Abstract
Purpose
To evaluate the efficacy of topical autologous serum application to stop aqueous oozing or point-leak through filtering bleb after trabeculectomy.
Patients and Methods
A total of 21 consecutive eyes with oozing and 21 eyes with a point-leak through a functional bleb after trabeculectomy with 5-fluorouracil or mitomycin C were enrolled in this randomized, case–control study. In eyes randomly assigned to the serum group, an antibiotic and the autologous serum, which was sterilely diluted to 20% with physiological saline, were topically applied four times a day for up to 12 weeks. In eyes assigned to the control group, the antibiotic alone was applied according to the same protocol. Intraocular pressure (IOP) and the presence of oozing or a point-leak were tested before and every 2 weeks after starting the treatments.
Results
In the serum and control groups, oozing stopped in 62.5 and 0% of eyes, respectively (P=0.003), and point-leaks stopped in 27.3 and 18.2%, respectively (P>0.9). IOP significantly increased from 10.0±3.2 (mean±standard deviation) to 11.8±3.3 mmHg in eyes in which oozing stopped (P=0.066), and from 11.4±2.7 to 15.4±2.3 mmHg in eyes in which a point-leak stopped (P=0.042).
Conclusions
Autologous serum application was significantly effective to stop aqueous oozing but not point-leaks. Stopping oozing or point-leaks was significantly associated with an increase in IOP.
Similar content being viewed by others
Introduction
The introduction of antimetabolic agents such as 5-fluorouracil (5-FU) or mitomycin C (MMC) has improved the success rate of controlling intraocular pressure (IOP) after trabeculectomy. 1, 2, 3, 4, 5, 6 However, because avascular blebs with thin walls are more commonly obtained after trabeculectomy with antimetabolites,7, 8, 9, 10 bleb-related complications, such as hypotony due to a bleb leak, blebitis, and endophthalmitis, are increasing.11, 12, 13, 14, 15
Aqueous leakage from filtering blebs is not a rare condition after trabeculectomy with antimetabolites.1, 2, 4, 10, 11, 12, 14, 16, 17 Previous studies revealed the prevalence of aqueous leakage as 1.4% after trabeculectomy with 5-FU17 and 3.7% with MMC,17 and the probability of aqueous leakage estimated with the life-table method was 4.2% at 6 years after surgery with 5-FU.18 There are two types of aqueous leakage: point-leaks and oozing: The former is leakage with a visible aqueous stream from a leak point, and the latter is transconjunctival aqueous egress without a focal leak point.10 We recently reported that the prevalence of point-leaks was 1.4% with 5-FU and 2.3% with MMC, and that of oozing was 13.8% with 5-FU and 10.9% with MMC.10 Both are possible risk factors for bleb-related complications because oozing often indicates hyperpermeability and/or vulnerability of the bleb wall.7, 8, 9, 10, 19 Several methods for repairing point-leaks have been reported, such as surgical repair,20, 21, 22, 23, 24 subconjunctival autologous blood injection,25, 26, 27 and using tissue glue or fibrin.28, 29, 30 There is no established method, however, to treat oozing.
Serum contains various cytokines or chemical mediators, such as vitamin A, epidermal growth factor, and transforming growth factor-β.31, 32, 33 Topical application of autologous serum is reported to be useful in the treatment of corneal diseases, such as severe dry eye,32 persistent corneal epithelial defect,31 and superior limbic keratoconjunctivitis.33 Although the effects of serum on the conjunctiva have not been fully studied, vitamin A and epidermal growth factor are reported to have roles in maintaining the normal histology of the conjunctiva.34, 35, 36 In the current study, the therapeutic efficacy of the topical application of autologous serum to treat aqueous leakage, including oozing and point-leaks, was prospectively evaluated in glaucoma patients who had undergone trabeculectomy with antimetabolites.
