Abstract
Aims
To establish if invasive and noninvasive uveal melanomas have differences in expression of adhesion molecules, and whether their adhesive interactions with the extracellular matrix (ECM) and endothelium vary.
Methods
Cells from an invasive and noninvasive uveal melanoma cell line and hepatic and dermal microvascular endothelial cells were assessed by flow cytometry for adhesion molecule expression. Tumour cell adhesion to ECM substrates (collagens I and IV, fibronectin, laminin, and vitronectin) and endothelial cells was also investigated using a commercially available assay or a fluorescence-based in vitro assay, respectively. The significance of results comparing cell lines was determined using a Student's t-test, whereby P-values of less than 0.05 were taken as significant.
Results
α1- and α4-integrins were not expressed by noninvasive cells, but were detected on invasive cells. The invasive cell line also expressed higher levels of other integrins than the noninvasive line. Correspondingly, invasive cells adhered in higher numbers to ECM substrates and endothelial cells, and for the latter, the difference was highly significant (P<0.001). No preference in adhesion of invasive cells for the hepatic endothelium was observed.
Conclusions
Successful attachment to and migration through the ECM, basement membrane, and endothelium are vital processes involved in malignant progression. Differential expression of α1- and α4-integrins by invasive and noninvasive cells infers a role for these receptors in invasion, while the ability of invasive cells to adhere more efficiently to the endothelium suggests that this is a critical factor in uveal melanoma invasion.
Similar content being viewed by others
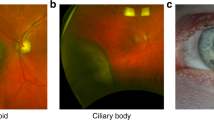
Introduction
During metastasis, tumour cells disperse via the vasculature and the lymphatic systems, undergoing intravasation and extravasation before finally invading and growing at secondary sites. For uveal melanoma however, dissemination via the vasculature is of primary importance as lymphatic vessels are absent from the eye. In addition, networks of extracellular matrix (ECM) channels have been identified in aggressive uveal melanomas, which could also assist in the dispersal of this malignancy.1 To undertake successfully the stages required for dissemination, tumour cells must be able to adhere to, and subsequently detach from components of the ECM and basement membrane (BM) such as collagens, fibronectin, and laminin, and ultimately the vascular endothelium. Adhesion molecules, expressed by both the tumour and endothelium, mediate these adhesive interactions, and more specifically integrins are thought to be particularly important in cancer metastasis, forming a major group of adhesion molecules coordinating ECM and cell–cell interactions.2
Integrins are a family of heterodimeric glycoproteins consisting of α and β subunits, linking the cytoskeleton with the ECM or adjacent cells. Changes in integrin expression have been reported during the malignant progression of many tumours3 and much evidence exists implicating their involvement in cutaneous melanoma metastasis.4 For example, altered αvβ and α5β1 expression has been described during the progression of metastatic melanoma cells,5, 6 while the presence of α4β1 receptors, involved in attachment to the endothelium, promotes the accumulation of disseminated cells in distant organs.7, 8 Highly metastatic melanoma cells also adhere well to the ECM proteins type IV collagen and laminin, and blocking α3β1 integrins prevents in vitro invasion through artificial BMs.9, 10, 11 Together, this would suggest that the ability of melanoma cells to metastasise is reflected in their capacity to adhere to the ECM and endothelium.
Although both cutaneous and uveal melanomas are similarly derived from neuroectodermal tissue, their metastatic behaviour in the body differs greatly. In particular, while cutaneous melanomas metastasise widely, uveal melanomas commonly spread to the liver and other sites are less frequently affected. Uveal melanomas are reported to express a range of adhesion molecules, including integrins, and members of the immunoglobulin family members,6, 12, 13, 14, 15 but only the expression of intercellular cellular molecule-1 (ICAM-1) has so far been shown to bear any relationship to clinical outcome.15 Little is, however, known about how adhesion molecule expression in uveal melanomas may influence the invasion process, and it is unclear whether the same mechanisms important in cutaneous melanoma are equally relevant, or if different interactions are required. In this investigation, we therefore undertook to study the differences in the adhesive interactions between invasive and noninvasive uveal melanoma with ECM proteins and cells of the vasculature.
