Abstract
Purpose
To compare the efficacy and safety of brimonidine 0.2% vs unoprostone 0.15%, both added to timolol maleate 0.5% each given twice daily.
Methods
In this prospective, multi-centred, double-masked, crossover comparison, patients were randomized to one treatment group for a 6-week treatment period, and then crossed over to the opposite treatment. Measurements were performed at 0800, 1000, 1600, 1800, and 2000 h at baseline and at the end of each treatment period.
Results
In all, 33 patients entered this trial and 29 completed. The baseline trough intraocular pressure (IOP) was 23.3±2.4 and the diurnal curve IOP was 22.0±1.3 mmHg. For the brimonidine and timolol maleate treatment group, the trough IOP was 21.6±3.3 and the diurnal curve IOP was 19.8±2.1 mmHg, while the timolol and unoprostone treatment showed a trough IOP of 20.9±3.8 and a diurnal curve IOP of 19.3±2.4 mmHg. There was no significant difference between treatment groups at any time point for the diurnal curve, or in the reduction from baseline (P>0.05). Both treatments failed to statistically reduce the IOP from baseline at 1800 h. There was no difference between treatment groups regarding ocular and systemic unsolicited adverse events, but patients admitted to more dryness (P=0.02) and burning upon instillation (P<0.0001) with unoprostone by survey.
Conclusion
Brimonidine 0.2% or unoprostone 0.15% added to timolol maleate 0.5% provide similar efficacy and safety throughout the daytime diurnal curve.
Similar content being viewed by others
Introduction
Patients with primary open-angle glaucoma or ocular hypertension are typically treated with medication to reduce the intraocular pressure (IOP) to prevent the onset or progression of optic nerve damage. Over the past several decades, timolol maleate has been the most commonly used primary therapy to lower the IOP.1, 2 However, many patients need a second medication to help further reduce the IOP. Over the past several years, brimonidine 0.2% (Alphagan®, Allergan, Irvine, CA, USA) has been an important adjunctive medication added to timolol maleate. Another medication, unoprostone 0.15% (Rescula®, Novartis Ophthalmics, Basal, Switzerland), was released recently into the worldwide market and may also be used as adjunctive therapy to timolol maleate.3
Unfortunately, data are still limited that evaluate the diurnal curve efficacy of brimonidine vs unoprostone each added to timolol maleate. Stewart and associates recently evaluated brimonidine 0.2% vs unoprostone 0.15%, both given twice daily, over the diurnal curve as monotherapy.4 This study showed that, although brimonidine was more effective at peak, it lost its ocular hypertensive efficacy at the end of the daytime dosing cycle at 1800 and 2000 h.4 In contrast, unoprostone statistically maintained the mean pressure reduction throughout the dosing cycle, and was more effective than brimonidine at 1800 and 2000 h.4
The purpose of this study was to evaluate the daytime diurnal safety and efficacy with a larger number of measurements for the intraocular pressure and greater statistical power to detect a statistical difference between brimonidine 0.2% and unoprostone 0.15%, both added to timolol maleate 0.5%, each given twice daily in patients with primary open-angle glaucoma or ocular hypertension.
Materials and methods
Patients
Individuals were included in this four-centre prospective trial if they demonstrated the following criteria: 18 years of age or older; new or previous clinical diagnosis of primary open-angle glaucoma or ocular hypertension; at baseline on timolol maleate 0.5% twice daily the IOP was between 22 and 34 mmHg, inclusive in at least one eye at 0800, and the average of all baseline pressure measures (diurnal curve) was ⩾20 mmHg in the same eye (visit 2); and visual acuity was 20/200 or better in the study eye(s).
Patients were excluded from this study for any of the following exclusions: any abnormality preventing reliable applanation tonometry in study eye(s); any opacity or patient uncooperativeness that restricted adequate ocular examination in the study eye; infectious/noninfectious conjunctivitis, keratitis or uveitis in either eye; any history of allergic hypersensitivity or poor tolerance to any components of the preparations used in this trial; females of childbearing potential not using reliable means of birth control; pregnant or lactating females; any serious medical or psychiatric condition; participation in any investigational drug or device trial within the previous 30 days prior to visit 1; intraocular conventional or laser surgery within the 3 months prior to visit 1; according to the investigator's best judgement risk of visual field or visual acuity worsening as a consequence of participation in the trial; inability to understand the trial procedures; any anticipated change in systemic hypotensive therapy during the active treatment portion of the trial (visits 2–6); and history of monoamine oxidase use; and bronchial asthma, history of bronchial asthma, severe chronic obstructive pulmonary disease, sinus bradycardia, second- or third-degree atrioventricular block, or overt cardiac failure.
