Abstract
Aims
To study the incidence of cystoid macular oedema and changes in retinal thickness after phacoemulsification with optical coherence tomography (OCT).
Methods
In all, 131 eyes of 131 patients were studied at the ophthalmology clinic at Tung Wah Eastern Hospital from September 2001 to October 2002. All the patients had clinical assessment and OCT preoperatively and at weeks 2, 4, and 8 postoperatively. The incidence of postoperative cystoid macular oedema (CMO) was evaluated. The foveal thickness (FT) and central 1 mm retinal thickness (CT) at different time intervals were analysed.
Results
Four (3.05%) patients developed CMO after phacoemulsification, which was evident clinically and tomographically. Fluorescein angiogram confirmed leakage in all cases. For other patients, the mean preoperative FT was 189.36±26.83 μm. The mean FT, were 175.74±26.79 μm, 180.25±27.13 μm, 176.58±26.45 μm at 2 weeks, 4 weeks, and 8 weeks postoperatively, respectively. The preoperative FT was significantly thicker than those in the postoperative period. The same trend was noted for CT.
Conclusion:
OCT is useful for detecting and confirming clinical CMO after cataract surgery; however, its use in detecting subtle changes in retinal thickness is limited by the normal variation in retinal thickness. The measurement of retinal thickness with OCT may also be affected by the status of the lens.
Similar content being viewed by others
Introduction
Optical coherence tomography (OCT) is a relatively new method for high-resolution cross-sectional imaging of the retina that directly measures changes in the z-plane (depth of the retina). 1, 2, 3, 4 This method uses near-infrared light to detect relative changes in reflection at optical interfaces by the method of low-coherence interferometry. OCT has the advantages of being noninvasive, comfortable, and can be safely repeated as often as required.
OCT has been found to be useful for objectively monitoring retinal thickness in patients with macular oedema, macular holes, or epiretinal membranes,4 with a high degree of reproducibility and repeatability.3, 4, 5, 6, 7 Cystoid macular oedema (CMO) is an important complication of cataract extraction, with uncertain aetiology.8, 9, 10 OCT can demonstrate cystic changes and increased retinal thickness in patients with CMO.3, 4 As OCT has a high resolution of up to 10 μm, it may be able to detect subtle changes in retinal thickness that cannot be seen at clinical examination. However, retinal thickness measurement with OCT may be affected by a number of factors such as age, sex, race, body mass, axial length, or refractive state.5, 7, 11 As OCT measures the retardation of light at different optical media, the measurement may also be affected by the status of the ocular media, including the lens. At present, no adjustment is made by the machine for pseudophakia or aphakia. In this study, the incidence of CMO and changes in retinal thickness after phacoemulsification measured with OCT are examined and the usefulness of OCT to detect subtle CMO is evaluated.
Subjects and methods
In all, 131 eyes of 131 patients were recruited from the ophthalmology clinic at the Tung Wah Eastern Hospital in Hong Kong from September 2001 to October 2002. All patients were older than 50 years with cataracts that still permitted a clear fundal examination. Patients with other ocular pathologies were excluded from the study. The inclusion and exclusion criteria are shown in Table 1.
At 1 week before surgery, all patients underwent clinical assessment that included visual acuity, objective and subjective refraction, Amsler chart, intraocular pressure (IOP) measurement, and a dilated fundal examination. Past medical history was recorded. The presence of posterior vitreous detachment, foveal reflex, foveal depression, retinal thickening, or other retinal pathology was documented as a baseline.
OCT examination (OCT 2000 scanner, Humphrey Instruments, San Leandro, CA, USA) was carried out by an experienced operator through a dilated pupil. Six radial-line scans, 3.00 mm each in length, centred on the fovea were taken. Each scan contained 100 A-scan measurements equally spaced along each line. For patients who were unable to fixate on the foveal target, the operator could choose to offset the OCT to position the fovea onto the center of the scan. The images obtained had a laminar structure with two bands of high-intensity signal. The distance between the inner aspects of these bands was assumed to be a measure of retinal thickness, as in previous publications.2 Low-intensity spaces within the laminar structure were assumed to be cystoid spaces within the retina. The images acquired underwent processing by the retinal map analysis in the computer software in the OCT machine. The central foveal thickness (FT) was computed by averaging the retinal thickness at the central points of the six scans. The central 1 mm retinal thickness (CT) was also obtained from the A-scans by averaging the retinal thickness of a disc of 1 mm diameter centred on the fovea.