Materials and methods
Cell culture
The invasive (SOM 196B) and noninvasive (SOM 157d) uveal melanoma cell lines were derived from samples obtained from primary posterior uveal melanomas upon enucleation, and were confirmed for melanoma status and maintained as previously described.16, 17 Levels of invasion had been previously quantified using an in vitro Matrigel invasion assay.17 Ethical approval was obtained prior to study, and protocols adhered to the principles of the Declaration of Helsinki. Human dermal microvascular endothelial cells (adult) (HDMECAs) were obtained commercially (TCS Cellworks Ltd, UK), while human liver sinusoidal endothelial cells (HuLiSECs) were freshly extracted from liver resections and maintained as detailed before.17, 18 The invasive cutaneous melanoma cell line A37519 was maintained in Dulbecco's minimal medium (Invitrogen, UK) containing 10% foetal calf serum.
ECM adhesion assays
Adhesion of uveal melanoma cells to ECM proteins (collagen type I, collagen type IV, fibronectin, laminin, and vitronectin) was assessed using a CytoMatrixTM screening kit (Chemicon International, CA, USA). Briefly, wells coated with human ECM protein were rehydrated with phosphate-buffered saline (PBS) (Oxoid Ltd, Hampshire, UK), and nonspecific binding was blocked with 1% bovine serum albumin (BSA). Cells were nonenzymatically disaggregated from culture flasks using cell dissociation solution (Sigma-Aldrich, Dorset, UK), and resuspended at a concentration of 5 × 105 cells/ml in RPMI-1640 with 0.1% BSA. Cell suspension (100 μl) was added to each well, and the plate was incubated at 37°C for 1 h. Plates were carefully washed by hand three times with PBS, and stained with 0.2% crystal violet in 10% ethanol for 5 min. Wells were manually washed a further three times before adding a solubilisation buffer of equal volumes of 0.1 M NaH2PO (pH 4.5) and 50% ethanol. Levels of adhesion were determined by assessing the absorbance at 540 nm on a microplate reader (Dynex Technologies Inc., VA, USA). The data were collected and analysed using RevelationTM software (Dynex Technologies Inc., VA, USA). Triplicate wells were assessed for each treatment; experiments were repeated three times and the mean value was calculated. In all cases, adhesion to wells coated with BSA acted as negative controls, and levels of adhesion to ECM substrates were assessed relative to the controls.
Inhibition of adhesive interactions with the ECM using integrin-blocking antibodies
To block integrin-mediated adhesion to the ECM, uveal melanoma cells were preincubated with the relevant anti-integrin blocking mouse monoclonal antibodies (mAb) (Table 1), diluted in RPMI-1640 supplemented with 0.1%. BSA at a range of concentrations, for 30 min at room temperature prior to the ECM adhesion assay (as described above). With the exception of the negative control antibody, all mAbs were purchased from Chemicon International Inc. (Harrow, UK). A negative IgG1 isotype control antibody (DakoCytomation, Ely, UK) was included in each assay, and results were expressed as a percentage reduction in adhesion when compared with negative controls. As ICAM-1 and α4-integrins are reported to be primarily involved in tumour–tumour and tumour–endothelial attachment, respectively, the effect of blocking these adhesion molecules on ECM binding was not assessed. Inhibition experiments were also only carried out for integrins for which levels of expression were deemed sufficiently high to enable successful antibody blocking.
Flow cytometry
Levels of integrin and ICAM-1 expression by uveal melanoma cells and VCAM-1 and E-selectin by endothelial cells were assessed using flow cytometry (FACSort Vantage) (Beckton Dickinson, NJ, USA) (Table 1). Expression was detected by the use of appropriate FITC-labelled secondary antibodies (Table 1) with a band pass filter (BP530/30). The data were collected and analysed using Cell QuestTM software (Beckon Dickinson, NJ, USA), assessing the median values of fluorescence. Test samples were run against a control sample, labelling cells with a negative IgG1 isotype control antibody. Results were expressed as the relative median fluorescent intensity (MFI), comparing test with control samples. Relative MFI values of greater than 2 were taken as positive, as expression levels were considered to have doubled. Experiments with SOM 157d and SOM 196B were repeated three times and a mean calculated.
