Abstract
Purpose
To evaluate the clinical and volumetric improvement 1 week after an injection of intravitreal triamcinolone acetonide in eyes with diabetic macular oedema.
Methods
Seven phakic eyes of seven diabetic patients diagnosed with clinically significant macular oedema were treated with a single 4-mg intravitreal injection of triamcinolone acetonide (0.1 ml). LogMAR best corrected visual acuity (logMAR BCVA), best corrected reading ability (RA), and central macular thickness (CMT) with optical coherence tomography (OCT) were assessed prior and 1 week subsequent to treatment.
Results
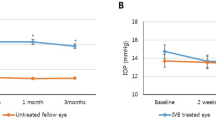
Mean improvement in logMAR BCVA was 0.146 (P=0.03). Mean reduction in CMT was 150.9 μm (P=0.02, Wilcoxon signed-rank test). Mean improvement in RA was 3 lines.
Conclusion
Reduction in macular oedema was demonstrated on OCT at 1 week, in most cases associated with improvement in central visual function, in particular, reading ability. Total resolution of diabetic macular oedema may occur at 1 week following intravitreal steroid injection.
Similar content being viewed by others
Introduction
Visual impairment in diabetes mellitus is commonly due to exudative maculopathy. Treatment for this condition traditionally involves argon laser photocoagulation,1 despite which many eyes lose vision over time.2 Recently, improvements in macular architecture and visual function, both with and without previous laser photocoagulation, have been demonstrated after intravitreal administration of triamcinolone,3, 4 the earliest recorded benefit having been at 1 month post-treatment.
At the Queen's Medical Centre, Nottingham we have been treating selected cases of diabetic macular oedema with intravitreal triamcinolone, since June 2002 (37 eyes of 32 patients). In our experience, patients often report early subjective visual improvement after intravitreal steroid administration.5 We therefore performed a retrospective case record review to assess whether such subjective benefit is accompanied by objective improvement of visual function and macular architecture.
Case series
Visual and anatomical improvement 1 week after pars plana injection of 4 mg of intravitreal triamcinolone (Kenalog, Squibb) under local anaesthesia with indirect ophthalmoscopic monitoring, were studied in seven phakic eyes of seven Type II diabetics with clinically significant macular oedema (Table 1).
Best-corrected visual acuity for distance (BCVA, LogMAR) and reading acuity (RA, Near Vision Test Type Chart, Faculty of Ophthalmologists, Clement Clarke) and central macular thickness (CMT) with optical coherence tomography (OCT) (Fast Macular Thickness Scan, Stratus/Zeiss OCT III) were assessed prior and 1 week subsequent to treatment.
Results
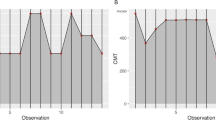
The subjects' ages ranged from 52 to 79 years (mean 66 years), while the duration of macular oedema ranged from 8 to 51 months (mean 19.6 months). Mean LogMAR BCVA improved by 0.146 from 0.58 to 0.43 (P=0.03), all patients except one exhibiting improvement. Mean near acuity improved by 3 lines. Mean CMT decreased by 150.9 μm from 490 to 339 μm (P=0.02, Wilcoxon-signed rank test) (Table 2).
Discussion
Diminution of near (reading) vision secondary to diabetic maculopathy is particularly debilitating. Our subjects universally experienced improvements in reading vision 1 week after treatment, associated with objective reduction of macular thickness on OCT. We are aware of only one previous study that has demonstrated improvements in reading ability after treatment (grid laser photocoagulation) for diabetic macular oedema.6
Closer inspection of our results reveal some interesting cases. Patient A experienced a 5-lines improvement in RA despite a mere 3.9% reduction in CMT. In contrast, patient G experienced improvements of 14 letters in LogMAR BCVA and 4 lines in RA associated with CMT reduction of 39%. Patient C achieved excellent RA (N5) mirrored by a normal appearing 1-week post-treatment OCT (Figure 1a and b).
Triamcinolone acetonide, a minimally water-soluble suspension, has interesting intravitreal pharmacokinetics, with considerable intersubject variation in peak concentrations achieved and elimination half-lives.7 The longevity of the therapeutic effect is correspondingly variable, vitrectomised eyes for example exhibiting a shorter elimination half-life. It is tempting to speculate whether the efficacy of treatment is related to the achieved (and maintained) intraocular concentrations of triamcinolone.
Intraocular pressure is known to rise following intravitreal triamcinolone8 and resolution of macular oedema may be related, in part, to this phenomenon. However, apart from transitory ocular hypertension in one case, our subjects remained normotensive, suggesting that visual and retinal thickness improvements are due either to disruption of the vitreous anatomy by the injection process or perhaps to a steroid effect on the retina.
Unresolved issues in relation to intravitreal triamcinolone remain, including the optimal dosage schedule and long-term safety/efficacy. We have demonstrated, to our knowledge for the first time, that both anatomical and functional improvement occurs earlier than previously recognised in the treatment of diabetic macular oedema with this treatment modality.
The mechanism of action of this agent however, remains an enigma.
References
Early treatment of diabetic retinopathy study report No. 1. Photocoagulation for diabetic macular oedema. Arch Ophthalmol 1985; 103: 1796–1806.
Lee CM, Olk RJ . Modified grid laser photocoagulation for diffuse diabetic macular oedema. Long term visual results. Ophthalmology 1991; 98(10): 1594–1602.
Martidis A, Duker JS, Greenberg PB, Rogers AH, Puliafito CA, Reichel E et al. Intravitreal triamcinolone for refractory diabetic macular oedema. Ophthalmology 2002; 109: 920–927.
Jonas JB, Kreissig I, Söfker A, Degenring RF . Intravitreal injection of triamcinolone for diffuse diabetic macular edema. Arch Ophthalmol 2003; 121: 57–61.
Negi A, Vernon SA, Lim C, Owen-Armstrong K . Intravitreal triamcinolone improves vision in eyes with chronic diabetic macular oedema refractory to laser photocoagulation. Eye, 2004, September 10 [E-pub ahead of print].
Mcnaught EI, Foulds WS, Allan D . Grid photocoagulation improves reading ability in diffuse diabetic macular oedema. Eye 1988; 2: 288–296.
Beer PM, Bakri SJ, Singh RJ, Liu W, Peters GB, Miller M . Intraocular concentration and pharmacokinetics of triamcinolone acetonide after a single intravitreal injection. Ophthalmology 2003; 110(4): 681–686.
Jonas JB, Kreissig I, Degenring R . Intraocular pressure after intravitreal injection of triamcinolone acetonide. Br J Ophthalmol 2002; 86: 1450–1451.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interest: None.
Rights and permissions
About this article
Cite this article
Islam, M., Negi, A. & Vernon, S. Improved visual acuity and macular thickness 1 week after intravitreal triamcinolone for diabetic macular oedema. Eye 19, 1325–1327 (2005). https://doi.org/10.1038/sj.eye.6701766
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701766