Patients and methods
In consecutive patients who had a history of trabeculectomy with 5-FU or MMC and had a functioning bleb, the presence of point-leaks or oozing of aqueous through the bleb was tested as follows, in the outpatient clinic of the Department of Ophthalmology, University of Tokyo Graduate School of Medicine (Tokyo, Japan), from February 2000 to December 2000. A moistened sterile fluorescein strip was gently applied to the bleb surface and the presence of a spontaneous visible aqueous stream from a leak point (point-leak) was initially tested under cobalt blue slitlamp illumination. If no point-leak was found, the slitlamp observation was continued for 15 s to find oozing, which was identified as aqueous egress without apparent interruption of the conjunctival tissue or an aqueous stream on the bleb wall.10
In patients in whom point-leaks or oozing were found, the purpose of the study was explained and the advantage and disadvantage of treatment were discussed. In patients who gave a written informed consent, each eye was randomly assigned into the treatment group (serum group) or control group. In patients in the serum group, 40 ml of blood was obtained from the antebrachial vein and centrifuged for 5 min at 1500 r.p.m. According to the methods of Tsubota et al,31, 32, 33 the serum was sterilely separated and diluted with physiological saline to a 20% concentration; the 20% serum solution was aliquoted into 5 ml bottles with ultraviolet light-filtering walls, since vitamin A is easily degraded by light, and patients were instructed to keep the bottles in a dark and cool place, such as a refrigerator, and to stock the rest of the bottles in a freezer until required. Both the 20% serum solution and an antibiotic (0.3% ofloxacin, Tarivid™, Santen Pharmaceutical Co. Ltd, Osaka, Japan) were topically applied with a 5-min interval into the eyes with point-leaks or oozing four times a day. In eyes of the control group, the antibiotic alone was topically applied four times a day.
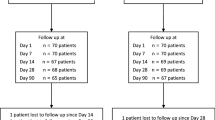
The patients were instructed to visit the outpatient clinic every 2 weeks, and a slitlamp examination was performed with testing for point-leaks or oozing at every visit by a clinician masked to the treatment. If a point-leak or oozing was not found at two consecutive visits, the treatment protocol was discontinued, but the observation was continued every 2 weeks for the at least 8 weeks to check for the recurrence of oozing or point-leaks. If point-leaks or oozing did not stop, the protocol of treatment and observation was continued for 12 weeks. IOP was measured with an applanation tonometer at every visit. None of the eyes required intervention for signs of infection (blebitis or endophthalmitis) or problems relating to hypotony (hypotony maculopathy, shallow anterior chamber, etc). The study adhered to the tenets of the Declaration of Helsinki and the research protocol was approved by an Institutional Review Board.
Results
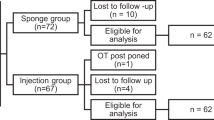
Oozing was found in 21 eyes of 21 patients and a point-leak in another 21 eyes of 21 patients. There was no patient who had oozing and/or a point-leak in both eyes. Eight and 13 of the 21 eyes with oozing, and 11 and 10 of the 21 eyes with point-leaks, were assigned to the serum and control groups, respectively. Table 1 summarizes the patients' demographics; there was no significant difference between the serum and control groups (P>0.1, χ2, Fisher exact, or Mann–Whitney tests).
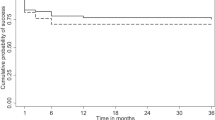
Of the 21 eyes with oozing, the oozing stopped in five of eight eyes (62.5%) in the serum group and none of 13 eyes (0%) in the control group, a statistically significant difference (P=0.003, Fisher exact test). Of the 21 eyes with point-leaks, the point-leak stopped in three of 11 eyes (27.3%) in the serum group and two of 11 (18.2%) eyes in the control group, which was not significantly different (P>0.9). The proportion in whom oozing stopped was not statistically significantly higher than the proportion in whom point-leaks stopped in the serum group (62.5 vs 27.3%) and in the control group (27.3 vs 18.2%), respectively (P=0.144, 0.178). In the current study, no case of recurrence of oozing or point-leak was observed at least 6 months after the determination of the stoppage of oozing or point-leak.