Procedures
Before any procedures were performed, the patients signed an Institutional Review Board approved informed consent form. At the screening visit (visit 1, day −28), and, at each subsequent visit, patients had slit-lamp biomicroscopy, Early Diabetic Treatment Retinopathy Study (ETDRS) visual acuity, and Goldmann applanation tonometry performed. At visit 1, patients had the inclusion and exclusion criteria reviewed, medical history obtained, and gonioscopy, dilated funduscopy, and a visual field (Program 24-2, Humphrey Visual Field Analyzer, Humphrey Instruments, Dublin, CA, USA) performed.
Qualified patients were placed on timolol 0.5% solution twice daily for 28 days and asked to return for the baseline visit (visit 2, day 0). At this visit and at each subsequent visit, unsolicited adverse events were recorded. Also, at visit 2, as well at the other efficacy visits (visits 4 and 6), an ocular symptom query (dry eye, pain in or around eyes, blurred vision, tearing, stinging or burning, crusting, itching, sandy or gritty feeling, or irritation), a systemic symptom survey (fatigue, dizziness, despondency, depression, or dry mouth), and a diurnal curve of the intraocular pressure at 0800, 1000, 1600, 1800, and 2000 h were performed. Following the trough pressure at the baseline and efficacy visits, patients had study medicines instilled by an unmasked dosing coordinator (who performed no other procedures) before the remainder of the diurnal curve was completed.
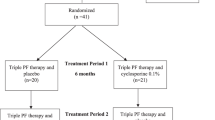
Patients who met the intraocular pressure requirements described above were randomized into the trial. Patients received either the brimonidine 0.2% and timolol maleate 0.5% to be instilled twice daily at 0800 and 2000 h, or timolol maleate 0.5% and unoprostone 0.15% to be instilled twice daily at 0800 and 2000 h with 5 min separating drop instillations. The patient, physician, and study personnel (apart from the unmasked dosing coordinator) were masked to the medicines.
Patients returned for the Period 1 safety check (visit 3, week 2) and then returned for the Period 1 efficacy visit (visit 4, week 6). Patients were then placed on the opposite treatment and returned for the Period 2 safety check (visit 5, week 8) and for the Period 2 efficacy visit (visit 6, week 12) performed the same way as visit 4.
Statistics
Data analyses were two-sided and a 0.05 alpha level was used. The primary efficacy variable was the IOP difference at Hour 0 between visits 4 and 6. This was analysed by a paired t-test for intragroup analysis.5 The standard deviation used to determine the power was 2.8 mmHg.6, 7, 8, 9 This study provided with 27 patients at least an 80% power that a 1.5 mmHg difference could be excluded between groups. The secondary efficacy variable, intraocular pressure at each time point as well as diurnal IOP (the average of the five individual time points), was also analysed by a paired t-test.5
Safety parameters for intragroup analysis were evaluated with the Wilcoxon sign rank test including the ocular and systemic symptom queries.5 Visual acuity was analysed by a paired t-test.5 Adverse events were evaluated with a McNemar test.10
Results
Patients
In all, 33 patients were enrolled, who met the inclusion and exclusion criteria. Of these, 29 patients completed the study. The average age was 61.0±11.0 years. Of these patients, 21 were Caucasian and eight were African American; 13 were male and 16 were female. A total of 20 patients had primary open-angle glaucoma and nine had ocular hypertension.
Intraocular pressure
The individual IOP and diurnal curves are shown in Table 1 and in diagrammatical form in Figure 1. The baseline trough pressure was 23.3±2.4 and the baseline diurnal curve was 22.0±1.3 mmHg on timolol alone. This study found that both study treatments caused a significant reduction for the diurnal curve, from baseline and at each time point (P>0.05), except at 1800 h following dosing (P>0.05).
The brimonidine and timolol maleate therapy showed a trough IOP of 21.6±3.3 mmHg and a diurnal curve of 19.8±2.1 mmHg. In contrast, timolol maleate and unoprostone showed a trough IOP of 20.9±3.8 mmHg (P=0.49) and a diurnal curve pressure of 19.3±2.4 mmHg (P=0.45). There was no difference between treatment groups at any time point in the absolute pressure value or in the reduction of the IOP from baseline (P>0.05) (Table 1).