Endothelial adhesion assays
To study the adhesive interactions between endothelial and SOM 157d and SOM 196B, HDMECAs or HuLiSECs (2 × 104/well) were grown to confluence in a 96-well plate, precoated with gelatin, for 24 h. Prior to setting up the adhesion assay, the growth medium was removed from the wells and the cells were washed twice with PBS. Adhesion of A375 cells was used as a comparison with a cutaneous melanoma cell line.
Tumour cells were labelled with carboxy-fluorescein diacetate, succinimidyl ester (CFDA-SE) (5 μM) (Molecular Probes Inc., OR, USA) (fluorescing at 492–517 nm)17 following the manufacturer's instructions. Cells were then resuspended at a concentration of 5 × 105/ml in RPMI-1640 with 0.1% BSA, and 50 μl of the cell suspension (25 × 103/well) was pipetted into each well containing the endothelial cell layer. Plates were incubated at 37°C for 4 h. At 5 min prior to the end of the incubation period, endothelial cells were counterstained with Hoescht (33342) (10 μM) (Sigma-Aldrich, Dorset, UK) and replaced in the incubator. Any nonadherent cells were carefully removed through gentle pipetting and plates were washed three times manually with PBS. Cells were fixed with 4% formaldehyde/PBS for 15 min, before rinsing in distilled water and air-drying overnight in a dark, dry atmosphere. Levels of adhesion were determined by assessing the absorbance at 510 nm on a microplate reader (Denley, Stevenage, UK). The data were collected and analysed using Wellfluor Data CaptureTM software (Denley, Stevenage, UK). Six wells were analysed for each condition and experiments were repeated three times and a mean calculated. In all cases, adhesion to wells coated with fibronectin (15 μg/ml) acted as positive controls, while for negative controls no tumour cells were added to endothelial cell monolayers. Levels of adhesion to endothelial cells were assessed relative to the controls.
Statistical analysis
A Student's t-test was used to compare population means of adhesion assay data, analysing treatment values against an appropriate control. Due to the presence of low absorbance units when assessing the adhesion to ECM proteins, the variance in the data obtained was found to be heterogeneous, and consequently a square root transformation was applied (√(x+0.5)). Comparisons between results with SOM 196B and SOM 157d and between results with HDMECAs and HuLiSECs were similarly statistically assessed using the Student's t-test. In all cases, P-values of less than 0.05 were taken as significant and were used to establish the fact that cellular adhesion was significantly increased, or decreased, compared to the respective control level. As experiments were repeated three times assessing triplicate values, there is only a small possibility that the significant differences observed would have occurred by chance.
Results
Adhesion molecule expression
Basal levels of expression of adhesion molecules by SOM 196B and SOM 157d assessed by flow cytometry are shown in Table 2. In summary, both uveal melanoma cell lines were negative for ICAM-1 expression. Invasive SOM 196B cells expressed high levels of the integrin subunits α1, α2, α3, α5, and α6, while only being weakly positive for α4 and αvβ3. The noninvasive SOM 157d similarly expressed α2, α3, α5, and α6, and low levels of αvβ3, and in contrast to SOM 196B, was negative for both α1 and α4 expression. For those integrins detected, the levels of expression were notably higher for SOM 196B when compared with SOM 157d, apart from αvβ3 that was comparable. Neither E-selectin nor VCAM-1 was detected on dermal or hepatic endothelial cells (data not presented in Table 2).
Adhesion to ECM proteins and inhibition studies
Similar patterns of adhesion to ECM proteins were seen for both cell lines (Figure 1), and with the exception of vitronectin, invasive SOM 196B adhered at higher levels than noninvasive SOM 157d, but levels did not reach significance (P>0.05). When compared with negative controls, both cell types preferentially adhered to fibronectin (P<0.01). Preincubation with anti-integrin-blocking antibodies established that attachment was primarily via α3-integrins (Table 2). Blocking the α5-subunit and the αvβ3 receptor on SOM 196B cells also partially decreased adhesion (Table 2). Both uveal melanoma cell lines also attached in significant numbers to laminin (P<0.01), and vitronectin (P<0.05) via α6- and αvβ3-integrins, respectively (Table 2), when comparing with control levels to BSA. In addition, SOM 196B but not SOM 157d adhered to both collagens I and IV (P<0.01) and this proved to be principally mediated through α2-subunits, and to a lesser extent by means of the α1- and α3-subunits (Table 2).