The changes in IOP associated with treatment in the eyes with oozing and point-leaks are shown in Tables 2 and 3, respectively. IOP before the treatment was IOP when oozing or point-leak was initially found. IOP after the treatments was IOP when oozing or point-leak stopped or at the end of the 12-week treatment. Among the 21 eyes with oozing, IOP increased from 10.0±3.2 to 11.8±3.3 mmHg (P=0.066, Wilcoxon signed rank test) in the five eyes in which oozing stopped, while the IOP significantly decreased from 11.0±3.3 to 9.8±3.6 mmHg (P=0.042) in the 16 eyes in which oozing continued. If the serum and control groups were separately analysed, similar tendencies were obtained (Table 2). Among the 21 eyes with point-leaks, the IOP significantly increased from 11.4±2.7 to 15.4±2.3 mmHg (P=0.042) in the 5 eyes in which point-leaks stopped, but did not significantly change (P=0.344) in the 16 eyes in which a point-leak continued. If the serum and control groups were separately analysed, similar tendencies were obtained (Table 3).
Discussion
This prospective study revealed that the topical application of autologous serum is significantly effective for stopping aqueous oozing, but not for curing point-leaks in eyes after trabeculectomy with 5-FU or MMC. The IOP significantly increased in eyes in which aqueous leakage including oozing and point-leak stopped, regardless of the treatments. No other complication was observed during autologous serum treatment.
Aqueous leakage through a filtering bleb is thought to be associated with several postoperative complications, including endophthalmitis.11, 12, 13, 14, 15 In most of the previous reports, aqueous leakage was tested with the Seidel test to find point-leaks, but oozing was usually not reported. Our recent study, however, revealed that oozing is much more frequent than point-leaks.10 Since the development of blebitis or endophthalmitis is not so frequent after trabeculectomy, it should be difficult to precisely determine the relative risks of oozing on these complications. According to Susanna et al,19 however, point-leaks could be induced with digital massage on the upper lid in 15 of 47 eyes with filtering blebs that initially showed the negative Seidel test, and the induced point-leak was much more frequently observed in eyes with a transparent, avascular bleb, suggesting that oozing, which usually occurred in blebs with avascular walls,10 may easily develop point-leaks. Moreover, as Lehmann et al.37 suggested, the physical barrier function against bacteria should be impaired in the thin and avascular bleb wall, with denuded epithelium, and in the underlying full thickness stromal damage.7 Thus, eyes with oozing should have potential risks of developing point-leak- and bleb-related infections, and a method to treat oozing should be of clinical importance.
Eyes with bleb leaks generally show lower IOP than those without it. In our previous study,10 IOPs were 11.9±3.9, 9.8±3.2, and 9.1±2.2 mmHg (mean±standard deviation) in eyes without oozing or point-leaks, those with oozing, and those with point-leaks, respectively, and the intergroup difference was significant (P<0.001, Kruskal–Wallis test). Therefore, with a view to IOP control, bleb leaks may not be necessarily an adverse condition. In the current study, the IOP increased from 10.0±3.2 to 11.8±3.3 mmHg (P=0.066) in eyes in which oozing stopped, and from 11.4±2.7 to 15.4±2.3 mmHg (P=0.042) in eyes in which point-leaks stopped, while IOP decreased or did not change in eyes in which oozing or point-leaks continued. These results suggest that not only point-leaks but also oozing is associated with keeping IOP lower. Thus, an attempt to stop oozing may not be indicated in eyes in which the target IOP is low, although continuing careful observation is necessary. Conversely, an eye with oozing and consistent low IOP may be a good indication for autologous serum application.
