Abstract
Purpose
To retrospectively evaluate the incidence of cyclodeviation among patients with diplopia and analyse the causative diseases and clinical manifestations of cyclodeviation.
Methods
The medical records of 266 consecutive patients of 15 years of age or older presenting with diplopia, who had undergone the Lancaster red–green test (LRGT) from January 2001 to December 2002, were retrospectively reviewed. The presence of cyclodeviation on LRGT, predisposing conditions, causative diseases, and clinical manifestations of cyclotropia were analysed. Cyclodeviation on the LRGT were compared with those from the Maddox double-rod test (MDRT) and fundus photography.
Results
A total of 63 (24%) out of 266 patients exhibited cyclodeviation on LRGT. Eight out of 63 patients with cyclodeviation on the LRGT complained of torsional diplopia. Superior oblique palsy (SOP) was the most common causative disease (42 patients), followed by skew deviation (six) and thyroid orbitopathy (three). Excyclodeviation was found in 57 patients and incyclodeviation in four patients on the LRGT. The spontaneous recovery rate was 83% in patients of vascular origin and 17% of traumatic origin. Cyclodeviation with the MDRT and fundus photography showed good correlation with those obtained from the LRGT. There was no association of the amount of cyclotropia with the presence of torsional diplopia as well as with its recovery.
Conclusion
In spite of the rare complaint of torsional diplopia, 24% of the patients with diplopia showed cyclodeviation on the LRGT. SOP was the most common causative disease. Most of the patients with cyclodeviation of a vascular origin showed spontaneous improvement.
Similar content being viewed by others
Introduction
Cyclodeviation is defined as the rotation of an eyeball along the anteroposterior axis and cyclotropia as a misalignment of cyclodeviation between the two eyes.1 Patients with torsional deviations rarely complain of torsional diplopia,1, 2, 3 thus to the vast majority of ophthalmologists, cyclotropia has not been of significant concern. However, considering that cyclotropia cannot be corrected with prisms,2 the evaluation of cyclodeviation can be of considerable help in the diagnosis and management of the strabismus.
Even though a synoptophore examination may be one of the best indicators for a cyclodeviation, the Lancaster red–green test (LRGT) has some advantages over other tests in the evaluation of cyclodeviation: it measures the torsional amplitude of each eye in nine different directions of gaze, gives information about the pattern of cyclodeviation in each direction of gaze, and measures cyclodeviation simultaneously with the horizontal and vertical deviations. Therefore, it provides information about the three-dimensional positions and movement patterns of both eyes.4
To the best of our knowledge, there have been few reports in the literature in which the clinical characteristics of cyclotropia were evaluated and analysed using the LRGT. The purpose of this study was to evaluate the incidence of cyclotropia using the LRGT among patients presenting with diplopia and to analyse the causative diseases and clinical manifestations of cyclotropia.
Methods
The medical records of 266 consecutive patients of 15 years of age or older presenting with diplopia, who had undergone the LRGT from January 2001 to December 2002, were retrospectively reviewed. Since a high level of cooperation and understanding of the test was necessary, patients younger than 15 years of age were excluded.
Ophthalmic examinations, including the LRGT, alternate prism and cover test, duction/version test, and the Bielschowsky head tilt test were performed. The Maddox double-rod test (MDRT), fundus photography, and neuroimaging, including magnetic resonance imaging or computed tomography of brain, were performed in selected cases. Fundus photographs were taken through a dilated pupil 20–30 min after instillation of two drops of cyclopentolate and phenylephrine. We used the Topcon fundus camera equipped with the chin rest, head support, and internal fixation device. The photographer took care to observe that the patient’s head was straight while being photographed. The patient was fixated on the internal fixation device within the camera. For the majority of patients in the study, two photographs were taken of each eye at each photographic sitting. Each photograph was rated as being intorted, normal, or extorted. Eyes were considered intorted if the fovea was located above the upper border of the geometric lower 1/3 of the disc, eyes were considered extorted if the fovea was below the bottom of the disc, and eyes were considered normal if the fovea lay in an area between the geometric lower 1/3 of the disc.
