 Therefore, Program C-20-1 takes approximately 25% of the time of the SITA FAST algorithm and Program 24-2.
In agreement with others, we found a moderate correlation between the number of locations exhibiting abnormality with the FDT and the MD visual field index.2, 29 The depth and location of visual field loss with the FDT were also only moderately correlated with that of the HFA.
The increasing reliance upon the discrimination of optic nerve head abnormality for the diagnosis of glaucoma enabled the use of the high specificity Program C-20-1 rather than the higher sensitivity Program C-20-5. Despite this trend, knowledge of the extent of visual field damage still remains an essential prerequisite for the management of patients with glaucoma. The use of the high specificity Program C-20-1 was also compatible with the necessity to identify efficiently the high proportion of false-positive referrals to glaucoma clinics in general.39 In addition, the use of Program C-20-1 reduced the number of false-positive visual field outcomes. Nevertheless, the relatively poor performance of both types of perimetry in comparison to expert observation of the optic nerve head mandates the development and use of optic nerve head imaging technology with built-in confidence limits for normality. Such an approach should also reduce the number of inappropriate and/or later-stage referrals from the community.
The Humphrey Matrix also incorporates a screening program, N-30-1, which uses a 10° square stimulus and which is identical to that in the original FDT perimeter and similar to that of Program C-20-1 described here. It can be expected, therefore, that the results from the current study will be applicable to the Humphrey Matrix in this respect.
In conclusion, Program C-20-1 of the FDT perimeter is a rapid test taking approximately 25% of the time of the HFA Program 24-2 and the SITA Fast algorithm. It exhibits a high specificity in the detection of glaucoma similar to that of the HFA and high sensitivity for the detection of advanced field loss. However, the sensitivity of the FDT Program C-20-1 is low for the detection of mild loss.
References
Quigley HA, Sanchez RM, Dunkelberger GR, Lhernault NL, Baginski TA . Chronic glaucoma selectively damages large optic nerve fibres. Invest Ophthalmol Vis Sci 1987; 28: 913–920.
Quigley HA . Identification of glaucoma related visual field abnormality with the screening protocol of Frequency Doubling Technology. Am J Ophthalmol 1998; 125: 819–829.
Maddess T, Henry GH . Performance of non-linear visual units in ocular hypertension and glaucoma. Clin Vis Sci 1992; 7: 371–383.
Johnson CA, Samuels SJ . Screening for glaucomatous visual field loss with Frequency-Doubling perimetry. Invest Ophthalmol Vis Sci 1997; 38: 413–425.
Anderson RS, O’Brien CJ . Psychophysical evidence for a selective loss of M ganglion cells in glaucoma. Vis Res 1997; 37: 1079–1083.
Johnson CA . Selective versus non-selective losses in glaucoma. J Glauc 1994; 3: 532–544.
Kelly DH . Frequency doubling in visual responses. J Opthalmol Soc Am 1966; 56: 1628–1633.
Tyler CW . Observations on spatial-frequency doubling. Perception 1974; 3: 81–86.
Tolhurst DJ . Illusory shifts in spatial frequency caused by temporal modulation. Perception 1975; 4: 331–335.
Maddess T, Goldbert I, Dobinson J, Wine S, James AC . Clinical trials of the frequency doubled illusion as an indicator of glaucoma. Invest Ophthalmol Vis Sci 1995; 36: S335.
Burnstein Y, Ellish NJ, Magbalon M, Higginbotham EJ . Comparison of Frequency Doubling perimetry with Humphrey Visual Field Analyzer in a glaucoma practice. Am J Ophthalmol 2000; 129: 328–333.
Trible JR, Schultz RO, Robinson JC, Rothe TL . Accuracy of glaucoma detection with Frequency Doubling perimetry. Am J Ophthalmol 2000; 129: 740–745.
Cellini M, Torreggiani A . Frequency Doubling perimetry in ocular hypertension and chronic open angle glaucoma. Acta Ophthalmol Scand 2002; 80: 24–25.
Horikoshi N, Osako M, Tamura Y, Okano T, Usui M . Comparison of detectability of visual field abnormality by Frequency Doubling Technology in primary open-angle glaucoma and normal-tension glaucoma. Jpn J Ophthalmol 2001; 45: 503–509.
Sponsel WE, Arango S, Trigo Y, Mensah J . Clinical classification of glaucomatous visual field loss by Frequency Doubling perimetry. Am J Ophthalmol 1998; 125: 830–836.
Iester M, Altieri M, Vittone P, Calabria G, Zingirian M, Traverso CEI . Detection of glaucomatous visual field defect by non-conventional perimetry. Am J Ophthalmol 2003; 135: 35–39.
Cello KE, Nelson-Quigg JM, Johnson CA . Frequency Doubling Technology perimetry for detection of glaucomatous visual field loss. Am J Ophthalmol 2000; 129: 314–322.
Sample PA, Bosworth CF, Blumenthal EZ, Girkin C, Weinreb RN . Visual function-specific perimetry for indirect comparison of different ganglion cell populations in glaucoma. Invest Ophthalmol Vis Sci 2000; 41: 1783–1790.