According to Tsubota et al,31, 32, 33 autologous serum prepared in the same manner as in the current study includes vitamin A, epidermal growth factor, and transforming factor-β1. They also reported that the migration speed of a confluent sheet of human corneal epithelial cells was significantly higher in medium containing 20% serum than in that without it.31 Although the influence of cytokines or other chemical mediators in serum on the conjunctiva is not so clear as that on the corneal tissues, several studies suggest that deficiency of vitamin A caused abnormal histology in the conjunctiva, such as decreased goblet cells and increased cellular stratification.34, 35 Also, another study found epidermal growth factor in the conjunctiva and tears of rats, but not in the cornea and aqueous humor.36 Doyle et al38 suggested that peribleb injection of transforming growth factor-β contributes to healing bleb leaks created by stab incision of the bleb in rabbits. The current result that autologous serum application was significantly effective in stopping aqueous oozing also suggests that these substances may have beneficial effects on treating hyperpermeability of thin and avascular bleb walls, in which an irregular cell arrangement of the epithelial layer and a damaged basement membrane exist.7, 8, 9, 13, 14, 15 The 20% serum application, however, is not thought to be effective enough to close a leaking micro-hole responsible for a point-leak on the bleb wall.
The topical application used in the current study was formulated from the patient's own serum in a sterile manner, and was kept in a dark and cool place, such as a freezer and a refrigerator. The concentrations of vitamin A, epidermal growth factor, and transforming growth factor-β1 in 20% serum are reported to be stably maintained for 1 month in a refrigerator or 3 months in a freezer.31 Although contamination of the serum solution was not assessed in the current study, a previous report found no bacterial or fungal positive cultures from the remaining serum prepared as in the current study and used in 12 cases with dry eyes in Sjögren's syndrome.32 No eye participating in the current study developed infectious complications, such as conjunctivitis, blepharitis, blebitis, and an endophthalmitis during or after the current study. In the current study, although the recurrence of oozing was not seen during at least 6 months follow-up in eyes in which oozing was initially stopped with or without the treatment, it is still unclear whether the effect of autologous serum application on curing oozing is long-lasting or not. Therefore, the cost (or effort) effectiveness of this regimen should not be concluded here, and deserves further clinical studies with longer follow-up periods.
In conclusion, autologous serum application was significantly effective in stopping aqueous oozing but not point-leaks after trabeculectomy with 5-FU or MMC. Stopping oozing is expected to reduce the risk of future bleb-related complications, such as hypotony, hypotony maculopathy, blebitis, and endophthalmitis. However, it also has the possibility of aggravating IOP control at least in a part of cases. An eye concurrently having oozing and hypotony or a fairly low IOP is in our view an indication for treatment with autologous serum application. If an eye without low IOP has oozing, careful observation of the bleb should be advocated rather than instantly starting the autologous serum application.
References
Rockwood EJ, Parrish II RK, Heuer DK, Skuta GL, Hodapp E, Palmberg PF et al. Glaucoma filtering surgery with 5-fluorouracil. Ophthalmology 1987; 94: 1071–1078.
The Fluorouracil Filtering Surgery Study Group. Five-year follow-up of the Fluorouracil Filtering Surgery Study. Am J Ophthalmol 1996; 121: 349–366.
Kitazawa Y, Kawase K, Matsushita H, Minobe M . Trabeculectomy with mitomycin. A comparative study with fluorouracil. Arch Ophthalmol 1991; 109: 1693–1698.
Liebmann JM, Ritch R, Marmor M, Nunez J, Wolner B . Initial 5-fluorouracil trabeculectomy in uncomplicated glaucoma. Ophthalmology 1991; 98: 1036–1041.
Araie M, Shoji N, Shirato S, Nakano Y . Postoperative subconjunctival 5-fluorouracil injections and success probability of trabeculectomy in Japanese: results of 5-year follow-up. Jpn J Ophthalmol 1992; 36: 158–168.
Cheung JC, Wright MM, Murali S, Pederson JE . Intermediate-term outcome of variable dose mitomycin C filtering surgery. Ophthalmology 1997; 104: 143–149.
