Abstract
Purpose To re-assess the value of argon laser treatment for macular oedema in ischaemic branch retinal vein occlusion (I-BRVO).
Methods Case series consisting of three patients with macular oedema following I-BRVO. Three patients were studied including two patients where ischaemia extended to include the foveal avascular zone (FAZ), with additional retinal neovascularisation in one of these. Heavy, overlapping areas of treatment were applied to the ischaemic retina up to 500 microns from the fovea.
Results All cases in the series benefited from significantly improved visual acuity. In one case laser was given several years after the initial retinal vasculopathy.
Conclusions Argon laser treatment may improve visual acuity in I-BRVO even with severe ischaemia extending into the FAZ. Treatment intensity must be sufficient to destroy ischaemic retina. Visual benefit may last for several years, and treatment can be undertaken several years after I-BRVO. The benefit to visual acuity of argon laser treatment in I-BRVO needs to be re-assessed in a prospective study.
Similar content being viewed by others
Main
Branch retinal vein occlusion (BRVO) is a common ophthalmic disease, but the management of some aspects of the condition has yet to be adequately documented.1,2,3 Macular oedema is the major cause of vision loss in these patients and it is still unclear when or indeed if argon laser treatment should be used to improve visual acuity when BRVO is associated with ischaemia (I-BRVO).2,3,4 Some I-BRVO patients benefit from treatment, but important aspects of the treatment regimen remain unclear such as which patients to treat, when to treat, and how much treatment is needed.
We present three cases of I-BRVO that may suggest answers to some of these questions. In each case, blue-green argon laser was applied using an area centralis lens. Laser spot sizes of 100–200 μm, for 0.1–0.2 ms and power ranging from 100 to 200 mW were used in a dense grid pattern. This was applied to the ischaemic area as defined by fluorescein angiography. No laser spots were applied closer than 500 μm to the fovea.
Case report
Case 1
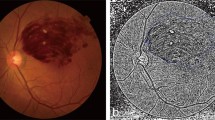
In 1994, a 59-year-old female patient had suffered an I-BRVO secondary to hypertension and hypercholesterolaemia. After 7 years, visual acuity was still poor at 6/36 and fluorescein angiography revealed marked retinal ischaemia extending into the foveal avascular zone and recent retinal neovascularisation in the upper temporal quadrant (Figure 1a). There was no significant vitreous haemorrhage. Upper temporal sector argon laser photocoagulation was recommended and undertaken.
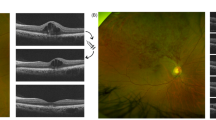
Early venous phase fluorescein angiography of the macula in cases of I-BRVO. (a) Case 1, right eye showing upper temporal ischaemia extending into the foveal avascular zone (arrow); (b) Case 2, right eye showing marked upper temporal ischaemia extending up to but not including the foveal avascular zone that, however, appears enlarged and irregular; (c) Case 3, left eye, intense upper temporal ischaemia extending into the foveal avascular zone (arrow).
After 4 months, there had been significant regression of pre-retinal neovascularisation and, remarkably, there had been marked improvement in acuity to 6/9. This improved acuity was still evident 1 year later.
Case 2
A 45-year-old, female, non-insulin dependent diabetic suffered an I-BRVO reducing acuity to 6/60 (Figure 1b). After 4 months, acuity remained poor and so argon laser photocoagulation was recommended and undertaken in the ischaemic sector.
After 1 month, visual acuity had improved to 6/9 and this improvement was still evident 15 months later.
Case 3
A 64-year-old male, hypertensive patient presented with an I-BRVO and an acuity of 6/24 (Figure 1c). This poor vision was still evident at 4 months and laser treatment recommended. Laser spot sizes of 100 μm, for 0.1 ms and power ranging from 100 to 140 mW were used in a sparse grid pattern. Approximately 40 burns only were applied to a small area of ischaemic retina superotemporal to the fovea. This had no effect on acuity and a further 8 months later, argon laser photocoagulation was undertaken to a larger area of the ischaemia following the revised protocol given above. After 2 months, visual acuity had improved to 6/9 and this beneficial response was still evident 6 months later.