Phacoemulsification and intraocular lens insertion, using the same techniques, were performed using topical or retrobulbar anaesthesia. Clear corneal incision, continuous circular capsulorrhexis, and foldable acrylic lens insertion were performed. Sodium hyaluronate or chondroitin sulphate was used for lens implantation and was completely removed afterwards. No subconjunctival steroid, acetylcholine, or carbonic anhydrase inhibitor was given. Antibiotic and steroid eye drops and ointment were given postoperatively. Clinical assessment and OCT were performed at 2, 4, and 8 weeks postoperatively.
At each visit, if the scans taken were not satisfactory, they were repeated up to five times for each patient. The scans with the smallest SDs of the centre of the six radial lines were taken for analysis. The measurements were excluded from analysis if the best SD achieved in all five measurements was more than 50 μm. In 38 patients, the scans were repeated at the same visit to study intravisit variability. Fluorescein angiogram (FA) was performed for patients with topographic or clinical evidence of CMO or unexplained poor visual outcome.
Statistical analysis
Continuous variables, including preoperative and postoperative retinal thickness, were compared by paired t-test. The CT and FT of the different sexes were analysed with independent sample t-test. Comparisons of visual acuities in different groups were performed with the Mann–Whitney U test. The categorical data were analysed by χ2 test. The intrasubject and intravisit variability were assessed by Wilcoxon signed-rank test. Statistical tests were considered to be significant if P-values were less than 0.05.
Results
Among the 131 patients, 44 had diabetes mellitus. Four patients (3.05%) developed CMO with retinal thickening or cystic changes clinically. OCT confirmed the retinal thickening and cystic changes in all four patients, and all cases showed leakage on FA. One of these four patients had diabetes. The OCT images are shown in Figure 1. These patients were excluded from the analysis of retinal thickness. The CMO was first noted to be present at week 2 in one patient and at week 4 in three patients. The visual acuities of the patients were 0.2, 0.3, 0.3, and 0.3, respectively, when the CMO was detected. One of these four patients developed posterior vitreous detachment at week 4 postoperatively. There was no statistical difference between the occurrence rate of CMO in diabetic and nondiabetic patients, but the number of patients with CMO was too small for meaningful conclusion.
OCT images of the four patients with postoperative cystoid macular oedema. (a) In the first patient, the foveal thickness is 371±7 μm, the central 1 mm retinal thickness 308 μm at 2 weeks postoperatively. Visual acuity is 0.2. (b) In the second patient, the foveal thickness is 226±9 μm, the central 1 mm retinal thickness 252 μm at 4 weeks postoperatively. Visual acuity is 0.3. (c) In the third patient, the foveal thickness is 206±7 μm, the central 1 mm retinal thickness 223 μm at 4 weeks postoperatively. Visual acuity is 0.3. (d) In the fourth patient, the foveal thickness is 208±11 μm, the central 1 mm retinal thickness 233 μm at 4 weeks postoperatively. Visual acuity is 0.3.
After excluding the four patients with CMO, 127 eyes (69 right and 58 left) of 43 men (33.9%) and 84 women (66.1%) were included for analysis of retinal thickness. The mean age of the patients was 74.27 years (range, 55–86 years). The mean ages of men and women were comparable (P=0.153). The preoperative median visual acuity of the patients was 0.2 (range, 0.001–0.7). The median visual acuity improved to 0.6 (range, 0.2–1.0) at 8 weeks postoperatively. The preoperative and postoperative visual acuities are shown in Figure 2. The mean refractive errors were −1.28 diopters sphere (range, +4.50 to −5.50 diopters sphere) and 1.64 diopters cylinder (range, 0–6.25 diopters cylinder) preoperatively. The mean refractive errors at week 8 were 0.15 diopters sphere (range, +3.50 to −2.75 diopters sphere) and 1.36 diopters cylinder (range, 0–4.50 diopters cylinder). The high postoperative astigmatism was related to high pre-existing astigmatism. Eight patients (6.3%) had ruptured posterior capsules. Seven patients had the intraocular lens placed in the ciliary sulcus and one in the capsular bag. Among these eight patients, one patient was noted to have posterior vitreous detachment at 4 weeks postoperatively. None of these patients developed postoperative CMO.