Shields MB, Scroggs MW, Sloop CM, Simmons RB . Clinical and histopathologic observations concerning hypotony after trabeculectomy with adjunctive mitomycin C. Am J Ophthalmol 1993; 116: 673–683.
Mietz H, Brunner R, Addicks K . Histopathology of an avascular filtering bleb after trabeculectomy with mitomycin-C. J Glaucoma 1993; 2: 266–270.
Nuyts RM, Felten PC, Pels E, Langerhorst CT, Geijssen HC, Grossniklaus HE et al. Histopathologic effects of mitomycin C after trabeculectomy in human glaucomatous eyes with persistent hypotony. Am J Ophthalmol 1994; 118: 225–237.
Matsuo H, Tomidokoro A, Suzuki Y, Shirato S, Araie M . Late-onset transconjunctival oozing and point leak of aqueous humor from filtering bleb after trabeculectomy. Am J Ophthalmol 2002; 133: 456–462.
Wolner B, Liebmann JM, Sassani JW, Ritch R, Speaker M, Marmor M . Late bleb-related endophthalmitis after trabeculectomy with adjunctive 5-fluorouracil. Ophthalmology 1991; 98: 1053–1060.
Ticho U, Ophir A . Late complications after glaucoma filtering surgery with adjunctive 5-fluorouracil. Am J Ophthalmol 1993; 115: 506–510.
Greenfield DS, Parrish II RK . Bleb rupture following filtering surgery with mitomycin-C: clinicopathologic correlations. Ophthalmic Surg Lasers 1996; 27: 876–877.
Belyea DA, Dan JA, Stamper RL, Liebmann MF, Spencer WH . Late onset of sequential multifocal bleb leaks after glaucoma filtration surgery with 5-fluorouracil and mitomycin C. Am J Ophthalmol 1997; 124: 40–45.
Sihota R, Dada T, Gupta SD, Sharma S, Arora R, Agarwal HC . Conjunctival dysfunction and mitomycin C-induced hypotony. J Glaucoma 2000; 9: 392–397.
Katz GJ, Higginbotham EJ, Lichter PR, Skuta GL, Musch DC, Bergstrom TJ et al. Mitomycin C versus 5-fluorouracil in high-risk glaucoma filtering surgery. Extended follow-up. Ophthalmology 1995; 102: 1263–1269.
Greenfield DS, Liebmann JM, Jee J, Ritch R . Late-onset bleb leaks after glaucoma filtering surgery. Arch Ophthalmol 1998; 116: 443–447.
Uchida S, Suzuki Y, Araie M, Shigeeda T, Hara T, Shirato S . Long-term follow-up of initial 5-fluorouracil trabeculectomy in primary open-angle glaucoma in Japanese patients. J Glaucoma. 2001; 10: 458–465.
Susanna Jr R, Takahashi W, Nicolela M . Late bleb leakage after trabeculectomy with 5-fluorouracil or mitomycin C. Can J Ophthalmol 1996; 31: 296–300.
Wilson MR, Kotas-Neumann R . Free conjunctival patch for repair of persistent late bleb leak. Am J Ophthalmol 1994; 117: 569–574.
Budenz DL, Chen PP, Weaver YK . Conjunctival advancement for late-onset filtering bleb leaks: indications and outcomes. Arch Ophthalmol 1999; 117: 1014–1019.
Harris LD, Yang G, Feldman RM, Fellman RL, Starita RJ, Lynn J et al. Autologous conjunctival resurfacing of leaking filtering blebs. Ophthalmology 2000; 107: 1675–1680.
Myers JS, Yang CB, Herndon LW, Allingham RR, Shields MB . Excisional bleb revision to correct overfiltration or leakage. J Glaucoma 2000; 9: 169–173.
Wadhwani RA, Bellows AR, Hutchinson BT . Surgical repair of leaking filtering blebs. Ophthalmology 2000; 107: 1681–1687.
Smith MF, Magauran III RG, Betchkal J, Doyle JW . Treatment of postfiltration bleb leaks with autologous blood. Ophthalmology 1995; 102: 868–871.