Adhesion of SOM 196B and SOM 157d to ECM proteins. The levels of cell adhesion were measured using 0.2% crystal violet staining. Following staining and washing, the retained dye was solubilised and measured at an absorbance at 560 nm. Wells coated with BSA acted as negative controls. The bars show the mean (±SEM) absorbency at 560 nm for three experiments. The x-axis shows the substrate and the y-axis shows the absorbance at 560 nm. **P<0.01 and *P<0.05 when comparing adhesion to ECM proteins with negative controls. SOM: Sheffield ocular melanoma; ECM: extracellular matrix.
Adhesion to endothelial cells
Due to the preferential binding of both SOM 157d and SOM 196B to fibronectin observed in ECM adhesion assays (Figure 1), this substrate was used as a positive control in the endothelial adhesion assays, allowing comparison with attachment to the endothelium. In common with adhesion to ECM substrates (Figure 1), the invasive SOM 196B line was more adherent than the noninvasive SOM 157d line (P<0.001) and the cutaneous melanoma A375 line to both microvascular endothelial cell types (Figure 2). No preference for hepatic endothelial cells (HuLiSECs) was, however, shown by the invasive SOM 196B cells, and cells attached in similar numbers to both hepatic and dermal (HDMECAs) endothelial cells (P>0.05) (Figure 2). All melanoma cells studied nevertheless adhered in higher numbers to the ECM substrate fibronectin than to the endothelium (P>0.05) (Figure 2).
Adhesion of the uveal melanoma cell lines SOM 196B and SOM 157d and the cutaneous melanoma cell line A375 to fibronectin (Fn), HDMECAs, and (HuLiSECs). Mean (± SEM) number of tumour cells adhering to Fn or different endothelial cell types. Results represent the mean of three experiments. Units of fluorescence at 510 nm are measured on the y-axis. No significant differences in adhesion of SOM 196B, SOM 157d and A375 cells to fibronectin were observed (P>0.05) when compared with adhesion to either HDMECAs or HuLiSECs. When comparing adhesion to either endothelial cell types between tumour cell types, significantly higher levels of SOM 196B cells adhered to both HDMECAs and HuLiSECs, when compared with SOM 157d (P<0.001).
Discussion
Uveal melanomas are highly aggressive tumours predominantly metastasising to the liver,20 with the most aggressive tumours possessing the ability to invade through the surrounding matrix, the underlying BM and into the vasculature and establish secondary disease. Similarly in vitro, uveal melanoma cells also demonstrate differences in invasive abilities through BM and endothelial barriers17 and we have correspondingly shown in this present study that invasive cells express higher integrin levels and are more adherent than their noninvasive counterparts to both the ECM and cells of the vasculature (Figures 1 and 2).
A previous study carried out in this laboratory associated expression of α1-, α4- and α6-integrins by uveal melanomas with the more aggressive phenotype.13 In this present study, a similar pattern of α1- and α4-expression was observed between invasive and noninvasive cells (Table 2), while lower levels of α6-expression were detected on noninvasive cells when compared with their invasive counterparts (Table 2). Together, these data support an involvement of these receptors with malignant progression and the invasive phenotype previously demonstrated.6, 13, 17 In this current study, inclusion of blocking antibodies in ECM adhesion assays identified that α1- and α6-integrins on SOM 196B cells are involved with attachment to collagens I and IV and laminin (Table 2), with these cells correspondingly adhering at higher levels to these substrates than noninvasive SOM 157d (Figure 1). As both laminin and collagen type IV are found in high levels in the BM, and premetastatic uveal melanoma cells, associated with a better prognosis, lack laminin receptors,21 this would similarly infer an involvement of α1- and α6-integrins with uveal melanoma invasion. Also in view of the phenomenon of networks of nonendothelial channels in uveal melanoma that are rich in laminin,1 increased expression by aggressive uveal melanomas of laminin-binding integrins may facilitate dispersal by such means.