Adverse events
Ocular adverse events are shown in Table 2 and systemic adverse events in Table 3 . There was no significant difference for any individual adverse event between the two treatments evaluated in this trial. The most frequent ocular adverse events were burning and conjunctival hyperaemia. There were no significant differences in systemic adverse events between the two treatment groups (P>0.05). There were no serious adverse events.
On the systemic query, no significant difference existed between groups for any solicited systemic adverse event. However, on the ocular symptom survey, more patients reported dryness (n=7) with unoprostone than brimonidine (n=1, P=0.02). Also, a greater number of patients indicated more stinging upon instillation with unoprostone (n=26) than brimonidine (n=8, P<0.001). No difference in visual acuity was observed between treatment periods (P=0.93).
Discontinued patients
In all, 29 patients completed both the trough time points of the study. Two patients were excluded from data analysis because of a site administrative error. One patient was not used due to incorrect dosing and one patient was exited early from a treatment period because of dermatitis of the eyelid while on brimonidine.
Discussion
Brimonidine 0.2% was commercially released by Allergan in late 1996. It is a highly selective α2-adrenergic agonist, and reduces the IOP primarily by decreasing aqueous production. It has become a popular adjunctive agent for glaucoma and, when prescribed, it is frequently given as monotherapy. It reduces the IOP at the 0800 trough level approximately 15–16% from baseline.11, 12, 13, 14 It is labelled three times a day, but is most frequently dosed twice daily. Brimonidine may cause side effects, including ocular allergy with an incidence approximately 10% presenting 3 months or later after initiation of therapy.15 Also, systemic side effects of dry mouth, fatigue, and blood pressure changes may occur.16, 17
Unoprostone 0.15% was released onto the commercial market in October 2000. This medicine demonstrates the structural characteristics of an F2α prostaglandin, but may not be active at the FP-receptor in humans (internal data, Novartis Ophthalmics). It is labelled as a docosanoid by the United States regulatory agency. Unoprostone reduces the IOP by increasing outflow.17 However, the exact pathway by which it acts, uveoscleral or conventional, has not yet been clarified.
Regulatory trials in the United States and Europe have shown that unoprostone reduces the IOP from baseline between 14 and 19%, with a consistent pressure reduction maintained over the 12-h daytime diurnal curve (internal data, Novartis Ophthalmics).18 However, in these studies, unoprostone was not as effective statistically in reducing the IOP as timolol maleate. In addition, several reports have recently shown that latanoprost reduces the IOP statistically more than unoprostone.19, 20 Ocular stinging upon instillation is the most common side effect.21
This current report evaluated brimonidine 0.2% and timolol maleate 0.5% therapy given twice daily vs concomitant timolol maleate 0.5% and unoprostone 0.15%, each given twice daily in patients with primary open-angle glaucoma or ocular hypertension.
This study found that both treatments caused a significant reduction at each time point and for the diurnal curve from baseline, except at 1800 h after dosing. The reason why both medications did not reduce IOP at 1800 h after dosing, but at each other time point including 2000 h after dosing, is not clear from the results.
For brimonidine, the results at the end of the dosing cycle were consistent with several past studies. In two separate diurnal curve studies, Stewart and coworkers4 showed no effect from brimonidine as monotherapy when given twice daily at 1800 and 2000 h.4 Stewart and associates also noted, in contrast, that a small effect was shown at both time points when brimonidine was added to timolol maleate (1.0 mmHg decrease).22
Unoprostone typically demonstrates a 12-h effect with twice daily dosing, and does not typically demonstrated a peak effect.21, 23 In a previous study (mentioned above), the effect of unoprostone monotherapy at peak was shown to be less than that of brimonidine (1200 h after dosing).4 In contrast, unoprostone maintained a reduced pressure effect for the 12-h daytime dosing cycle. In this current study, an ocular hypotensive effect was seen throughout the dosing cycle, except at 1800 h when unoprostone was added to timolol. The reason for the lack of effect at 1800 h in this trial is not clear.
When the two treatment groups were compared, there was no significant difference in the IOP between treatments at each time point and for the diurnal curve of the pressure. Timolol and unoprostone showed a slight trend to be better at morning trough, whereas brimonidine and timolol showed a tendency to be better 8 h after dosing. In addition, there was no significant difference between treatments at each time point for the amount of reduction of the IOP.