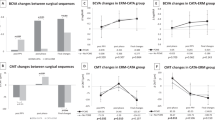
The mean preoperative FT of the patients was 189.36±26.83 μm. The mean FTs were 175.74±26.79 μm, 180.25±27.13 μm, 176.58±26.45 μm at 2 weeks, 4 weeks and 8 weeks postoperatively. The mean preoperative CT was 205.55±24.35 μm while the mean postoperative CTs were 196.11±24.36 μm, 201.02±24.86 μm, and 198.42±24.50 μm at week 2, week 4, and week 8, respectively (Table 2). The preoperative CT and FT were significantly thicker than those in the postoperative period (P<0.05) except when comparing the preoperative with the 4 weeks postoperative CT (P=0.124) (Table 3). The FT and CT vs time are shown in Figures 3 and 4. On comparison with the preoperative FT, 24 patients had a thicker FT at week 4 (mean 9.35±6.03 μm; range, 2.00–22.00 μm), but the patients with thicker FT did not have a poorer VA than those with thinner FT postoperatively (P=0.345) and none of these patients showed cystic changes onOCT.
Visual acuities at week 8 were not correlated with the FT (P=0.08) or CT (P=0.07). Changes in retinal thickness were also not correlated with changes in spherical equivalents (P=0.17 for FT, P=0.63 for CT). For the signal to noise (S/N) ratio, it showed statistically significant improvements after surgery by paired t-test when compared with preoperative period (P=0.009 for week 2, and P<0.005 for the week 4, and week 8 follow-up). The signal to noise ratios at different periods are shown in Figure 5.
Intrasubject variability
The SD of the six scans in each measurement was calculated by the OCT software. The mean of the SD within each measurement (intrasubject variability) was 16±10 μm (range, 2–46 μm), 13±8 μm (range, 2–41 μm), 14±8 μm (range, 2–50 μm) and 13±6 μm (range, 3–44 μm) for visits at weeks 0, 2, 4, and 8, respectively.
Intravisit variability
The measurements of 38 eyes were repeated during the same visit to assess intravisit variability in FT and CT. The mean absolute differences between two measurements were 8.8±8.8 μm (range, 0–36.0 μm) and 6.2±5.8 μm (range, 0–23.0 μm) for FT and CT, respectively. No statistically significant differences were found between two measurements for both FT (P=0.905) and CT (P=0.714) with Wilcoxon signed-rank test. Intraclass correlation coefficients were 0.94 (95% confidence interval (CI), 0.89–0.97) and 0.90 (95% CI, 0.82–0.95) for CT and FT, respectively.
Discussion
CMO is an important cause of reduced vision following cataract surgery with a variable incidence depending on the definition, timing of diagnosis, presence of surgical complications, and diagnostic method.8, 9, 10 It may be difficult to detect clinically and FA used to be the procedure of choice to confirm the diagnosis.12, 13 In some patients, FA may show leakage in the macula although the patient is asymptomatic.8 Compared with FA, OCT is noninvasive, comfortable, and safe, and can be repeated more frequently. In patients with uveitis, OCT is as effective as FA in detecting CMO but is more superior in demonstrating axial distribution of fluid.14 Ethically, it may not be justified to perform angiography to detect subclinical CMO for all postoperative cataract patients, but OCT can be safely performed and repeated to detect CMO that is not clinically obvious. Moreover, while FA may more effectively determine the presence and source of the oedematous fluid, increased retinal thickness has been found to correlate more strongly with reduced visual acuity than the presence of leakage on FA.13, 15, 16
Since OCT can achieve a high-resolution measurement of retinal thickness of up to 10 μm, it may be able to detect subtle changes in retinal thickness which is not clinically evident.4 For patients with diabetes mellitus, increased retinal thickness has been found in patients without clinical evidence of retinopathy or clinically significant macular oedema.16, 17 Previously, assessment of retinal thickening relied on subjective estimations by examination with stereoscopic microscopy, but biomicroscopy is unreliable for detecting central macular thickening smaller than approximately 100 μm.4 The advent of OCT has greatly improved the accuracy and reliability of the assessment of retinal thickness in an objective manner. This study shows that it has a high reproducibility and a low variability in measuring retinal thickness in cataract patients preoperatively and postoperatively. However, the examination failed in some patients, despite repeated attempts, due to poor patient fixation or poor media clarity. In patients with cataracts, OCT examination is more difficult and a more experienced operator is required.