On migrating through the surrounding ECM and BM, malignant cells further invade through the vessel wall (‘transendothelial migration’), ultimately facilitating dissemination. To establish secondary colonies successfully, this process must be accomplished at both the primary and secondary sites.22 As described earlier, using an in vitro transendothelial invasion assay, we have shown that invasive SOM 196B cells invade through the BM and endothelium in greater numbers than noninvasive SOM 157d.17 Correspondingly in this present study, SOM 196B was significantly more adherent to both endothelial cells types than SOM 157d (P<0.001) (Figure 2); similar interactions with endothelial cells have also been reported for lymphoma cells in vitro.23
Both uveal melanoma cell types were, however, less adherent to the endothelium than to the ECM substrate fibronectin. This observation was reflected in the previous invasion study whereby comparison of BM invasion with transendothelial invasion identified a significant reduction in numbers of cells invading by inclusion of the endothelial layer (P>0.05).17 Together with the current findings of a highly significant difference between the number of invading and noninvading cells adhering to the endothelium (P<0.001), these results would suggest that adhesion to the endothelium is a more specific event, requiring a more malignant phenotype than attachment to the ECM. As a consequence, the ability of invasive uveal melanoma cells to adhere efficiently to the endothelium could be a critical factor in invasion. In support, studies on prostate carcinoma, a tumour frequently metastasising to the bone, have shown that adhesion of tumour cells to bone is regulated by direct attachment to the endothelium in preference to the ECM,24 similarly implying that adhesion to the vasculature is a crucial stage in prostate carcinoma metastasis.
As prostate carcinoma cells in vitro have also been reported to adhere to primary bone marrow endothelium in higher numbers than to other endothelial cell types,25, 26 this present study also investigated the possibility that uveal melanoma cells preferentially attach to hepatic endothelial cells. Despite the selective targeting of uveal melanoma cells to the liver in vivo,19 uveal melanoma cells, however, had no significant preference for hepatic endothelial cells (HuLiSECs) (P>0.05). Instead, the invasive uveal melanoma cell line adhered in greater numbers to HDMECAs (P>0.05) (Figure 2); a direct explanation for this preference remains uncertain, but did indicate differential attachment to the two endothelial cell types. Adhesion molecules involved in tumour–endothelial interactions can, however, vary depending upon static or hydrodynamic conditions in vivo27, 28 and the microenvironment29, 30, 31, and as the in vitro assay system used in this study was static, this may have affected the patterns of adhesion observed.
With the exception of α4-integrins, ICAM-1, E-selectin, and VCAM-1, all adhesion molecules studied are primarily involved with tumour attachment to the ECM. In contrast, the aforementioned adhesion molecules all mediate either tumour–endothelial or tumour–tumour interactions. Expression of ICAM-1 has been associated with an increased risk of uveal melanoma metastasis15 and worse prognosis in cutaneous melanoma,4, 32 and similarly invasive cells studied here expressed higher levels than their noninvasive counterparts (Table 2), also implicating an involvement of ICAM-1 in invasion. As described previously, both uveal melanocytes13 and noninvasive cells do not express α4-integrins, while increased levels were detected on invasive cells (Table 2). Although little is known about α4-integrins and uveal melanoma metastasis, ligation of α4β1 with its endothelial ligand VCAM-1 is involved with cutaneous melanoma metastasis,7 and the pattern of spread is proposed to relate to organ-specific VCAM-1 expression.8 Moreover, E-selectin is reported to mediate colorectal tumour cell adhesion to the hepatic endothelium.29, 33 Both endothelial cell types studied here nevertheless lacked expression of E-selectin and VCAM-1, but as inflammatory regulators upregulate their expression,29, 30 their involvement in uveal melanoma attachment to the endothelium cannot be excluded. Further studies are nevertheless required to validate the importance of these adhesion molecules in uveal melanoma metastasis.
In summary, we have demonstrated here that invasive uveal melanoma cells adhere in higher numbers to ECM substrates and cells of the vasculature than noninvasive cells. The highly significant difference (P<0.001) in numbers of invasive and noninvasive cells attaching to the endothelium would suggest that adhesion to the vasculature is vital in determining the invasive phenotype. The absence of α1- and α4-integrins on noninvasive cells and uveal melanocytes,13 mediating the adhesive interactions studied, would infer a vital role for these receptors in uveal melanoma invasion. Further investigation into the factors regulating these interactions is required to improve an understanding of uveal melanoma metastasis.