The LRGT was performed as described in detail elsewhere in the literature.5 The quantitation of cyclotropia in the LRGT was performed as follows: the coordinates of bars in the Lancaster charts were obtained using the Photoshop program version 6.0® (Adobe, USA). The degree of cyclotropia was calculated using the function of arctangent in the Excel 2002 program (Microsoft, USA). The absolute degree of cyclotropia was measured in the primary (P) and in the downgaze (D). A difference of the degree of cyclotropia in the primary and in the downgaze (D–P) was calculated from the value of P and D. The minus value of D−P means larger degree of cyclotropia in the primary position than in the downgaze. The measured degree of cyclotropia of each patient was analysed in various conditions including superior oblique palsy (SOP) and the relationship of the degree of cyclotropia and the perception of torsional diplopia or with the recovery of diplopia was investigated. Measurements of cyclotropia obtained from the LRGT were compared with those obtained from the MDRT and from fundus photography. The causative diseases, predisposing conditions, incidence of excyclodeviation or incyclodeviation, and the clinical courses for each predisposing condition were also investigated.
Results
Among the 266 patients complaining of diplopia, 63 patients (24%) showed cyclotropia on the LRGT. Among the 63 patients with cyclotropia on the LRGT, only eight patients (13%) complained of torsional diplopia. The mean age of 63 patients with cyclotropia at the time of the LRGT was 48 years (15–77 years). In all, 41 of the patients with cyclotropia (65%) were male and 22 patients (35%) were female. The average follow-up period was 11 months (range from 0 to 96 months).
A comparison of the results of the LRGT with those of the MDRT and fundus photography is given in Table 1 and Figure 1. The correlation rate of the results obtained from the LRGT as compared with those obtained from the MDRT was 86% for excyclodeviation and 100% for incyclodeviation. Only three cases (14%) showed a discrepancy, in which no cyclodeviation was indicated in the MDRT, whereas the LRGT showed excyclodeviation. A comparison with the results of fundus photography showed that the LRGT exhibited a correlation rate of 83% for excyclodeviation and 100% for incyclodeviation. Only five cases (17%) showed no cyclodeviation based on fundus photography.
The causative diseases associated with cyclotropia, as diagnosed by the LRGT are summarized in Table 2. SOP was the most frequent causative disease (42 patients, 67%) associated with cyclotropia, followed by skew deviation (six patients, 10%) and thyroid orbitopathy (three patients, 5%).
The degree of cyclotropia in the Lancaster chart was measured in the primary position and downgaze. The mean degree of cyclotropia was 9.68° in the primary position (P) and 11.98° in downgaze (D) with a difference of 2.29° (D−P). In Table 3, there was no difference in the degree of cyclotropia in primary position and downgaze between SOP patients and the remaining patients. However, difference of the degree of cyclotropia between primary position and downgaze (D−P) was significantly larger in SOP patients. In all, 34 (81%) out of 42 SOP patients showed larger amount of cyclotropia in downgaze, whereas 10 (48%) out of 21 nonsuperior oblique palsy patients showed larger amount of cyclotropia in downgaze. Between unilateral and bilateral SOPs, the degree of cyclotropia in primary position (P) and downgaze (D) was significantly larger in the bilateral group, whereas the difference between primary position and downgaze (D−P) was similar between both groups (Table 3).
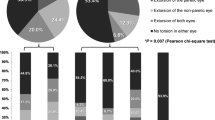
The predisposing conditions of cyclotropia were diverse. Vascular origin was the most common (24 patients, 38%), followed by trauma (21 patients, 31%). Vascular origin implies paralytic strabismus due to ischaemia or haemorrhage of the central nervous system without any history of trauma, and this occurred exclusively in the middle-aged and elderly patients (more than 40 years old in this study) with pre-existing hypertension or diabetes mellitus. Other predisposing conditions included dysthyroid orbitopathy (three patients, 5%), strabismus surgery (two patients, 3%), and neurosurgical operation (two patients, 3%) (Table 4).