Both brimonidine and unoprostone statistically reduced the IOP compared to timolol alone, but only by approximately 2 mmHg. This is less than that observed with the addition of latanoprost compared to timolol alone, and slightly more than that observed with the dorzolamide/timolol fixed combination compared to timolol alone (1.2 mmHg).24, 25, 26, 27 The results of this study are similar, but slightly less, to those of Hommer and associates,28 in which approximately a 3 mmHg further reduction was found when adding brimonidine or unoprostone to timolol. The reason for the differences in the extent of the reduction between the current trial and Hommer's study is not readily apparent.
Safety results were similar between treatment results. The most common ocular adverse events were conjunctival hyperaemia and ocular stinging upon instillation, for which there was no significant difference between treatments. Stinging has been noted previously with unoprostone.21, 23 On the solicited ocular symptom survey, stinging upon instillation and dryness was noted more commonly with unoprostone. No differences in unsolicited or solicited systemic events were noted. There were no serious adverse events in this trial.
This study suggests that brimonidine 0.2% or unoprostone each added to timolol maleate 0.5% provide similar efficacy and safety throughout the daytime diurnal curve.
This study did not evaluate other types of glaucoma or nighttime IOPs with these medications. In addition, the study did not evaluate the efficacy of brimonidine vs unoprostone dosed per label (three times daily for brimonidine). Further research may help clarify any important medical differences between brimonidine and unoprostone as monotherapy or adjunctive therapy.
References
Stewart WC . Clinical Practice of Glaucoma. SLACK Inc.: Thorofare, 1990, pp 149–183.
Shields MB . Textbook of Glaucoma, 2nd ed. Williams & Wilkins: Baltimore, 1987, pp 449–455, 466–469.
Day DG, Schacknow PN, Wand M, Sharpe ED, Stewart JA, Leech J et al. Timolol 0.5%/dorzolamide 2% fixed combination versus timolol maleate 0.5% and unoprostone 0.15% given twice daily to patients with primary open-angle glaucoma or ocular hypertension. Am J Ophthalmol 2003; 135: 138–143.
Stewart WC, Stewart JA, Day DG, Leech J . The safety and efficacy of unoprostone 0.15% vs brimonidine 0.2%. Acta Opthalmol Scand 2004; in press.
Book SA . Essentials of Statistics. McGraw Hill Book Company: New York, 1978, pp 117–122, 205–215.
Mundorf TK, Cate EA, Sine CS, Otero DW, Stewart JA, Stewart WC . The safety and efficacy of switching timolol maleate 0.5% solution to timolol hemihydrate 0.5% solution given twice daily. J Ocul Pharmacol Ther 1998; 14: 129–135.
Duff GR . A double-masked crossover study comparing the effects of carteolol 1% and 2% on intraocular pressure. Acta Ophthalmol 1987; 65: 618–621.
Konstas AGP, Lake S, Maltezos AC, Holmes KT, Stewart WC . 24 hour intraocular pressure reduction with latanoprost compared to pilocarpine as third line therapy in exfoliation glaucoma. Eye 2001; 15: 59–62.
Stewart WC, Day DG, Stewart JA, Schuhr J, Latham KE . The efficacy and safety of latanoprost 0.005% once daily versus brimonidine 0.2% twice daily in open-angle glaucoma or ocular hypertension. Am J Ophthalmol 2001; 131: 631–635.
Siegel S . Nonparametric Statistics for the Behavioral Sciences. McGraw Hill Book Company: New York, 1956, pp 63–67.
Katz LJ . The Brimonidine Study Group. Brimonidine tartrate 0.2% twice daily vs timolol 0.5% twice daily: 1-year results in glaucoma patients. Am J Ophthalmol 1999; 127: 20–26.
Schuman JS . Clinical experience with brimonidine 0.2% and timolol 0.5% in glaucoma and ocular hypertension. Surv Ophthalmol 1996; 41: S27–S37.
Walters TR . Development and use of brimonidine in treating acute and chronic elevations of intraocular pressure: a review of safety, efficacy, dose response, and dosing studies. Surv Ophthalmol 1996; 41: S19–S26.
LeBlanc RP . Twelve-month results of an ongoing randomized trial comparing brimonidine tartrate 0.2% and timolol 0.5% given twice daily in patients with glaucoma or ocular hypertension. Brimonidine Study Group 2. Ophthalmology 1998; 105: 1960–1967.