References
Hendrix MJ, Seftor EA, Kirschmann DA, Quaranta V, Seftor RE . Remodeling of the microenvironment by aggressive melanoma tumor cells. Ann N Y Acad Sci 2003; 995: 151–161.
Hart IR, Saini A . Biology of tumour metastasis. Lancet 1992; 339: 1453–1457.
Zetter BR . Adhesion molecules in tumour metastasis. Sem Cancer Biol 1993; 4: 219–229.
Johnson JP . Cell adhesion molecules in the development and progression of malignant melanoma. Cancer Metastasis Rev 1999; 18(3): 345–357.
Danen EH, Ten Berge PJ, Van Muijen GN, Van ‘t Hof-Grootenboer AE, Brocker EB, Ruiter DJ . Emergence of alpha 5 beta 1 fibronectin- and alpha v beta 3 vitronectin-receptor expression in melanocytic tumour progression. Histopathology 1994; 24(3): 249–256.
Seftor RE, Seftor EA, Hendrix MJ . Molecular role(s) for integrins in human melanoma invasion. Cancer Metastasis Rev 1999; 18(3): 359–375.
Holzmann B, Gosslar U, Bittner M . Alpha 4 integrins and tumor metastasis. Curr Top Microbiol Immunol 1998; 231: 125–141.
Langley RR, Carlisle R, Ma L, Specian RD, Gerritsen ME, Granger DN . Endothelial expression of vascular cell adhesion molecule-1 correlates with metastatic pattern in spontaneous melanoma. Microcirculation 2001; 8(5): 335–345.
Danen EH, van Muijen GN, van de Wiel-van Kemenade E, Jansen KF, Ruiter DJ, Figdor CG . Regulation of integrin-mediated adhesion to laminin and collagen in human melanocytes and in non-metastatic and highly metastatic human melanoma cells. Int J Cancer 1993; 54(2): 315–321.
Yoshinaga IG, Vink J, Dekker SK, Mihm Jr MC, Byers HR . Role of alpha 3 beta 1 and alpha 2 beta 1 integrins in melanoma cell migration. Melanoma Res 1993; 3(6): 435–441.
Melchiori A, Mortarini R, Carlone S, Marchisio PC, Anichini A, Noonan DM et al. The alpha 3 beta 1 integrin is involved in melanoma cell migration and invasion. Exp Cell Res 1995; 219(1): 233–242.
Baker JK, Elshaw SR, Mathewman GE, Nichols CE, Murray AK, Parsons MA et al. Expression of integrins, degradative enzymes and their inhibitors in uveal melanoma: differences between in vitro and in vivo expression. Melanoma Res 2001; 11(3): 265–273.
Elshaw SR, Sisley K, Cross N, Murray AK, MacNeil SM, Wagner M et al. A comparison of ocular melanocyte and uveal melanoma cell invasion and the implication of alpha1beta1, alpha4beta1 and alpha6beta1 integrins. Br J Ophthalmol 2001; 85(6): 732–738.
Anastassiou G, Schilling H, Djakovic S, Bornfeld N . Expression of VLA-2, VLA-3, and alpha(v) integrin receptors in uveal melanoma: association with microvascular architecture of the tumour and prognostic value. Br J Ophthalmol 2000; 84(8): 899–902.
Anastassiou G, Schilling H, Stang A, Djakovic S, Heiligenhaus A, Bornfeld N . Expression of the cell adhesion molecules ICAM-1, VCAM-1 and NCAM in uveal melanoma: a clinicopathological study. Oncology 2000; 58(1): 83–88.
Woodward JK, Elshaw SR, Murray AK, Nichols CE, Cross N, Laws D et al. Stimulation and inhibition of uveal melanoma invasion by HGF, GRO, IL-1alpha and TGF-beta. Invest Ophthalmol Vis Sci 2002; 43(10): 3144–3152.
Woodward JK, Nichols CE, Rennie IG, Parsons MA, Murray AK, Sisley K . An in vitro assay to assess uveal melanoma invasion across endothelial and basement membrane barriers. Invest Ophthalmol Vis Sci 2002; 43(6): 1708–1714.