To accurately assess changes in retinal thickness, it is first necessary todetermine the range of normal retinal thickness. In addition to the reliability of the measuring instrument, retinal thickness measurement can be affected by parameters such as axial length, body mass, age, sex, or race of the patients.5, 7, 16 Due to the normal variation in retinal thickness, a cutoff point has to be determined to differentiate abnormal thickening from normal thickness. Some studies used the upper range of a group of healthy eyes or three SDs greater than the mean value as the cutoff point.4, 16, 17 This approach, however, would produce false negative results for patients with thinner retinas. On the other hand, if a lower value is used, false positive results would be obtained for patients with thicker retinas. Our study shows that the standard deviation of retinal thickness is around 24–27 μm. Therefore, although OCT can theoretically give rise to a resolution up to 10 μm, measurement error and normal variation in retinal thickness in different individuals limit the value of OCT in detecting subtle changes in retinal thickness.
Our results show that the mean preoperative retinal thickness was significantly greater than the mean postoperative retinal thickness. It is usually thought that retinal thickness would be the same or increased after cataract surgery due to postoperative inflammation and it is not likely that surgery would cause a decrease in retinal thickness. Our findings may be explained by an error in preoperative measurements because of the presence of cataracts, or it may be due to an apparent thinning of the retina when the crystalline lens is replaced by an intraocular lens. Our study shows that the S/N ratio is increased in the postoperative visits. This may be due to an increase in noise in the cataractous eye which affects the measurement by OCT and the gradual improvement in the clarity of the media postoperatively. As OCT measures the retardation of light when traversing through different ocular media by comparing the reflected signal with a light source from a reference mirror, some structural or surface changes in the media may give rise to an artefact in measurements. If this is the case, some adjustment in retinal thickness measurement by the OCT may be required if the lens status is changed.
In this study, four (3.05%) of 131 patients developed CMO that was evident on OCT and clinical examination. All four patients showed leakage on FA examination. Improved surgical techniques with less postoperative inflammation may have reduced the incidence of postoperative CMO after phacoemulsifcation, especially clinically evident CMO. Ursell et al18 reported an incidence of 19% angiographic CMO after phacoemulsification. Although their patients with angiographic CMO had worse visual acuities than patients without CMO, no clinical CMO was seen in any patient with angiographic CMO at any postoperative visit. In our patients who showed some mild postoperative retinal thickening, there was no significant impairment in visual acuity. In a study of patients with uveitis, three of 128 eyes studied had CMO at FA but not at OCT while 108 eyes has similar results at OCT and FA.14 To our knowledge, no study comparing the incidence of postoperative CMO with OCT vs FA has been reported. However, because of the findings of retinal thinning after cataract surgery, further studies to verify these findings and to investigate how the lens status affects the retinal thickness measurement are advisable.
In conclusion, OCT is useful for detecting and confirming clinical CMO, but its value in detecting subclinical CMO is limited by the normal variation in retinal thickness and the possible effect of lens change on retinal thickness.
References
Huang D, Swanson EA, Lin CP, Schuman JS, Stinson WG, Chang W et al. Optical coherence tomography. Science 1991; 254: 1178–1181.
Hee MR, Izatt JA, Swanson EA, Huang D, Schuman JS, Lin CP et al. Optical coherence tomography of the human retina. Arch Ophthalmol 1995; 113: 325–332.
Puliafito CA, Hee MR, Lin CP, Reichel E, Schuman JS, Duker JS et al. Imaging of macular diseases with optical coherence tomography. Ophthalmology 1995; 102: 217–229.
Hee MR, Puliafito CA, Wong C, Duker JS, Reichel E, Rutledge B et al. Quantitative assessment of macular edema with optical coherence tomography. Arch Ophthalmol 1995; 113: 1019–1029.