Stewart WC . New perspectives in the medical treatment of glaucoma. Curr Opin 1999; 127: 142–147.
Hutzelmann J, Owens S, Shedden A, Adamsons I, Vargas E . Comparison of the safety and efficacy of the fixed combination of dorzolamide/timolol and the concomitant administration of dorzolamide and timolol: a clinical equivalence study. International Clinical Equivalence Study Group. Br J Ophthalmol 1998; 82: 1249–1253.
Sakurai M, Araie M, Oshika T, Mori M, Masuda K, Ueno R et al. Effects of topical application of UF-021, a novel prostaglandin derivative, on aqueous humor dynamics in normal human eyes. Jpn J Ophthalmol 1991; 35: 156–165.
Stewart WC, Mundorf T, Haque R, Brown A, Kapik B, Shams N . Comparison of the IOP-lowering efficacy and safety of the docosanoid unoprostone 0.15% versus timolol maleate 0.5% dosed twice daily for 6 months in patients with primary open-angle glaucoma or ocular hypertension. Invest Ophthalmol Vis Sci 2001; 42: S557.
Susanna Jr R, Giampani Jr J, Borges AS, Vessani RM, Jordao ML . A double-masked, randomized clinical trial comparing latanoprost with unoprostone in patients with open-angle glaucoma or ocular hypertension. Ophthalmology 2001; 108: 259–263.
Aung T, Chew PTK, Yip CC, Chan YH, See JLS, Khng CG et al. A randomized double-masked crossover study comparing latanoprost 0.005% with unoprostone 0.12% in patients with primary open-angle glaucoma and ocular hypertension. Am J Ophthalmol 2001; 131: 636–642.
Nordmann JP, Mertz B, Yannoulis NC, Schwenniger C, Kapik B, Shams N . A double-masked randomized comparison of the efficacy and safety of unoprostone with timolol and betaxolol in patients with primary open-angle glaucoma including pseudoexfoliation glaucoma or ocular hypertension. Six month data. Am J Ophthalmol 2002; 133: 1–10.
Stewart WC, Stewart JA, Day DG, Sharpe ED . Efficacy and safety of timolol maleat/ketanoprost fixed combination vs timolol maleate and brimonidine given twice daily. Acta Ophthalmol Scand 2003; 81: 242–246.
Stewart WC, Stewart JA, Kapik BM . The effect of unoprostone isopropylate 0.12% vs timolol maleate 0.5% on the diurnal IOP. J Glaucoma 1998; 6: 388–397.
Higginbotham EJ, Feldman R, Stiles M, Dubiner H . Fixed Combination Investigative Group. Latanoprost and timolol combination therapy vs monotherapy: one-year randomized trial. Arch Ophthalmol 2002; 120: 915–922.
Pfeiffer N, European Latanoprost Fixed Combination Study Group. A comparison of the fixed combination of latanoprost and timolol with its individual components. Graefes Arch Clin Exp Ophthalmol 2002; 240: 893–899.
Boyle JE, Ghosh K, Gieser DK, Adamsons IA . A randomized trial comparing the dorzolamide–timolol combination given twice daily to monotherapy with timolol and dorzolamide. Dorzolamide–Timolol Study Group. Ophthalmology 1998; 105: 1945–1951.
Clineschmidt CM, Williams RD, Snyder E, Adamsons IA . A randomized trial in patients inadequately controlled with timolol alone comparing the dorzolamide–timolol combination to monotherapy with timolol or dorzolamide. Dorzolamide–Timolol Combination Study Group. Ophthalmology 1998; 105: 1952–1959.
Hommer A, Kapik B, Shams N . The Unoprostone Adjunctive Therapy Study Group. Unoprostone as adjunctive therapy to timolol: a double masked randomised study versus brimonidine and dorzolamide. Br J Ophthalmol 2003; 87: 592–598.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was supported by Novartis Ophthalmics, Atlanta, GA, USA.
Rights and permissions
About this article
Cite this article
Sharpe, E., Henry, C., Mundorf, T. et al. Brimonidine 0.2% vs unoprostone 0.15% both added to timolol maleate 0.5% given twice daily to patients with primary open-angle glaucoma or ocular hypertension. Eye 19, 35–40 (2005). https://doi.org/10.1038/sj.eye.6701392
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6701392