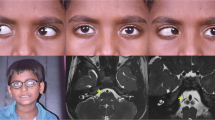
Excyclodeviation or excyclotropia was found in 57 patients (90.5%) and incyclodeviation or incyclotropia in four patients (6.4%) on the LRGT. Excyclodeviation and incyclodeviation in opposite eyes were found in two patients (3.1%). SOP was the most common cause of excyclodeviation, affecting 42 patients (74%). The causes of incyclodeviation included third nerve palsy, inferior rectus muscle palsy, dysthyroid orbitopathy involving multiple extraocular muscles, and sixth nerve palsy. The diverse patterns of cyclotropia on the LRGT in various diseases are depicted in Figure 2.
Patterns of cyclotropia on the Lancaster red-green test. (a) A case of right superior oblique palsy 4 months (upper) and 13 months (lower) after stroke (fourth ventricle hemorrhage). The amount and extent of cyclotropia decreased with time, although a small amount of cyclotropia remained in the inferior gaze. (b) A case of bilateral superior oblique palsy. A large amount of excyclotorion and alternating hypertropia were shown. (c) A case of left traumatic third nerve palsy. Incyclodeviation of the left eye was induced by unopposed superior oblique action. (d) A case of thyroid ophthalmopathy more on the right eye. An excyclodeviation was developed by restriction of right inferior rectus.
Diplopia was relieved with strabismus surgery in five patients. Among the 55 patients that we were able to follow-up for more than 6 months, 27 patients (49%) experienced spontaneous improvement of diplopia. The most frequent rate of spontaneous improvement of diplopia was observed in those patients whose cyclotropia was of vascular origin (19 out of 23 patients, 83%), whereas spontaneous recovery occurred in only three (17%) out of 18 patients whose predisposing condition was trauma.
The relationship between the amount of cyclotropia and the recognition of cyclotropia is depicted in Table 5. The degree of cyclotropia (P, D, D−P) had no statistically significant relationship with the presence and recovery of diplopia.
Discussion
Approximately a quarter of the patients (24%) presenting with diplopia showed cyclotropia on the LRGT. Only a few patients (13%) complained of torsional diplopia. The reason that so few patients perceived themselves as having torsional diplopia can be explained as follows: First, a large horizontal or vertical deviation might interfere with the patients’ ability to recognize torsional diplopia. Second, the patients might make use of an adaptive mechanism such as cyclofusion/cycloconvergence,3, 6 sensorial adaptation,7, 8, 9 or psychological adaptation1 in order to compensate the torsional component of their strabismus. Large peripheral Panum's fusional areas allow sensory cyclofusion of up to 8° and motor cyclofusion occurs in the presence of large-field stimuli, further helping to minimize problems from torsional diplopia both in normal individuals and in patients with ocular motor pareses.3 Third, most patients might not be aware of their having cyclotropia while carrying out daily activities in which binocular dissociation was not present, because the LRGT is such a dissociating test. Table 5 showed that the amount of cyclodeviation did not affect the perception of torsional deviation because there was no association between the degree of cyclodeviation and the perception of torsional diplopia.
The comparison of the results obtained from the LRGT with those obtained from the MDRT and fundus photography (Table 1 and Figure 1) demonstrated that there was good correlation in the evaluation of cyclodeviation. The main limitation of the LRGT in measuring cyclodeviation is that only the amount of cyclotropia and not the absolute amount of cyclodeviation in each eye can be measured.
Trobe investigated the prevalence of cyclotropia using the MDRT in patients with acquired vertical strabismus.10 He reported that cyclotropia was associated with SOP, dysthyroid ophthalmopathy, nondysthyroid restrictive ophthalmopathy, and myasthenia gravis, but not with skew deviation. Our study is unique in that we attempted to determine the prevalence of cyclotropia in patients presenting with all kinds of diplopia using the LRGT, to list the causative diseases associated with cyclotropia and to investigate the clinical courses. Moreover, the amount of cyclotropia of primary position and downgaze could be obtained in the Lancaster charts using the computer software program.