Koozekanani D, Roberts C, Katz SE, Herderick ED . Intersession repeatability of macular thickness measurements with the Humphrey 2000 OCT. Invest Ophthalmol Vis Sci 2000; 41: 1486–1491.
Massin P, Vicaut E, Haouchine B, Erginay A, Paques M, Gaudric A . Reproducibility of retinal mapping using optical coherence tomography. Arch Ophthalmol 2001; 119: 1135–1142.
Muscat S, Parks S, Kemp E, Keating D . Repeatability and reproducibility of macular thickness measurements with Humphrey OCT system. Invest Opthalmol Vis Sci 2002; 43: 490–495.
Rossetti L, Autelitano A . Cystoid macular edema following cataract surgery. Curr Opin Ophthalmol 2000; 11: 65–72.
Rossetti L, Chaudhuri J, Dickersin K . Medical prophylaxis and treatment of cystoid macular edema after cataract surgery: the results of a meta-analysis. Ophthalmology 1998; 105: 397–405.
Norregaard JC, Bernth-Petersen P, Bellan L, Alonso J, Black C, Dunn E et al. Intraoperative clinical practice and risk of early complications after cataract extraction in the United States, Canada, Denmark, and Spain. Ophthalmology 1999; 106: 42–48.
Alamouti B, Funk J . Retinal thickness decreases with age: an OCT study. Br J Ophthalmol 2003; 87: 899–901.
Jaffe NS, Luscombe SM, Clayman HM, Gas JD . A fluorescein angiographic study of cystoid macular edema. Am J Ophthalmol 1981; 92: 775–777.
Dowler JGF, Sehmi KS, Hykin PG, Hamilton AMP . The natural history of macular edema after cataract surgery in diabetes. Ophthalmology 1999; 106: 663–668.
Antcliff RJ, Stanford MR, Chauhan DS, Graham EM, Spalton DJ, Shilling JS et al. Comparison between optical coherence tomography and fundus fluorescein angiography for the detection of cystoid macular edema in patients with uveitis. Ophthalmology 2000; 107: 593–599.
Nussenblatt RB, Kaufman SC, Palestine AG, Davis MD, Ferris FL .Macular thickening and visual acuity. Measurement in patients with cystoid macular edema. Ophthalmology 1987; 94: 1134–1139.
Hee MR, Puliafito CA, Duker JS, Reichel E, Coker JG, Wilkins JR et al. Topography of diabetic macular edema with optical coherence tomography. Ophthalmology 1998; 105: 360–370.
Sanchez-Tocino H, Alvarez-Vidal A, Maldonado MJ, Moreno-Montanes J, Garcia-Layana A . Retinal thickness study with optical coherence tomography in patients with diabetes. Invest Ophthalmol Vis Sci 2002; 43: 1588–1594.
Ursell PG, Spalton DJ, Whitcup SM, Nussenblatt RB . Cystoid macular edema after phaco emulsification. Relationship to blood-aqueous barrier damage and visual acuity. J Cataract Refract Surg 1999; 25: 1492–1497.
Author information
Authors and Affiliations
Corresponding author
Additional information
The authors have noial or proprietary interest commerct in any of the companies, products, or methods described in this article.
Rights and permissions
About this article
Cite this article
Ching, HY., Wong, A., Wong, CC. et al. Cystoid macular oedema and changes in retinal thickness after phacoemulsification with optical coherence tomography. Eye 20, 297–303 (2006). https://doi.org/10.1038/sj.eye.6701864
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701864
Keywords
This article is cited by
-
Phacoemulsification combined with micropulse cyclodiode laser in glaucoma patients: efficacy and safety
Eye (2022)
-
Comparison of macular thickness change by optical coherence tomography after uncomplicated cataract surgery in eyes with and without exfoliation syndrome
International Ophthalmology (2021)
-
Preoperative central macular thickness as a risk factor for pseudophakic macular edema
Graefe's Archive for Clinical and Experimental Ophthalmology (2021)
-
Early changes in retinal microcirculation after uncomplicated cataract surgery using an active-fluidics system
International Ophthalmology (2021)
-
Spectral-domain optical coherence tomography evaluation of postoperative cystoid macular oedema following phacoemulsification with intraoperative complication
BMC Ophthalmology (2014)