Burn JL, Greaves CL, Majeed AW, Bird NC . Human liver sinusoidal endothelial cell (HuLiSEC) culture. Clin Metastasis 2000; 17(9): 774.
Gehlsen KR, Davis GE, Sriramarao P . Integrin expression in human melanoma cells with differing invasive and metastatic properties. Clin Exp Metastasis 1992; 10(2): 111–120.
Char DH . Metastatic choroidal melanoma. Am J Ophthalmol 1978; 86(1): 76–80.
Rohrbach JM, Wild M, Riedinger C, Kreissig I, Thiel HJ . Premetastatic uveal melanoma cells do not express laminin receptors. Ger J Ophthalmol 1994; 3(3): 144–147.
Voura EB, Sandig M, Siu CH . Cell–cell interactions during transendothelial migration of tumor cells. Microsc Res Technol 1998; 43(3): 265–275.
Yun Z, Smith TW, Menter DG, McIntire LV, Nicolson GL . Differential adhesion of metastatic RAW117 large-cell lymphoma cells under static or hydrodynamic conditions: role of integrin alpha(v) beta3. Clin Exp Metastasis 1997; 15(1): 3–11.
Cooper CR, McLean L, Walsh M, Taylor J, Hayasaka S, Bhatia J et al. Preferential adhesion of prostate cancer cells to bone is mediated by binding to bone marrow endothelial cells as compared to extracellular matrix components in vitro. Clin Cancer Res 2000; 6: 4839–4874.
Lehr JE, Pienta KJ . Preferential adhesion of prostate cancer cells to a human bone marrow endothelial cell line. J Natl Cancer Inst 1998; 90(2): 118–123.
Scott LJ, Clarke NW, George NJ, Shanks JH, Testa NG, Lang SH . Interactions of human prostatic epithelial cells with bone marrow endothelium: binding and invasion. Br J Cancer 2001; 84(10): 1417–1423.
Mogiri M, Zoja C, Figliuzzi M, Foppolo M, Micheletti G, Bontempe M et al. Fluid shear stress modulates surface expression of adhesion molecules by endothelial cells. Blood 1995; 85(7): 1696–1703.
Yoshida N, Yoshikawa S, Nakagawa K, Sakamoto Y, Nakamura Y, Naito Y et al. Effect of shear stress and a stable prostaglandin I2 analogue on adhesive interactions of colon cancer cells and endothelial cells. Clin Exp Immunol 1999; 117: 430–434.
Khatib A-M, Kontogiannea M, Fallavollita L, Jamison B, Meterissian S, Brodt P . Rapid induction of cytokine and E-selectin expression in the liver in response to metastatic tumor cells. Cancer Res 1999; 59: 1356–1361.
Simiantonaki N, Jayasinghe C, Kirkpatrick CJ . Effect of pro-inflammatory stimuli on tumor cell-mediated induction of endothelial cell adhesion molecules in vitro. Exp Mol Pathol 2002; 73(1): 46–53.
Wang HH, McIntosh AR, Hasinoff BB, MacNeil B, Rector E, Nance DM et al. Regulation of B16F1 melanoma cell metastasis by inducible functions of the hepatic microvasculature. Eur J Cancer 2002; 38(9): 1261–1270.
Haritopoulos KN, Lazaris AC, Kavantzas N, Tseleni-Balafouta S, Thomopoulou G, Aroni K . ICAM-1 and beta(3) integrin immunoexpression in malignant melanoma cells: can they be used as additional predictors? APMIS 2003; 111(3): 421–429.
Minami S, Furui J, Kanematsu T . Role of carcinoembryonic antigen in the progression of colon cancer cells that express carbohydrate antigen. Cancer Res 2001; 61(6): 2732–2735.
Acknowledgements
We thank Yorkshire Cancer Research and the Humane Research Trust for providing funding for this project, and Mrs Olivia Smith for assistance with flow cytometry.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Woodward, J., Rennie, I., Elshaw, S. et al. Invasive and noninvasive uveal melanomas have different adhesive properties. Eye 19, 342–348 (2005). https://doi.org/10.1038/sj.eye.6701471
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701471