The LRGT showed advantage over MDRT and fundus photography in that the degree of cyclotropia could be measured in nine different directions of gaze. In the present study, the amount of cyclotropia of P and D were measured, but any nine directions of gaze could be measured in the Lancaster charts. Our results demonstrated that the difference of degree of cyclotropia between primary position and downgaze D−P in SOP patients was significantly larger than in other cyclotropia patients (Table 3). However, the actual amount of cyclotropia (P and D) had no difference. The comparison between unilateral and bilateral SOP patients showed that the number of eyes only made the difference in the degree of cyclodeviation but the degree of difference between D−P was the same. It can be assumed the D−P value is a marker for the involvement of superior oblique muscle and can be a tool in differentiating the cyclotropia patients whether the aetiology is SOP or not. However, it cannot differentiate the number of involved eyes in SOP patients.
There was a large difference in the rate of spontaneous improvement between those patients presenting with diplopia of traumatic origin and those whose diplopia was of vascular origin (17 vs 83%, respectively). This result corresponds with the previous reports.11, 12, 13 In our study, the amount of cyclodeviation obtained through the LRGT had no association with the recovery of symptoms (Table 4). This shows that the origin of cyclotropia is more important than the amount of cyclotropia in the improvement of cyclotropia.
In conclusion, diverse aspects of cyclotropia could be identified through the LRGT. The LRGT showed equally reliable results in comparison with the MDRT and fundus photography, and showed advantage of measuring the amount of cyclotropia in different directions of gaze. Even though patients with diplopia rarely complain of torsional diplopia, 24% of the patients with diplopia showed cyclodeviation on the LRGT. SOP was the most common causative disease and most of the patients with cyclodeviation of vascular origin showed spontaneous improvement.
References
von Noorden GK, Campos EC . Binocular Vision and Ocular Motility. Theory and Management of Strabismus, 6th ed. Mosby Inc.: Philadelphia, 2002 p 389.
von Noorden GK . Clinical and theoretical aspects of cyclotropia. J Pediatr Ophthalmol Strabismus 1984; 21: 126–132.
Guyton DL . Ocular torsion: sensorimotor principles. Graefe’s Arch Clin Exp Ophthalmol 1988; 226: 241–245.
Lancaster WB . Detecting, measuring, plotting, and interpreting ocular deviations. Arch Ophthalmol 1939; 22: 867–883.
Hwang JM, Guyton DL . The Lancaster red-green test before and after occlusion in the evaluation of incomitant strabismus. J AAPOS 1999; 3: 151–156.
Ruttom M, von Noorden GK . The Bagolini striated glass test for cyclotropia. Doc Ophthalmol 1984; 58: 131–139.
Olivier P, von Noorden GK . Excyclotropia of the nonparetic eye in unilateral superior oblique muscle paralysis. Am J Ophthalmol 1982; 93: 30–33.
Ruttum M, von Noorden GK . Adaptation to tilting of the visual environment in cyclotropia. Am J Ophthalmol 1983; 96: 229–237.
von Noorden GK . Clinical observations in cyclodeviations. Ophthalmology 1979; 86: 1451–1461.
Trobe JD . Cyclodeviations in acquired vertical strabismus. Arch Ophthalmol 1984; 102: 717–720.
Rush JA, Younge BR . Paralysis of cranial nerves III, IV, and VI. Cause and prognosis in 1000 cases. Arch Ophthalmol 1981; 99: 76–79.
Richards BW, Jones FR, Younge BR . Causes and prognosis in 4,278 cases of paralysis of the oculomotor, trochlear and abducens cranial nerves. Am J Ophthalmol 1992; 113: 489–496.
Tiffin PA, MacEwen CJ, Craig EA, Clayton G . Acquired palsy of the oculomotor, trochlear and abducens nerves. Eye 1996; 10: 377–384.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Woo, SJ., Seo, JM. & Hwang, JM. Clinical characteristics of cyclodeviation. Eye 19, 873–878 (2005). https://doi.org/10.1038/sj.eye.6701675
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701675
Keywords
This article is cited by
-
The effects of torsion on horizontal motor fusion and stereopsis
Scientific Reports (2023)
-
Development of a simple computerized torsion test to quantify subjective ocular torsion
Eye (2017)