Leen MM, Moster MR, Katz LJ, Terebuh AK, Schmidt CM, Spaeth GL . Management of overfiltering and leaking blebs with autologous blood injection. Arch Ophthalmol 1995; 113: 1050–1055.
Doyle JW, Smith MF, Garcia JA, Schultz G, Sherwood MB . Injection of autologous blood for bleb leaks in New Zealand white rabbits. Invest Ophthalmol Vis Sci 1996; 37: 2356–2361.
Zalta AH, Wieder RH . Closure of leaking filtering blebs with cyanoacrylate tissue adhesive. Br J Ophthalmol 1991; 75: 170–173.
Asrani SG, Wilensky JT . Management of bleb leaks after glaucoma filtering surgery. Use of autologous fibrin tissue glue as an alternative. Ophthalmology 1996; 103: 294–298.
Wright MM, Brown EA, Maxwell K, Cameron JD, Walsh AW . Laser-cured fibrinogen glue to repair bleb leaks in rabbits. Arch Ophthalmol 1998; 116: 199–202.
Tsubota K, Goto E, Shimmura S, Shimazaki J . Treatment of persistent corneal epithelial defect by autologous serum application. Ophthalmology 1999; 106: 1984–1989.
Tsubota K, Goto E, Fujita H, Ono M, Inoue H, Saito I et al. Treatment of dry eye by autologous serum application in Sjogren's syndrome. Br J Ophthalmol 1999; 83: 390–395.
Goto E, Shimmura S, Shimazaki J, Tsubota K . Treatment of superior limbic keratoconjunctivitis by application of autologous serum. Cornea 2001; 20: 807–810.
Hatchell DL, Sommer A . Detection of ocular surface abnormalities in experimental vitamin A deficiency. Arch Ophthalmol 1984; 102: 1389–1393.
Huang AJ, Tseng SC, Kenyon KR . Change of paracellular permeability of ocular surface epithelium by vitamin A deficiency. Invest Ophthalmol Vis Sci 1991; 32: 633–639.
Watanabe H, Ohashi Y, Kinoshita S, Manabe R, Ohshiden K . Distribution of epidermal growth factor in rat ocular and periocular tissues. Graefes Arch Clin Exp Ophthalmol 1993; 231: 228–232.
Lehmann OJ, Bunce C, Matheson MM, Maurino V, Khaw PT, Wormald R et al. Risk factors for development of post-trabeculectomy endophthalmitis. Br J Ophthalmol 2000; 84: 1349–1353.
Doyle JW, Smith MF, Garcia JA, Schultz G, Sherwood MB . Treatment of bleb leaks with transforming growth factor-beta in the rabbit model. Invest Ophthalmol Vis Sci 1997; 38: 1630–1634.
Author information
Authors and Affiliations
Corresponding author
Additional information
None of the authors has any commercial or proprietary interest in materials described in this article.
Rights and permissions
About this article
Cite this article
Matsuo, H., Tomidokoro, A., Tomita, G. et al. Topical application of autologous serum for the treatment of late-onset aqueous oozing or point-leak through filtering bleb. Eye 19, 23–28 (2005). https://doi.org/10.1038/sj.eye.6701422
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701422
Keywords
This article is cited by
-
Subconjunctival implantation of ologen Collagen Matrix to treat ocular hypotony after filtration glaucoma surgery
Eye (2017)
-
Evaluation of filtering blebs exhibiting transconjunctival oozing using anterior segment optical coherence tomography
Graefe's Archive for Clinical and Experimental Ophthalmology (2015)
-
Surgical revision of dysfunctional filtration blebs with bleb preservation, sliding conjunctival flap and fibrin glue
Eye (2010)
-
Early bleb leak after trabeculectomy and prognosis for bleb failure
Eye (2009)
-
Sodium hyaluronate eye drops prevent late-onset bleb leakage after trabeculectomy with mitomycin C
Eye (2008)