Comment
It has been suggested that argon laser only be used to treat macular oedema caused by I-BRVO if the foveal avascular zone is still intact.2,3,4,5 It has also been suggested that even in I-BRVO patients with intact foveal avascular zones, improvement with treatment may not be significantly different from that seen in the natural history of I-BRVO patients as a group.6,7,8
Clearly, the patients in this study benefited from treatment, most remarkably Cases 1 and 3 where ischaemia extended into the foveal avascular zone. When comparing these results with previous studies, it is noteworthy that in each case, the grid laser treatment applied was more intense than Branch Vein Occlusion Study Group2 recommendations. This might explain why Patient 3 did not respond to initial laser treatment but benefited with marked acuity improvement when more intensive treatment was applied. Such treatment may be effective by more efficiently removing ischaemic retinal tissue and so more significantly reducing hypoxia. It has been proposed that by reducing hypoxia, a relative increase in inner retinal oxygen tension can lead to vasoconstriction and reduced hydrostatic pressure within vessels. According to Starling's law, there would then be a relative influx of extracellular fluid into the vessels reducing macular oedema.9 Although such treatment could lead to clinically significant scotoma, this is probably outweighed by the advantage of improved foveal acuity.10 It was also particularly surprising to see visual improvement in Case 1 after 7 years and this suggests that outer retinal cells at the fovea may be able to survive local ischaemia for several years.
These cases therefore suggest that argon laser treatment may improve visual acuity in I-BRVO even with severe ischaemia extending into the foveal avascular zone, if treatment intensity is enough to destroy ischaemic retina. This therapeutic benefit may be achievable for several years. It is clear, however, that a large prospective study is needed to specifically reinvestigate the visual functional benefits of laser therapy in I-BRVO.
References
Keenan JM, Kritzinger EE, Dodson PM . Management of retinal vein occlusion. Br J Hosp Med 1993; 49: 268–273.
The Branch Vein Occlusion Study Group. Argon laser photocoagulation for macular edema in branch vein occlusion. Am J Ophthalmol 1984; 98: 271–282.
Branch Vein Occlusion Study Group. Argon laser scatter photocoagulation for prevention of neovascularization and vitreous haemorrhage in branch vein occlusion. A randomized clinical trial. Arch Ophthalmol 1986; 104: 34–41.
Shilling JS, Jones CA . Retinal branch vein occlusion: a study of argon laser photocoagulation in the treatment of macular oedema. Br J Ophthalmol 1984; 68: 196–198.
The Royal College of Ophthalmologists. Proposed Guidelines for Retinal Vein Occlusion. The Royal College of Ophthalmologists, London 2002; in preparation.
Finkelstein D . Ischemic macular edema. Recognition and favorable natural history in branch vein occlusion. Arch Ophthalmol 1992; 110: 1427–1434.
Hayreh SS, Rubenstein L, Podhajsky P . Argon laser scatter photocoagulation in treatment of branch retinal vein occlusion. A prospective clinical trial. Ophthalmologica 1993; 206: 1–14.
Battaglia Parodi M, Saviano S, Ravalico G . Grid laser treatment in macular branch retinal vein occlusion. Graefe's Arch Clin Exp Ophthalmol 1999; 237: 1024–1027.
Arnarsson A, Stefansson E . Laser treatment and the mechanism of edema reduction in branch retinal vein occlusion. Invest Ophthalmol Vis Sci 2000; 41: 877–879.
Barbazetto IA, Schmidt-Erfurth UM . Evaluation of functional defects in branch retinal vein occlusion before and after laser treatment with scanning laser perimetry. Ophthalmology 2000; 107: 1089–1098.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Zaidi, F., Gair, E. & Gregory-Evans, K. Criteria for improving visual acuity in ischaemic branch retinal vein occlusion using argon laser. Eye 18, 316–318 (2004). https://doi.org/10.1038/sj.eye.6700610
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6700610