Bowd C, Zangwill LM, Berry CC, Blumenthal EZ, Vasile C, Sanchez-Galeana C et al. Detecting early glaucoma by assessment of retinal nerve fiber layer thickness and visual function. Invest Ophthalmol Vis Sci 2001; 42: 1993–2003.
Wu LL, Suzuki Y, Kunimatsu S, Araie M, Iwase A, Tomita G . Frequency Doubling Technology and confocal scanning ophthalmoscopic optic disc analysis in open-angle glaucoma with hemifield defects. J Glaucoma 2001; 10: 256–260.
Serguhn S, Spiegel D . Comparison of Frequency Doubling perimetry and standard achromatic computerized perimetry in patients with glaucoma. Graefe's Arch Clin Exp Ophthalmol 2001; 239: 351–355.
Wadood AC, Azuara-Blanco A, Aspinall P, Taguri A, King AJW . Sensitivity and specificity of Frequency Doubling Technology, Tendency-Orientated Perimetry, and Humphrey Swedish Interactive Threshold Algorithm-fast perimetry in a glaucoma practice. Am J Ophthalmol 2002; 133: 327–332.
Iester M, Mermoud A, Schnyder C . Frequency Doubling technique in patients with ocular hypertension and glaucoma. Ophthalmology 2000; 107: 288–294.
Landers JA, Goldberg I, Graham SL . Comparison of clinical optic disc assessment with tests of early visual field loss. Clin Exp Ophthalmol 2002; 30: 338–342.
Martin L, Wanger P, Vancea L, Gothlin B . Concordance of High Pass Resolution Perimetry and Frequency Doubling Technology perimetry results in glaucoma: No support for selective ganglion cell damage. J Glaucoma 2003; 12: 40–44.
Kalaboukhova L, Lindblom B . Frequency Doubling Technology and High Pass Resolution Perimetry in glaucoma and ocular hypertension. Acta Ophthalmol Scand 2003; 81: 247–252.
Tatemichi M, Nakano T, Tanaka K, Hayashi T, Nawa T, Iwasaki A et al. Laterality of the performance of glaucoma mass screening using Frequency Doubling Technology. J Glaucoma 2003; 12: 221–225.
Kogure S, Toda Y, Crabb D, Fitzke FW, Tsukahara S . Agreement between Frequency Doubling perimetry and static perimetry in eyes with high tension glaucoma and normal tension glaucoma. Br J Ophthalmol 2003; 87: 604–608.
Patel SC, Friedman DS, Varadkar P, Robin AL . Algorithm for interpreting the results of Frequency Doubling perimetry. Am J Ophthalmol 2000; 129: 323–327.
Casson R, James B, Rubinstein A, Ali H . Clinical comparison of Frequency Doubling Technology perimetry and Humphrey perimetry. Br J Ophthalmol 2001; 85: 360–362.
Budenz DL, Rhee P, Feuer WJ, McSoley J, Johnson CA, Anderson DR et al. Sensitivity and specificity of the Swedish Interactive Threshold Algorithm for glaucomatous visual field defects. Ophthalmology 2002; 109: 1052–1058.
Nordmann JP, Brion F, Hamard P, Mouton-Chopen D . Evaluation odes programmes perimetriques Humphrey SITA Standard et SITA Fast chez les patients normaux et glaucomateux. J Fr Ophthalmol 1988; 21: 549–554.
Wild JM, Pacey IE, O’Neill EC, Cunliffe IA . The SITA perimetric threshold algorithms in glaucoma. Invest Ophthalmol Vis Sci 1999; 40: 1998–2009.
Wild JM, Pacey IE, Hancock SA, Cunliffe IA . Between-algorithm, between-individual differences in normal perimetric sensitivity: Full Threshold, FASTPAC, and SITA. Invest Ophthalmol Vis Sci 1999; 40: 1152–1161.
Allen CS, Sponsel WE, Trigo Y, Dirks MS, Flynn WJ . Comparison of the Frequency Doubling Technology screening algorithm and the Humphrey 24-2 SITA-Fast in a large eye screening. Clin Exp Ophthalmol 2002; 30: 8–14.
Hodapp E, Parrish RK, Anderson DR . Clinical Decisions in Glaucoma. CV Mosby: St Louis, MI, 1993.
Lalle PA . Evaluation of automated perimetry. In: Litvak AB (ed.). Glaucoma Handbook. Butterworth-Heinemann: Oxford, 2001, pp 97–167.
Asman P, Heijl A . Glaucoma Hemifield Test. Automated visual field evaluation. Acta Ophthalmol 1992; 110: 182–189.
Vernon SA, Ghosh G . Do locally agreed guidelines for optometrists concerning the referral of glaucoma suspects influence referral practice? Eye 2001; 15: 458–463.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented, in part, at the Association for Research in Vision and Ophthalmology, Fort Lauderdale, FL, USA in May 2002.
Rights and permissions
About this article
Cite this article
North, R., Jones, A., Hunter, E. et al. Evaluation of the high specificity Screening Program (C-20-1) of the Frequency Doubling Technology (FDT) perimeter in clinical practice. Eye 20, 681–687 (2006). https://doi.org/10.1038/sj.eye.6701946
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701946